This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 35 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 43,843 times.
Vaginal dryness is a common complaint from women who are going through or are past menopause. It can also happen to younger women for a number of reasons. Whatever the cause, vaginal dryness can make sex uncomfortable or impossible, and can cause general discomfort throughout the day.[1] You can try to improve your vaginal dryness with products like lubricants and moisturizers, with estrogen-containing medications, and by increasing your sexual arousal before and during sexual activity.
Steps
Improving Lubrication
-
1Use lubricant for sexual activity. Astroglide, K-Y Jelly, and other water-based lubricants can help supply the moisture you need during sex. Buy these at any local pharmacy or drugstore. Use liberal amounts before and during intercourse or other sexual activity to reduce uncomfortable friction caused by dryness.[2]
- Silicone-based lubricants like Pure Pleasure, Pink, and others are also good options, but may stain your clothes if you spill some. They may not be compatible with some sex toys.
- Avoid oil-based products like mineral oil, baby oil, petroleum jelly, and Elegance Women’s Lubricant. Also avoid using hand or body lotions, which can increase irritation and dryness.[3]
- Try using jojoba oil, coconut oil, olive oil, or aloe if you prefer natural products.
-
2Get a vaginal moisturizer at your local drug store. If you want to skip the hormones, use a simple vaginal moisturizer. Brands like Fresh Start, Replens, and Lubrin should be readily available at your grocery store or pharmacy. Moisturizers are different from lubricants – lubricants are used only right before and during sex, whereas vaginal moisturizers can be used all the time for help with continuous discomfort caused by vaginal dryness.[4]
- Make sure the product you buy is estrogen-free, fragrance-free, tasteless, and can be used with barrier methods of birth control (generally, condoms), if needed.
- Use it once every 2-3 days.[5]
-
3Increase your sexual arousal. For some, vaginal dryness is a result of trying to have sex without being properly aroused. As you become sexually aroused, blood rushes to your genitals and your body starts to make its own vaginal lubricant.[6] Try some ways to amp up your arousal, and if you continue to have problems consider discussing it with your doctor, a counselor, or a sex therapist.
- Take your time before having sex – spend more time on foreplay. Caressing, kissing, massage, manual stimulation, and oral sex can help your body feel ready for intercourse.
- Use toys like a vibrator to increase sexual pleasure. Many women need clitoral stimulation to become aroused and climax.[7]
- Try masturbation so you know what feels good to you, then share that information with your partner.
- De-stress! Many women struggle with arousal because of psychological reasons. Consider doing something soothing before sex like taking a warm bath or a walk.[8]
Making Lifestyle Changes
-
1Avoid douching and using personal hygiene sprays. Douches and feminine sprays are marketed towards women as products that promote cleanliness. The vagina, however, is a self-cleaning part of your body. Stay away from these types of products if you have vaginal dryness, as they can worsen the problem.[9]
- Plain warm water is enough to clean your vagina. Don’t use soap or other cleansers on the outside or inside of your vagina.[10]
-
2Stick to plain, fragrance-free products. Bubble bath, scented soaps and lotions, and laundry detergent can all worsen dryness because they contain harsh chemicals. Use plain, unscented products whenever possible. Try natural laundry detergent, and skip using dryer sheets.[11]
-
3Be cautious of hot tubs and swimming pools. Public swimming areas contain high amounts of chlorine, which is very drying to your skin. Avoid spending a lot of time in pools and hot tubs, or at least rinse your vagina well with cool, plain water afterwards.[12]
-
4
-
5Exercise regularly. Get regular exercise to help keep your hormones in balance. Aerobic workouts are those that increase your heart rate and breathing rate. Walking, slow jogging, biking, and swimming are good options. Aim to get at least 30 minutes of aerobic activity at least 5 days per week.[15]
-
6Eat good fats and soy. Omega-3 fatty acids and products like flaxseed oil and soy have estrogen-like qualities, which may help improve vaginal dryness.[16] Eat fatty fish like salmon or mackerel several times per week, and incorporate soy products into your diet.
- You can also try taking oral probiotics to improve vaginal health. Find these as capsules at your pharmacy, or eat yogurt with live cultures.[17]
-
7Quit smoking. Nicotine dependence can cause or worsen vaginal dryness. Stop smoking now to help improve your symptoms.[18]
-
8Stop taking medications that worsen the condition. Some antidepressants, cold medicine, and allergy pills can dry out mucous membranes – including the sensitive skin in your vagina.[19] Make a list of your medications to take to your doctor. Discuss whether any of your medicines might be worsening your problem, and whether you can switch to a different medication.
- Never stop taking your medicine without your doctor’s supervision.
Managing Dryness Due to Low Estrogen
-
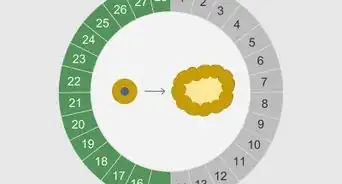
1Discuss risk factors with your doctor. Your body’s level of estrogen drops significantly during and after menopause, stopping your periods and causing vaginal atrophy – drying and thinning of the walls of your vagina. Thus, the most common way to improve vaginal dryness is by replacing lost estrogen. Using estrogen may not be safe for some women, however. Discuss your issue with your doctor or OB/GYN so they can ask you your health history and do an exam.[20]
-
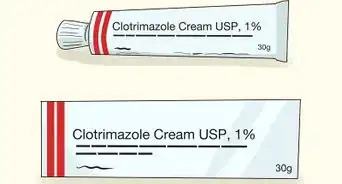
2Use an estrogen cream. Replace estrogen locally by using an estrogen cream like Estrace or Premarin. Insert the cream into your vagina with an applicator. Use it every day for 1-2 weeks, then 1-3 times per week – or however your doctor suggests you use it.[26]
- Estrogen also comes in tablet form, like Vagifem. Insert the tablet into your vagina with an applicator daily for 2 weeks, then twice a week thereafter for as long as you need it.
- Vaginal estrogen is considered safe for long-term use.[27]
-
3Try the estrogen ring. If you don’t want to use the cream, there are other options. Try an estrogen ring like Estring – a flexible ring that you insert into your vagina that releases estrogen to the local tissues. If inserting it is challenging, ask your doctor to do it for you. The ring only needs to be changed every 3 months.[28] [29]
-
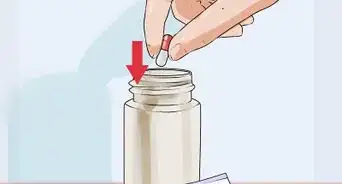
4Try Prasterone. Prasterone, or dehydroepiandrosterone (DHEA), is a non-estrogen vaginal suppository. Insert the capsule into your vagina daily. This can be a good option if you want to use local vaginal therapy but want to avoid estrogen.[32]
-
5Ask about a prescription for ospemifene. The medication ospemifene (Osphena) isn’t estrogen, but it’s similar to it and it acts similarly in your vagina. This pill can help improve vaginal dryness.[33] [34]
- You may have hot flashes as a side effect.
- This medication can increase your risk for blood clots or cancer of the uterus, and you shouldn’t use it if you have or have ever had breast cancer. Talk to your doctor about the risks and benefits of taking this medication.
-
6Consider hormone replacement therapy (HRT). HRT involves taking estrogen supplements by mouth so that the level of estrogen in your whole body increases, not just in and around your vagina. This can be helpful if you have severe symptoms of menopause like hot flashes. However, it’s more likely to cause side effects and can increase your risk for some cancers.[35]
- HRT is available as a prescription in pill form, as well as a patch, an under-the-skin implant, or a gel you put on your skin.
- Weigh the risks and benefits of HRT with your doctor.
Warnings
- Stop using a product right away if it causes burning, stinging, itching, or discomfort.⧼thumbs_response⧽
- If you try lubricants and moisturizers and still experience discomfort from vaginal dryness, see your doctor.⧼thumbs_response⧽
References
- ↑ https://www.nhs.uk/conditions/vaginal-dryness/
- ↑ https://www.uhn.ca/PatientsFamilies/Health_Information/Health_Topics/Documents/Know_How_to_Use_Vaginal_Moisturizers_Lubricants.pdf
- ↑ https://my.clevelandclinic.org/health/symptoms/21027-vaginal-dryness
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4819835/
- ↑ http://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-sex-after-menopause/
- ↑ https://www.sciencedirect.com/topics/medicine-and-dentistry/vaginal-lubrication
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3894744/
- ↑ https://www.apa.org/topics/stress/body
- ↑ https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/diagnosis-treatment/drc-20352294
- ↑ https://bloom-obgyn.com/vaginal-hygiene-dos-and-donts/
- ↑ https://www.slucare.edu/ob-gyn/female-pelvic-medicine-and-reconstructive-surgery/guidelines-for-vulvar-skin-care.php
- ↑ https://www.breastcancer.org/treatment-side-effects/menopause/treating-symptoms/vaginal-changes/prevention-self-care
- ↑ https://www.ruh.nhs.uk/patients/patient_information/BRU028_Vaginal_dryness_and_breast_cancer.pdf
- ↑ https://www.ucsfhealth.org/medical-tests/urine-24-hour-volume
- ↑ https://www.nhs.uk/live-well/sexual-health/keeping-your-vagina-clean-and-healthy/
- ↑ https://www.aafp.org/afp/2016/1201/p884.html
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2662373/
- ↑ https://ufhealth.org/vaginal-dryness
- ↑ https://www.morelandobgyn.com/blog/vaginal-dryness-causes-treatments
- ↑ https://www.mayoclinic.org/diseases-conditions/menopause/in-depth/hormone-therapy/art-20046372
- ↑ https://www.uofmhealth.org/health-library/tn9713
- ↑ https://www.cancer.org/cancer/breast-cancer/treatment/hormone-therapy-for-breast-cancer.html#:~:text=Chemotherapy%20drugs%3A%20Some%20chemo%20drugs,permanent%20and%20leads%20to%20menopause.
- ↑ https://www.cancer.gov/about-cancer/causes-prevention/risk/hormones
- ↑ https://www.mayoclinic.org/diseases-conditions/endometrial-cancer/symptoms-causes/syc-20352461
- ↑ https://www.aafp.org/afp/1999/1001/p1371.html
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3958523/
- ↑ https://www.uptodate.com/contents/vaginal-dryness-beyond-the-basics
- ↑ https://my.clevelandclinic.org/health/drugs/19191-estradiol-vaginal-ring-estring
- ↑ https://www.nhlbi.nih.gov/files/docs/pht_facts.pdf
- ↑ https://www.mayoclinic.org/drugs-supplements/estrogen-vaginal-route/precautions/drg-20069459
- ↑ https://www.tandfonline.com/doi/abs/10.3109/13697137.2014.947254
- ↑ https://www.uptodate.com/contents/vaginal-dryness-beyond-the-basics
- ↑ https://pubmed.ncbi.nlm.nih.gov/30694917/
- ↑ https://medlineplus.gov/druginfo/meds/a613039.html
- ↑ https://emedicine.medscape.com/article/276104-overview
- ↑ https://my.clevelandclinic.org/health/symptoms/21027-vaginal-dryness
- ↑ https://www.plannedparenthood.org/learn/birth-control/breastfeeding/whats-best-birth-control-option-while-breastfeeding
























-Step-10-Version-2.webp)













































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...