This article was medically reviewed by Lacy Windham, MD and by wikiHow staff writer, Jennifer Mueller, JD. Lacy Windham, MD, is a Board-Certified Obstetrician & Gynecologist in Cleveland, Tennessee. Dr. Windham attended medical school at the University of Tennessee Health Science Center in Memphis. Her residency was completed at Eastern Virginia Medical School in Norfolk, Virginia. She was the recipient of multiple awards during her residency training, including Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, Most Outstanding Resident Overall, and Special Award in Minimally Invasive Surgery.
There are 10 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 475,708 times.
When you have a problem "down there," it's easy to spiral into thinking the worst. But is that lump on your vulva potentially cancerous? Without getting a biopsy, there's no way to know for sure. The good news is that vulva cancer is really rare and it's usually pretty easily treated—especially if it's caught early. Read on to learn more about your vulva and how to spot the abnormalities that might be cancer symptoms, so you can get your doctor to look at them as soon as possible.
Things You Should Know
- Examine your vulva regularly so you'll be able to identify potential problems easily.
- Itching, pain, or bleeding that doesn't seem to have another cause and doesn't go away after a week or two could be a symptom of cancer.
- Visit your doctor as soon as possible if there's an abnormality that worries you. Treatments are more effective if you catch the problem early.
- If you're a smoker, 60-75 years old, infected with HPV or HIV, or have a family history of skin cancer, you may have a slightly higher risk of contracting vulvar cancer.
Steps
What is the vulva?
-
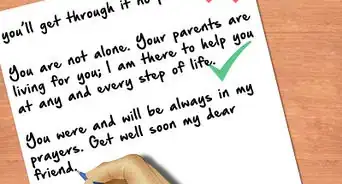
The vulva is the skin between your legs around your vagina. Often, when people talk about the "vagina," they're actually talking about the vulva. While everybody's vulva looks a little different, all vulvas are made up of the same basic parts: the inner and outer vaginal lips (labia), urethral and vaginal openings, and clitoris.[1] X Research source
- Vulvar cancer most often occurs on the outer vaginal lips (labia majora), but it can also show up on the inner lips or clitoris.[2] X Trustworthy Source National Cancer Institute An agency in the National Institutes of Health focused on cancer research and patient support Go to source
Symptoms of Vulvar Cancer
-
1Vulvar itching that doesn't go away. Itching is a common symptom of a lot of other, less serious conditions. But if you have severe itching that persists no matter what you do, make an appointment to have your doctor look at it.[3] X Trustworthy Source MedlinePlus Collection of medical information sourced from the US National Library of Medicine Go to source
-
2Unexplained pain or tenderness of the vulva. This is consistent pain or tenderness that might lessen or worsen, but never completely goes away. The pain might get worse when you have sex or go to the bathroom.[4] X Trustworthy Source National Cancer Institute An agency in the National Institutes of Health focused on cancer research and patient support Go to source
-
3Bleeding that isn't from menstruation. If you're still menstruating, make sure the bleeding isn't related to your menstrual cycle. Then, call your doctor as soon as possible—this is a more advanced symptom of vulvar cancer, as well as some other genital cancers.[5] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source
-
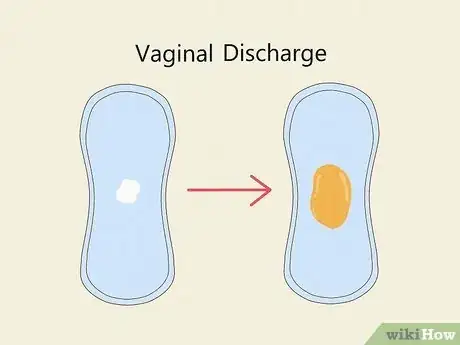
4Excessive discharge not related to your menstrual cycle. Only you know what discharge is normal for you. If your discharge changes in color, consistency, or volume and there's nothing that would explain that change, make an appointment with your doctor.[6] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source
-
5Changes in the color or thickness of the vulva. Changes to your vulvar skin are among the most common symptoms of vulvar cancer. Typically, your skin will be redder or whiter than it normally is for you. It might also have a rougher texture than normal.[7] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source
-
6A lump or open sore on or around your vulva. This could be a single lump or a group of small lumps that look similar to genital warts. If you have an open sore that doesn't heal within a few weeks to a month, that could also signal vulva cancer.[8] X Trustworthy Source National Cancer Institute An agency in the National Institutes of Health focused on cancer research and patient support Go to source
-
7Changes in an existing mole. Moles typically aren't any cause for concern, but if they change in shape or size, that could indicate the presence of cancer. Use the ABCDE rule to tell if the mole is potentially cancerous:[9] X Trustworthy Source American Cancer Society Nonprofit devoted to promoting cancer research, education, and support Go to source
- Asymmetry: one half doesn't match the other
- Border irregularity: the edges are ragged
- Color: not uniform; could include shades of tan, brown, or black or patches of red, blue, or white
- Diameter: wider than 1/4 inch (6 mm)
- Evolving: changes in size, shape, or color
-
8Pelvic pain when you urinate or have sex. This is a symptom not only of vulvar cancer but of other genital and pelvic cancers. It's also a symptom of many other conditions that aren't quite as serious as cancer, but it's still a serious symptom. Call your doctor as soon as possible and schedule an appointment so they can evaluate your situation.[10] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source
Diagnosis and Treatment
-
1Check your vulva regularly for abnormalities. It's so important to be familiar with this part of your body. Use your hands and your eyes to explore and examine your vulva. Gently feel your vulva for lumps or other irregularities. A hand mirror can help you see details more clearly. [11] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source
- Remember: there's nothing gross or shameful about knowing your own body. Many symptoms involve something that isn't normal for you—that means you need to know what is normal for you.
-
2Mention possible symptoms to your primary care doctor or gynecologist. If you have a symptom that persists for 2 weeks or longer, make an appointment to get it checked out. Describe your symptoms in detail, including how long you've had it and anything you've done to try to treat it on your own.[12] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source
- Your doctor will do a complete pelvic exam and also talk to you about your medical history. This helps them determine your risk for developing vulvar cancer.[13] X Trustworthy Source National Cancer Institute An agency in the National Institutes of Health focused on cancer research and patient support Go to source
-
3Undergo a biopsy to determine the presence of cancer. A biopsy involves your doctor cutting away a small piece of the affected vulvar tissue and looking at it under a microscope for signs of cancer. A biopsy is the only way to get a diagnosis of vulvar cancer—it's also the only way to definitively rule out cancer.[14] X Trustworthy Source FamilyDoctor.org Family-focused medical advice site run by the American Academy of Family Doctors Go to source
-
4Discuss treatment options based on your biopsy results. If your biopsy is negative for cancer, you'll likely still want to treat your symptoms. Your doctor will work with you to come up with a plan that best suits your needs.[15] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source
- Your doctor might recommend surgical removal of any lump or growth, even if it's not cancerous.
- If the biopsy reveals cancer, you'll likely have other tests to determine if the cancer has spread to other parts of your body.
Risk Factors
-
1Age Most people diagnosed with vulvar cancer are 65-75 years old. But at the same time, it can also develop in people under 40 years of age. Vulvar cancer often takes many years to develop, which is part of the reason age is a significant risk factor.[16] X Trustworthy Source FamilyDoctor.org Family-focused medical advice site run by the American Academy of Family Doctors Go to source
-
2Human papillomavirus (HPV) infection HPV is a sexually-transmitted infection (STI) that's been linked to vulvar cancer as well as cervical cancer and other genital cancers. Exposure to HPV, as well as other STIs, could increase your risk of developing vulvar cancer.[17] X Trustworthy Source National Cancer Institute An agency in the National Institutes of Health focused on cancer research and patient support Go to source
-
3HIV infection HIV weakens your immune system, which makes you more susceptible to many other infections and conditions. It can also increase your risk of developing vulvar cancer.[18] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source
-
4A family history of melanoma The most common types of vulvar cancer are skin cancers. A family history of skin cancer puts you at an increased risk of developing skin cancer yourself, including vulvar cancer. The risk is even greater if you've already had skin cancer somewhere else on your body.[19] X Research source
-
5Vulvar intraepithelial neoplasia (VIN) VIN is considered a precancerous condition, although the vast majority of people diagnosed with VIN don't ever develop vulvar cancer. Treatment for VIN significantly reduces your risk of developing vulvar cancer.[20] X Trustworthy Source American Cancer Society Nonprofit devoted to promoting cancer research, education, and support Go to source
-
6Other genital cancers or precancerous conditions If you've had abnormal Pap test results or have a family history of cervical or vaginal cancer, that might increase your risk of vulvar cancer. Vulvar cancer is also linked to the human papillomavirus (HPV), so you're considered at higher risk if you've tested positive for HPV or if you haven't been vaccinated against it.[21] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source
- Lichen sclerosus is a skin condition that makes the vulvar skin thin and itchy. About 4% of the people diagnosed with lichen sclerosus develop vulvar cancer.[22] X Research source
-
7Smoking Smoking or vaping tobacco could increase your risk of vulvar as well as other cancers. If you smoke, make a plan to quit.[23] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source
Prevention
-
1Use a condom every time you have sex. Exposure to STIs might increase your risk of developing vulvar and other genital cancers. Use condoms as barriers to protect yourself from that risk.[24] X Research source
- If you and your long-term partner want to stop using condoms with each other, make sure you both get tested for STIs first.
-
2Get the HPV vaccine if you're under 45 years of age. The HPV vaccine is approved for everyone from 12 to 45. Most people get this vaccine when they're between 12 and 14 years old, but if you missed it, you can still get it when you're older.[25] X Trustworthy Source Mayo Clinic Educational website from one of the world's leading hospitals Go to source
- Older teens and adults might need multiple rounds of the vaccine to get the same level of protection as 12-14-year-olds who take the vaccine.
-
3Have a pelvic exam yearly or as recommended by your doctor. If you have a higher risk or if you have a precancerous condition, your doctor might want to see you more frequently. Regardless, contact your doctor as soon as possible if you have symptoms that are bothering you. Remember: any cancer is easier to treat if you get to it early. The longer you wait, the more involved treatment will be.[26] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source
-
4Delay intercourse until your late teens or older. There's a correlation between having sex earlier and having sex with multiple partners and developing vulvar cancer. Part of this correlation might be due to the increased exposure to STIs. Regardless, making the decision to wait until you're older to have sex can lower your risk of developing vulvar cancer later in life.[27] X Research source
-
5Avoid risk factors you have control over. Some risk factors, like aging, you can't do anything about. But you can control your sexual activity and general health. Make good decisions that promote your health and well-being and you can help limit your risk of developing vulvar or other cancers.[28] X Trustworthy Source Centers for Disease Control and Prevention Main public health institute for the US, run by the Dept. of Health and Human Services Go to source
You Might Also Like
-Step-13.webp)


 Checking Your Lymph Nodes in Your Head, Neck, Armpit, and Groin
Checking Your Lymph Nodes in Your Head, Neck, Armpit, and Groin





-Step-8-Version-3.webp)


References
- ↑ https://www.plannedparenthood.org/learn/health-and-wellness/sexual-and-reproductive-anatomy/what-are-parts-female-sexual-anatomy
- ↑ https://www.cancer.gov/types/vulvar/patient/vulvar-treatment-pdq#_1
- ↑ https://medlineplus.gov/vulvarcancer.html
- ↑ https://www.cancer.gov/types/vulvar/patient/vulvar-treatment-pdq#_1
- ↑ https://www.cdc.gov/cancer/vagvulv/pdf/vagvulv_facts.pdf
- ↑ https://www.cdc.gov/cancer/vagvulv/pdf/vagvulv_facts.pdf
- ↑ https://www.cdc.gov/cancer/vagvulv/pdf/vagvulv_facts.pdf
- ↑ https://www.cancer.gov/types/vulvar/patient/vulvar-treatment-pdq#_1
- ↑ https://www.cancer.org/cancer/vulvar-cancer/detection-diagnosis-staging/signs-symptoms.html
- ↑ https://www.cdc.gov/cancer/vagvulv/basic_info/symptoms.htm
- ↑ https://www.cdc.gov/cancer/vagvulv/pdf/vagvulv_facts.pdf
- ↑ https://www.cdc.gov/cancer/vagvulv/basic_info/symptoms.htm
- ↑ https://www.cancer.gov/types/vulvar/patient/vulvar-treatment-pdq#_1
- ↑ https://familydoctor.org/condition/vulvar-cancer/?adfree=true
- ↑ https://www.cdc.gov/cancer/vagvulv/pdf/vagvulv_facts.pdf
- ↑ https://familydoctor.org/condition/vulvar-cancer/?adfree=true
- ↑ https://www.cancer.gov/types/vulvar/patient/vulvar-treatment-pdq#_1
- ↑ https://www.cdc.gov/cancer/vagvulv/pdf/vagvulv_facts.pdf
- ↑ https://www.cancer.net/cancer-types/vulvar-cancer/view-all
- ↑ https://www.cancer.org/cancer/vulvar-cancer/causes-risks-prevention/risk-factors.html
- ↑ https://www.cdc.gov/cancer/vagvulv/pdf/vagvulv_facts.pdf
- ↑ https://www.cancer.net/cancer-types/vulvar-cancer/view-all
- ↑ https://www.cdc.gov/cancer/vagvulv/pdf/vagvulv_facts.pdf
- ↑ https://www.cancer.net/cancer-types/vulvar-cancer/view-all
- ↑ https://www.mayoclinic.org/diseases-conditions/hpv-infection/in-depth/hpv-vaccine/art-20047292
- ↑ https://www.cdc.gov/cancer/vagvulv/pdf/vagvulv_facts.pdf
- ↑ https://www.cancer.net/cancer-types/vulvar-cancer/view-all
- ↑ https://www.cdc.gov/cancer/vagvulv/pdf/vagvulv_facts.pdf
About This Article
To recognize vulva cancer symptoms, look for unusual growths, itching, or tenderness of the vulvar skin. You might also feel some lumps or irregularities in your vulva, so make sure to gently touch in and around this area so you know what’s normal for you. Any lingering pain or burning, especially during sex or urination, should also prompt you to see a doctor. In addition to any outward signs, consider your risk factors, which include exposure to HPV, smoking, having HIV, and a history of precancerous or skin conditions of the vulva. For more tips from our Medical co-author, including how to get a diagnosis for vulvar cancer, keep reading!





























-Step-13.webp)



































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...