This article was co-authored by Roy Nattiv, MD. Dr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
There are 7 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 11,451 times.
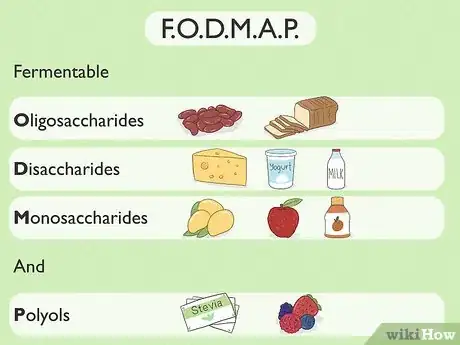
Irritable Bowel Syndrome (IBS) affects an estimated 25-45 million people in the United States,[1] and millions more worldwide. One of the most effective ways to improve IBS symptoms and determine the causes of digestive problems associated with IBS is using what is known as a low-FODMAP diet.[2] This 3-phase dieting plan can help IBS patients identify and eliminate symptom-causing foods containing FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, And Polyols). Keep reading to learn more about what FODMAPs are, why the low-FODMAP diet works, and how to follow the 3 phases of the low-FODMAP diet.
Steps
What are FODMAPs?
-
1FODMAPs are hard-to-digest carbohydrates and sugars. Instead of digesting FODMAPs quickly, the body often tries to ferment them into alcohol. This process produces methane, hydrogen, and carbon dioxide—a recipe for bloating and gas.
- FODMAPs pull water into your intestines.[3] The extra fluid gives fermenting bacteria a chance to work harder in your stomach, which can lead to gas, pain, and diarrhea.
- High-FODMAP foods have lots of bloat-inducing FODMAPS. Low-FODMAP foods are easier on the body.
-
2There are four main groups of FODMAPs. Don’t worry too much about memorizing the scientific names within the group! It may, however, be helpful for you to have a general understanding of the sorts of foods included in each one:
- Disaccharides: Anything with lactose (e.g., cheeses, yogurts, creams, dairy milks)
- Oligosaccharides: Breads, beans, and certain veggies (e.g., garlic, onion)
- Monosaccharides: Certain fruits and natural sugars (e.g., mangoes, apples, peaches, honey)
- Polyols: Sugar alcohols (e.g., artificial sweeteners) and some berries and other fruits
How do FODMAPs affect your digestion?
-
1FODMAPs are tough on your small intestine. Most FODMAP digestion happens in the small intestine, which is also where IBS symptoms generally develop. Even those with non-IBS symptoms have occasional issues digesting FODMAPs, but consistent IBS symptoms can indicate a hypersensitivity. This could be linked to three major issues:
- Your bowels may move food through your gut abnormally fast or slow.
- Your gut may be closely connected to your immune and nervous systems, making you especially sensitive to pain and bloating that happens in the gut.
- You may have a type or amount of bacteria in your gut that makes gas and bloating more likely.
-
2Portion sizes matter. Every person can tolerate a different amount of FODMAPs in their stomach. Even if you eat a food low in FODMAPs, large servings of that food (or of FODMAPS from earlier that day) can turn it into a high-FODMAP food and put your stomach at risk.
- This could explain why a particular food may trigger your IBS symptoms occasionally but not always.
Why does the low-FODMAP diet work?
-
1The low-FODMAP diet helps you learn which foods trigger your symptoms. In contrast to stricter IBS dieting plans, the goal of the low-FODMAP diet is to develop a long-term dieting plan that is less restrictive and more nutritionally balanced.[4]
- FODMAPs can actually be good for your digestive health as long as your gut can tolerate them! In addition to telling you which FODMAP foods you'll need to avoid, this diet should eventually tell you which ones you can still enjoy.
-
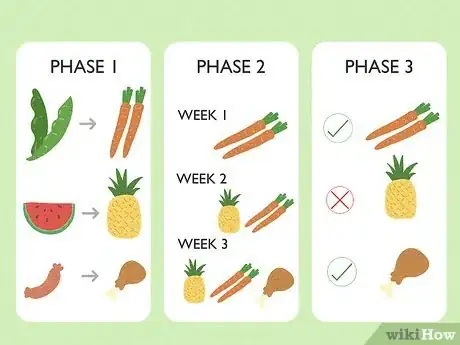
2The low-FODMAP diet has 3 phases. These phases are elimination, reintroduction, and integration. It can take several months for you to complete all 3 phases, but this approach makes it easier for you to understand your gut health and pinpoint the foods causing your symptoms.
How do I follow the 3 phases of the low-FODMAP diet?
-
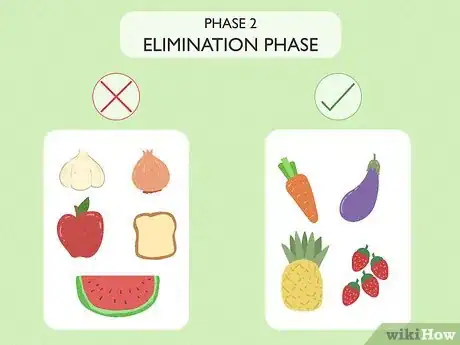
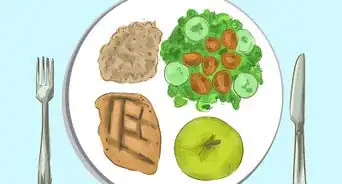
1Strictly avoid all high-FODMAP foods during the elimination phase. You should follow this phase of the diet until your symptoms improve. The exact amount of time varies, but this phase usually lasts 1-8 weeks.
- If symptoms do not improve at all after 8 weeks, you should add these high-FODMAP foods back into your diet since they can be important for your overall gut health.
-
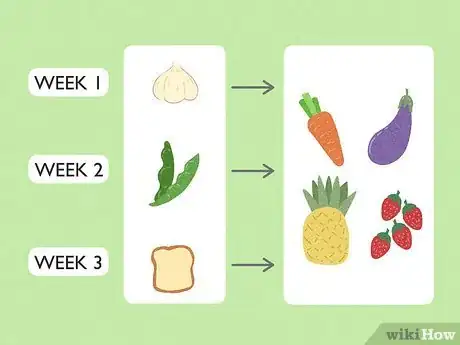
2Carefully add high-FODMAP foods back into your diet during the reintroduction phase. Add high-FODMAP foods back into your diet one at a time, giving your gut 1 to 3 days to adjust after each one. Keep track of which foods do and don't cause symptoms to reappear.
-
3Resume eating non-problem FODMAPs during the integration phase. After you’ve determined which foods you’re able to tolerate, you can begin to reintegrate them into your diet long-term. Continue avoiding foods that trigger your IBS symptoms.
- Pay attention to how much of a well-tolerated high-FODMAP food you eat in one sitting since large amounts may still trigger symptoms. The amount you're able to eat without causing symptoms is called your "threshold level."
What are some benefits of the low-FODMAP diet?
-
1The low-FODMAP diet shows quick results. Studies show that many dieters see symptoms improve within 1 week of eliminating high-FODMAP foods.[5] In other words, you could try the elimination phase for just 1 week and see how you feel! If it doesn't help at all, you don't have to commit to the diet plan any further.
-
2The low-FODMAP diet is highly successful. One 2016 report shows that over 86% of people with IBS symptoms saw their symptoms improve after following the low-FODMAP diet.[6] A 2017 analysis of other studies supported these findings: the diet successfully eased symptoms for tens of thousands of participants in the 30 studies analyzed.[7]
-
3The low-FODMAP diet can be personalized for the long-term. This diet looks at specific foods individually to determine how they contribute to your IBS symptoms. It also helps you determine how much you can eat of these foods before they cause you problems. Instead of relying on a generic dieting plan, you'll be able to follow a diet that meets your exact gastrointestinal needs.
What are some downsides of the low-FODMAP diet?
-
1High-FODMAP foods can be tasty and good for you. During the elimination phase, you might have trouble avoiding all high-FODMAP foods, especially those commonly used to season other dishes (e.g., onion and garlic). Many of these foods also provide prebiotics that feed a healthy gut; you may need to find other ways to get these prebiotics if you currently rely on high-FODMAP foods for them.
- To prevent food from tasting bland, get creative in the kitchen by swapping high-FODMAP seasonings for low-FODMAP alternatives.
-
2The diet takes a lot of time and money to complete. Even though you may notice a difference within 1 week, this diet can take 3-6 months to run its entire course due to the large number of high-FODMAP foods you'll need to gradually reintroduce. It can also be expensive to avoid high-FODMAP foods, especially in small grocery stores or when dining out.
-
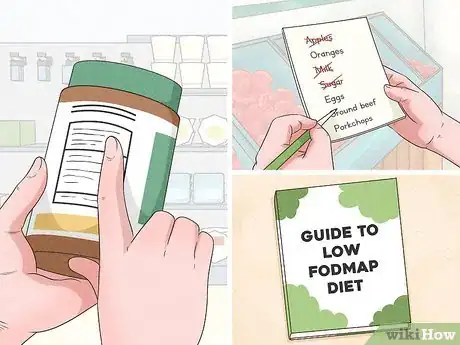
3The low-FODMAP diet requires a big commitment. High-FODMAP foods are common, so the elimination phase of the diet can be quite challenging. You'll need to check food labels, make shopping lists in advance, and map out your recipes ahead of time.
Should I start the low-FODMAP diet?
-
1Do you have consistent IBS symptoms? You should only begin the low-FODMAP diet if you regularly exhibit IBS symptoms for 6 months or more. Possible IBS symptoms include:
- Persistent abdominal cramping or stomach pain (at least once a week)
- Consistent changes in bowel movements (e.g., constipation, diarrhea, or mucus in stool)
-
2Have simpler changes failed to work? There are some simpler diet and lifestyle changes that might be enough to manage your IBS symptoms. If they're not enough, you can still try the low-FODMAP diet after trying them. A few useful options include:
- Establishing a regular meal pattern with small portion sizes
- Reducing your intake of alcohol, caffeine, and spicy foods
- Exercising regularly
-
3Are you ready to make the commitment? It’s important to make sure you have time and space to commit to the diet. Since stress can make IBS worse, you'll also need to manage any stressful situations that arise while you're on the diet to maximize your odds of success.
- Try not to be too intimidated by the restrictions. Even though getting rid of FODMAPs may require you to cut out some of your favorite ingredients and foods, there are plenty of ways to eat delicious meals while on this diet.
Expert Q&A
-
QuestionWhat is a low-FODMAP diet?
 Roy Nattiv, MDDr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
Roy Nattiv, MDDr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
Board Certified Gastroenterologist FODMAPs are carbohydrates that are somewhat inflammatory and difficult to digest. They pull water into the bowel and are easily digested by bacteria, which causes the production of gas. FODMAPs include a lot of foods that contain sugar, like lactose, certain beans, high fructose corn syrup, a lot of bread, cereals, pasta, and sweeteners. If you're considering this, it's a good idea to talk to your provider.
FODMAPs are carbohydrates that are somewhat inflammatory and difficult to digest. They pull water into the bowel and are easily digested by bacteria, which causes the production of gas. FODMAPs include a lot of foods that contain sugar, like lactose, certain beans, high fructose corn syrup, a lot of bread, cereals, pasta, and sweeteners. If you're considering this, it's a good idea to talk to your provider.
References
- ↑ https://www.aboutibs.org/facts-about-ibs.html#:~:text=IBS%20affects%20between%2025%20and,of%20all%20ages%2C%20even%20children
- ↑ https://pubmed.ncbi.nlm.nih.gov/28244679/
- ↑ https://stanfordhealthcare.org/medical-treatments/l/low-fodmap-diet.html
- ↑ https://www.monashfodmap.com/ibs-central/i-have-ibs/starting-the-low-fodmap-diet/
- ↑ https://www.gastrojournal.org/article/S0016-5085(13)01407-8/fulltext
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4918736/
- ↑ https://pubmed.ncbi.nlm.nih.gov/25982757/
About This Article
"A low-FODMAP diet can help you identify and eliminate the cause of your IBS symptoms. It works by targeting the most common culprits of stomach irritation for people with IBS. FODMAP stands for fermentable oligosaccharides (carbohydrates found in wheat, rye, beans, garlic, and onions), disaccharides (carbohydrates found in anything with lactose in it, like milk, yogurt, and cheese), monosaccharides (carbohydrates found in certain fruits and foods that are high in fructose, like figs, mangoes, honey, and agave), and polyols (a type of sugar found in blackberries, lychee, and sugar-free gum). Start the low-FODMAP diet by eliminating all of these foods from your diet for 4-8 weeks. This will give your gut time to heal. Then, introduce one food group from the acronym back into your diet at a time. Eat foods in that group in moderation for at least 3 days. If your IBS symptoms return, you’re likely sensitive to that food group and should avoid it in the future. After testing one food group, move onto the next and eat foods in that group for at least 3 days. Repeat with all of the food groups included in the diet to determine which foods are triggering your IBS and should be avoided. "



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...