This article was medically reviewed by Jonas DeMuro, MD. Dr. DeMuro is a board certified Pediatric Critical Care Surgeon in New York. He received his MD from Stony Brook University School of Medicine in 1996. He completed his fellowship in Surgical Critical Care at North Shore-Long Island Jewish Health System and was a previous American College of Surgeons (ACS) Fellow.
There are 21 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 46,994 times.
Research suggests that a tachycardia episode may be a one-off event and cause no symptoms or complications, but if it happens frequently then it may be a sign of a systemic disease or abnormal heart function.[1] Tachycardia is a potentially dangerous medical condition during which your heart rate speeds up past 100 beats per minute while at rest. Tachycardia can involve the heart's upper chambers (atrial), lower chambers (ventricular), or both. Chronic tachycardia increases your risk of heart attack and stroke. Experts note that home remedies and strategies can help lower your heart rate when you occasionally have a "racing" heart, although chronic tachycardia often requires medication.[2]
Steps
Home Remedies
-
1Stop and rest for a few minutes. Most people experience short episodes of tachycardia on rare occasions due to high levels of stress, a sudden fright or an anxiety attack.[3] If this sounds like the cause of your "racing" heart, then stop what you're doing and rest for five to 10 minutes. Maybe that means turning off a scary movie or removing yourself from a stressful situation (argument) or taking your mind off of a financial problem. Resting, relaxing and taking deep breaths can naturally lower your heart rate.
- Normal resting heart rate can vary quite a bit amongst people, but it's defined as between 60 and 100 beats per minute.[4] Greater than 100 beats, while at rest, is the threshold for defining tachycardia.
- Tachycardia doesn't always cause symptoms, but when it does the main one is feeling a racing heart or palpitations in your chest.[5] Other symptoms are possible and can include: shortness of breath, lightheadedness, dizziness, fainting and chest pain.
-
2Try some relaxation techniques. Since stress and anxiety are relatively common triggers for tachycardia and hyperventilation, you can help prevent them by managing how you react or respond to stressful situations.[6] Stress-relieving techniques like yoga, tai chi, deep breathing, visualization and meditation are all helpful for promoting relaxation and better emotional health.[7] Ask at your local gym, community center or health clinic about joining a stress-relieving class.
- Try to limit the stress in your life by making positive changes — get out of an abusive relationship, change your job, spend less time with negative people. Control anxious thoughts about your work, finances and relationships.
- Excessive stress and anxiety causes the release of hormones that prepare your body for "fight or flight", which leads to increased heart and breathing rates.
- Don't forget to get enough quality sleep — at least eight hours per night, although some people need up to 11 hours for best health. A chronic lack of sleep can lead to anxiety and heart palpitations.
Advertisement -
3Use a vagal maneuver. Vagal maneuvers are simple actions that you can do with your body that affect the vagus nerve, which is the main one regulating your heartbeat.[8] Maneuvers that affect the vagus nerve include doing the Valsalva technique, triggering the diving reflex, and repeatedly coughing. These simple maneuvers should be done as soon as you realize you're experiencing an episode of tachycardia — they can slow your heart rate down within seconds if done correctly. Ask your doctor for a demonstration of these maneuvers.
- The Valsalva maneuver involves holding your breath and bearing down as if you're having a bowel movement for about 10–15 seconds. It's a simple procedure, but it can change the rhythm of electrical impulses in your heart and help your heart rate return to normal.
- All people have a diving reflex, which gets activated when plunged into cold water — the body automatically slows its heart rate down to reduce blood flow in an attempt to preserve itself. To trigger this reflex, put very cold water or an ice pack against your face for at least 30 seconds.
- You can also try coughing forcefully.[9]
-
4Avoid substances and habits that can trigger tachycardia. There are a number of substances that can trigger tachycardia, including alcohol, caffeine, nicotine, some illicit drugs (such as cocaine) and some over-the-counter medications (particularly cold and cough medicines);[10] therefore, if you're having periodic heart palpitations and feel that your heart is racing, you should stop smoking as well as cut back on alcohol and caffeine-rich beverages.
- Caffeine is found in coffee, black and green teas, most soda pop (particularly colas), energy drinks and chocolate. Caffeine doesn't give you energy — it stimulates brain activity and increases heart rate and blood pressure.
- Consuming nicotine from cigarette smoking can increase your resting heart rate up to 15 beats/min and increase blood pressure up to 10 mm Hg.[11]
- Binge drinking alcohol (like on the weekends, for example) often increases heart rate, whereas chronic alcoholism tends to cause fluctuations (from too high to too low).[12]
- Tachycardia is more common in anxious young people, especially among females who drink lots of coffee/alcohol and smoke heavily.[13]
Medical Treatment
-
1Ask your doctor about the cause of your tachycardia. There are three types of tachycardia: atrial or supraventricular tachycardia (SVT), sinus tachycardia, and ventricular tachycardia. They are caused by different things, and discovering which type of tachycardia you are suffering from will help your doctor decide on the appropriate treatment.
- Atrial or supraventricular tachycardia (SVT) begins in the upper chambers of the heart. It is the most common type of tachycardia found in children and may be caused by anxiety, fatigue, smoking, drinking alcohol, or caffeine.[14]
- Sinus tachycardia may be caused by a fever, anxiety, medication or recreational drugs, fright, strenuous exercise, or severe emotional distress.[15]
- Ventricular tachycardia begins in the lower chambers of the heart and can be life-threatening. Seek immediate treatment if you have another cardiac condition and experience rapid heart beat. Ventricular tachycardia may be caused by lack of oxygen in the heart, medication, sarcoidosis (an inflammatory disease), or distortion of the structure of the heart due to disease.[16]
-
2Ask your doctor about medication side effects and interactions. Some medications, particularly when they are combined with others, can trigger bouts of tachycardia as a negative side effect. More specifically, anti-arrhythmic drugs (used to treat abnormal heart rhythms), digitalis, asthma medications, steroid therapy and most cold/cough remedies are well known to increase heart rate.[17] [18] Ask your doctor if your prescription medication(s) could trigger tachycardia as an unwanted side effect.
- Due to complex chemical interactions in the human body, it's virtually impossible to predict how more than two medications (taken concurrently) may interact with each other. Read the list of side effects of your drugs carefully.
- If you suspect a medication is triggering bouts of tachycardia, don't stop taking the drug "cold turkey" without the supervision of your doctor — it may cause worse symptoms. It's better to wean yourself off a medication and then switch to another with similar actions.
-
3Control high blood pressure and cholesterol levels. Cardiovascular disease, particularly atherosclerosis, increases blood pressure and makes your heart work harder by beating faster. High blood cholesterol is a primary risk factor for atherosclerosis, which involves clogged arteries from plaque build up. Clogged arteries trigger higher blood pressure (hypertension), which then often translates into higher than normal heart rate. Ask your doctor about lifestyle changes and medications that can keep blood pressure and cholesterol levels under control so you can reduce your risk of tachycardia.[19]
- Normal blood cholesterol levels are less than 200 mg/dL, whereas healthy blood pressure is less than 135/80 mmHg.[20]
- Reduce saturated and trans fats in your diet and eat more fresh fruits and vegetables, whole grains and nuts.
- If lifestyle and dietary changes don't lower cholesterol levels significantly, then medication may be needed. Cholesterol-lowering medications include statins, niacin-based drugs, bile-acid resins, fibric acid derivatives and cholesterol absorption inhibitors.
- Common medications for high blood pressure include thiazide diuretics, beta blockers, ACE inhibitors, calcium channel blockers and renin inhibitors.
-
4Talk to your doctor about anti-arrhythmic medication. If no other cause of your tachycardia can be found and dietary/lifestyle changes or vagal maneuvers don't help much, then medication will likely be needed. Primary causes of tachycardia that require medicine include cardiomyopathy, congestive heart failure, myocarditis and heart valve disease.[21] Anti-arrhythmic medications can quickly reduce heart rates, especially if they are given via injection. Other medications that may be prescribed (and often used in combination with anti-arrhythmic drugs) are calcium channel blockers (diltiazem, verapami) and beta blockers (metoprolol, esmolol).
- During an emergency situation, a doctor or nurse at the hospital may inject a quick-acting anti-arrhythmic drug (lidocaine, procainamide, sotalol, amiodarone) into a vein to treat an acute case of tachycardia.
- Patients who are at risk for tachycardia may also be given a slow-acting oral anti-arrhythmic medication (flecainide or propafenone) to take at home at the onset of tachycardia.
-
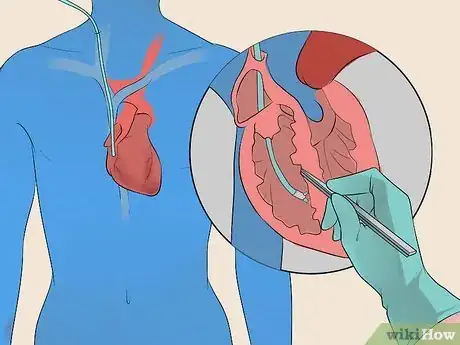
5Consider catheter ablation if appropriate. Catheter ablation is an invasive procedure recommended when an extra electrical pathway (sending too many signals to the heart) is responsible for chronic tachycardia.[22] It involves inserting a catheter into a groin, neck or arm vein and maneuvering it to the heart, where electrodes at the tip of the catheter destroy the extra electrical pathway with either heat, cold or radio frequencies.
- Catheter ablation is very effective, especially for ventricular tachycardia. It can also be used to treat atrial fibrillations and flutters.
- Catheter procedures carry a risk of damaging veins and dislodging emboli that can cause a heart attack or stroke. It may also damage the walls of the heart and affect the electrical system of the heart.[23]
- Tests that your doctor can use to detect a ventricular tachycardia include: a continuous ambulatory electrocardiogram (ECG), a regular ECG, and an intracardiac electrophysiology study.
-
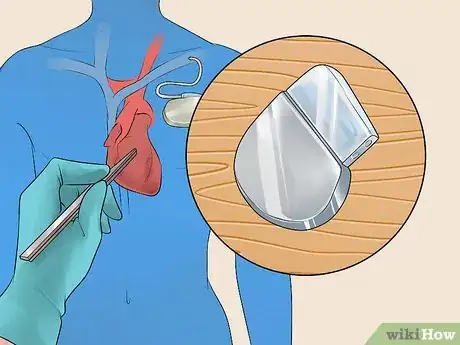
6Think about a surgical procedure if recommended. Surgery is a last resort for controlling tachycardia, but for some it may be the only effective option. There are a couple of different devices that can be implanted into your chest that are effective for treating tachycardia, such as pacemakers and implantable cardioverter-defibrillators.[24] More invasive procedures involve open-heart surgery to either destroy extra electrical pathways or repair heart damage directly.
- A pacemaker is a small device placed under the skin that sends electrical impulses to the heart when it senses abnormal heartbeats. It helps the heart resume normal contractions, rhythms and rates. A pacemaker is used to treat bradycardia (abnormally slow heart beat). When it is used for tachycardia, it is typically combined with a heart rate control medication, and/or RFA of the tachycardic focus.
- An implantable cardioverter-defibrillator (ICD) is a cellphone-sized device implanted in the chest like a pacemaker, but it's connected to the heart with wires.[25] An ICD delivers precisely calibrated electrical shocks when it senses an abnormal heart rate.
- Ask your doctor which of these devices is most appropriate for your tachycardia.
Warnings
- If you have chronic tachycardia episodes, it's important to follow up with regular physical exams at your doctor's office.⧼thumbs_response⧽
- Do not hesitate to call emergency services (9-1-1) if you need help controlling the situation. A heart attack can be a cause of the tachycardia. Prompt treatment can save your life.⧼thumbs_response⧽
- If ventricular tachycardia becomes an emergency situation, it may also require electrical defibrillation (electric shock).⧼thumbs_response⧽
- If you witness someone else experiencing tachycardia, you may need to perform emergency CPR if they faint and become unresponsive.[26]⧼thumbs_response⧽
References
- ↑ https://pubmed.ncbi.nlm.nih.gov/34406996/
- ↑ https://www.cedars-sinai.org/health-library/diseases-and-conditions/i/inappropriate-sinus-tachycardia.html
- ↑ https://www.okheart.com/about-us/ohh-news/what-is-sinus-tachycardia
- ↑ https://www.heart.org/en/healthy-living/fitness/fitness-basics/target-heart-rates
- ↑ https://www.heart.org/en/health-topics/arrhythmia/about-arrhythmia/tachycardia--fast-heart-rate
- ↑ https://www.webmd.com/heart-disease/atrial-fibrillation/vagal-maneuvers-and-heart-rate
- ↑ https://www.webmd.com/fitness-exercise/news/20170616/why-yoga-tai-chi-and-meditation-are-good-for-you
- ↑ https://www.webmd.com/heart-disease/atrial-fibrillation/vagal-maneuvers-and-heart-rate
- ↑ http://www.mercymemorial.org/Resource.ashx?sn=sec5VagalManeuvers
- ↑ https://www.cedars-sinai.org/health-library/diseases-and-conditions/i/inappropriate-sinus-tachycardia.html
- ↑ http://content.onlinejacc.org/article.aspx?articleid=1121737
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1767471/
- ↑ http://www.heart.org/HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/Tachycardia-Fast-Heart-Rate_UCM_302018_Article.jsp#.VnsgnFL9O1s
- ↑ http://www.heart.org/HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/Tachycardia-Fast-Heart-Rate_UCM_302018_Article.jsp#.V4PTApMrJE5
- ↑ http://www.heart.org/HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/Tachycardia-Fast-Heart-Rate_UCM_302018_Article.jsp#.V4PTApMrJE5
- ↑ http://www.heart.org/HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/Tachycardia-Fast-Heart-Rate_UCM_302018_Article.jsp#.V4PWP5MrJE7
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000187.htm
- ↑ http://www.emedicinehealth.com/supraventricular_tachycardia/page2_em.htm#supraventricular_tachycardia_svt_psvt_causes
- ↑ http://www.mayoclinic.org/diseases-conditions/tachycardia/basics/prevention/con-20043012
- ↑ https://www.nlm.nih.gov/medlineplus/magazine/issues/summer12/articles/summer12pg6-7.html
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000187.htm
- ↑ https://pubmed.ncbi.nlm.nih.gov/9892593/
- ↑ http://www.mayoclinic.org/tests-procedures/cardiac-ablation/basics/risks/prc-20022642
- ↑ https://pubmed.ncbi.nlm.nih.gov/8734173/
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000187.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000187.htm
About This Article
If your heart races occasionally even when you’re resting, make an appointment with your doctor to find out what’s causing your tachycardia. To manage a tachycardia episode at home or while you’re going about your day, stop and rest for 5-10 minutes or until your heart slows down. You can also try stress-reducing techniques, such as yoga or meditation, to help slow down your heart when you’re stressed or anxious. For a quick solution, try pinching your nose and bearing down or blowing gently through your nostrils for 10-15 seconds. Additionally, avoid common tachycardia triggers, such as caffeine, nicotine, and alcohol. For more advice from our Medical co-author, including how to get medical care for tachycardia, keep reading!
























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...