This article was co-authored by Laura Marusinec, MD. Dr. Marusinec is a board certified Pediatrician at the Children's Hospital of Wisconsin, where she is on the Clinical Practice Council. She received her M.D. from the Medical College of Wisconsin School of Medicine in 1995 and completed her residency at the Medical College of Wisconsin in Pediatrics in 1998. She is a member of the American Medical Writers Association and the Society for Pediatric Urgent Care.
There are 18 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 96% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 137,250 times.
A fever is an outward sign of illness, usually (although not always) an infection. The body's temperature rises as a protective defense mechanism. The best way to help your child overcome his illness is to monitor the fever and act accordingly. Pay attention to your child and his outward symptoms, and respond with actions that will keep your child comfortable while reducing the fever.
Steps
Choosing and Using a Temperature Device
-
1Choose a digital thermometer. Because of the risk of mercury poisoning if the thermometer breaks, the Canadian Pediatric Society and American Academy of Pediatrics recommend using digital thermometers rather than old-fashioned mercury thermometers to ensure safety.[1] [2]
- Mercury thermometers must be held as long as 3 minutes to get a reading, whereas digital readings come within seconds. For both safety and convenience, a digital thermometer is a better choice.[3]
- The AAP also recommends using a plastic rather than a glass thermometer to avoid the possibility of breakage and injury.[4]
-
2Consider rectal monitoring. Ask your doctor which method is right for you and your child. The American Academy of Pediatrics recommends measuring temperatures rectally using a digital thermometer in children from newborns to 3 years old to get the most accurate reading.[5]Advertisement
-
3Consider a temporal thermometer. A temporal thermometer, or forehead scanner, uses infrared to measure how hot the temporal artery in the forehead is.[8] These thermometers can be more expensive, however, so you may wish to use a regular oral or tympanic (in-ear) thermometer.
- Temporal thermometers can be used in children 3 months and older.[9]
-
4Cradle your child. Being sick can be scary and children always want to be held. Cuddling your child on your lap will allow you to take his temperature more easily because he will be more calm and cooperative.[10]
- Breastfeeding or telling stories will calm and distract the younger child. Older children can sit with their arm around you and snuggle in.
-
5Take the temperature orally or rectally. Oral digital thermometers provide reliably accurate (close to rectal), easily taken temperatures without causing the child too much distress. For children younger than 3, consider taking your child's temperature rectally instead.[11]
- Underarm, or axillary, temperatures may be up to 2 degrees lower than rectal temperatures. This is not as reliable a method as taking a temperature orally or rectally.[12]
- Oral thermometer probes are to be placed under the tongue - not bitten and not clamped down with teeth - and held in place until the probe beeps or 2-3 minutes have passed.
-
6Use the ear for children 18 months and over. Tympanic digital thermometers are also convenient and reliable for taking a child’s temperature. They work by measuring the heat of the ear canal and tympanic membrane inside the ear.[13]
- Pull the ear slightly down and back to allow the ear canal to open for a better reading. Insert the probe a few millimeters into the ear and pause. The tympanic reading is quick, beeps when ready, and is usually only slightly less accurate than rectal.[14]
- A child with an ear infection will have a raised temperature in that ear so the thermometer should be used in the opposite ear if possible.[15] If the ear infection is in both ears, use a different method to check your child's temperature.
-
7Check your child's temperature regularly. Every 4 hours, get a new temperature rating. Record these values so you can monitor rise and fall.
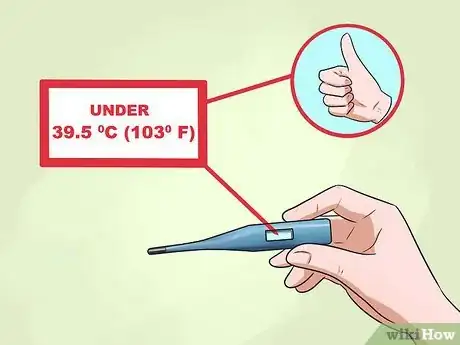
- A normal temperature is up to 37.2C or 99F. Low grade fevers are up to 38.3C or 100.9F and the most common fever range is 38.4C (101F) to 39.7C (103.5).[16]
- High grade fevers are over 39.8C (103.6F) and should be attended to by medical professionals when they do not come down with medication, or if your child seems very ill with a high fever.
-
8Know daily variations. Your temperature is lowest in the morning after a night of rest and highest before bed after a day of activity and normal work of the body. Do not be alarmed if your child’s temperature rises by a degree between these two times (when still less than 39.8C or 103.6F).[17]
Keeping your Child Comfortable
-
1Make sure your child stays hydrated. A fever can quickly dehydrate children due to the sweating and increased bodywork to fight infection. Keep their bodies at full fever-fighting capacity by having them drink a lot of fluids.[18]
-
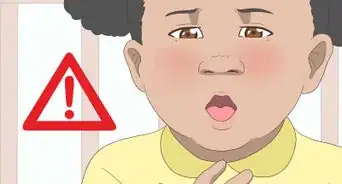
2Know the signs and symptoms of fever beyond temperature. Watch for chills, sweating, flushing of the cheeks, and shivering. These are all normal responses as your child’s body tries to fight off infectious invaders.[19]
- Your child may also complain of muscle and joint pain, which are also normal responses as the body fights off illness.
-
3Offer a lukewarm bath. External cooling techniques such as a lukewarm bath and sleeping with fewer blankets are good ways of keeping your child comfortable during the flushing and sweating responses to the fever. A sponge bath with lukewarm water can make your child more comfortable.[20] Do not make the child so cold as to shiver, as this will actually increase the body’s temperature as a default.[21]
- Cooling techniques encourage heat loss but do nothing to regulate the child’s internal temperature and thus are better used as comfort measures.
- You can use a fan in the room to improve air circulation, but don't position it so that it's blowing directly on your child.[22]
-
4Pay attention to your child's behaviour. Your child may want to sleep a lot, which is a healthy response allowing the body to rest and focus on fighting the cause of the fever. Unusual grogginess and difficulty waking your child from slumber, as well as confusion, are cause for alarm and your child should be taken to medical attention at once.[23]
Treating your Child’s Fever
-
1Let the fever ride its course. Fevers under 39.5C (103F) are generally not harmful in themselves. In many cases, fever is a good thing, as it is the body’s way of raising the temperature of the environment to be toxic to pathogens, bacteria, and viruses.[24]
- Fever usually does not cause harm, is self-limiting, and medication is usually not needed. Fever usually lasts no more than a few days.
- Infants under the age of 12 weeks with a fever of 38C (100.4F) or greater should go directly to emergency.[25]
- The main reason to treat a fever is to make your child more comfortable. But, if the fever is high (39.8C/103.6F or higher), you should consider treating it and seeking medical attention.
-
2Reduce a high fever or discomfort from fever with medication. Antipyretic (anti-fever) medications work on regulating the hypothalamus, the temperature centre in the brain. Both acetaminophen (Tylenol) and ibuprofen (e.g., Motrin, Advil) work well and should reduce the fever within 1.5 to 2 hours.[26] If your feverish child is younger than 2, consult with your pediatrician before giving any medication.[27]
- Do not give children aspirin (ASA, acetylsalicylic acid). Children who take aspirin can fall ill with Reye syndrome, a life-threatening illness that causes swelling of the brain and other issues.[28]
- Always be sure to give the correct dosage to a child. Children do not take the same amount as adults. Dosages are based on age and weight so read the bottle carefully to determine the right dose for your child based on the bottle guidelines. Check with your doctor or pharmacist if you are uncertain how much to give.
- There is no evidence that alternating medications reduces fever any quicker; rather, it can lead to dosage errors. This practice is not recommended in children.[29]
- Do not give ibuprofen to children younger than 6 months. If your child is vomiting or dehydrated, do not use ibuprofen.[30]
-
3Seek professional or emergency help if the fever is uncontrollable. Take your child to a doctor if he has a high fever (over 40C or 104F) that does not come down to 38.3C (101F) to 38.9C (102F) with medication. Also take your child to the doctor if the fever lasts over 24 hours (for children younger than 2) or 3 days (for children 2 and over) or if the child becomes dehydrated.[31]
- Take your child to emergency immediately if he becomes severely lethargic (drowsy), unresponsive, has trouble breathing, has a stiff neck, has a sudden rash, or becomes violently ill.
-
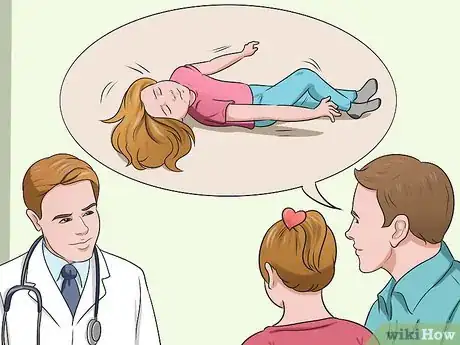
4See your doctor if your child has a febrile seizure. A febrile seizure is a seizure caused by a sudden high temperature and looks like stiffening of the body, involuntary jerking movements, eyes rolling back into the head, and loss of consciousness. A febrile seizure may last 2 minutes and looks very scary but is not necessarily harmful.[32]
- If your child is having a seizure, do not hold him down, try to stop him, or stick anything into his mouth. Remove his glasses and put something soft under his head if you can. Lay him on his side if possible. Let him be and move nearby furniture or sharp objects. Time the seizure and tell your doctor how long it lasted. If the seizure lasts more than 3 minutes, call an ambulance.
- Take your child for medical attention, even if he feels sleepy and wants to just rest at home. The doctor will want to ask questions to rule out any causes other than fever.
- Febrile seizures are common and do not cause brain damage or epilepsy.
References
- ↑ http://www.gov.mb.ca/health/documents/fever.pdf
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/How-to-Take-a-Childs-Temperature.aspx
- ↑ https://www.nationwidechildrens.org/family-resources-education/health-wellness-and-safety-resources/helping-hands/temperature-digital-and-glass-thermometers
- ↑ https://medlineplus.gov/ency/article/003400.htm
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/How-to-Take-a-Childs-Temperature.aspx
- ↑ https://www.nationwidechildrens.org/family-resources-education/health-wellness-and-safety-resources/helping-hands/temperature-digital-and-glass-thermometers
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/How-to-Take-a-Childs-Temperature.aspx
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/measuring-a-babys-temperature
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/How-to-Take-a-Childs-Temperature.aspx
- ↑ http://www.gov.mb.ca/health/documents/fever.pdf
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/How-to-Take-a-Childs-Temperature.aspx
- ↑ https://health.clevelandclinic.org/your-childs-fevers-5-common-myths-debunked/
- ↑ https://www.seattlechildrens.org/health-safety/keeping-kids-healthy/prevention/fever/
- ↑ http://www.gov.mb.ca/health/documents/fever.pdf
- ↑ http://www.pharmaceutical-journal.com/learning/learning-article/questions-from-practice-monitoring-fever-in-young-children/11046537.article
- ↑ https://medlineplus.gov/ency/article/001982.htm
- ↑ https://www.health.harvard.edu/blog/time-to-redefine-normal-body-temperature-2020031319173
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/Treating-a-Fever-Without-Medicine.aspx
- ↑ https://my.clevelandclinic.org/health/symptoms/10880-fever
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/Treating-a-Fever-Without-Medicine.aspx
- ↑ http://www.gov.mb.ca/health/documents/fever.pdf
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/Treating-a-Fever-Without-Medicine.aspx
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/When-to-Call-the-Pediatrician.aspx
- ↑ https://www.seattlechildrens.org/conditions/a-z/fever-myths-versus-facts/
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/When-to-Call-the-Pediatrician.aspx
- ↑ http://www.gov.mb.ca/health/documents/fever.pdf
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/Medications-Used-to-Treat-Fever.aspx
- ↑ http://kidshealth.org/parent/system/medicine/reye.html
- ↑ http://www.aafp.org/afp/2012/0301/p518.html
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/Medications-Used-to-Treat-Fever.aspx
- ↑ https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/When-to-Call-the-Pediatrician.aspx
- ↑ http://www.aboutkidshealth.ca/en/healthaz/conditionsanddiseases/brainandnervoussystemdisorders/pages/febrile-seizures-convulsions-caused-by-fever.aspx
About This Article
To monitor a child’s fever, take their temperature every 4 hours, and record the results so you can track if the fever is staying the same or getting worse. Remember, a normal temperature is up to 99 degrees Fahrenheit, and a low grade fever can be up to 100.9 degrees Fahrenheit. When you take your child’s temperature, note if it’s between 101 and 103.5 degrees Fahrenheit, which is within the most common fever range. However, if your child has a high grade fever over 103.6 degrees Fahrenheit that doesn’t come down with medication, you should seek medical assistance. Make sure your child stays hydrated since fevers can dehydrate the body. You can also offer a lukewarm bath to externally cool your child. For more tips from our Medical co-author, including how to treat your child’s fever with medication, keep reading!









































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...