This article was co-authored by Ni-Cheng Liang, MD. Dr. Ni-Cheng Liang is a board certified Pulmonologist and the Director of Pulmonary Integrative Medicine at Coastal Pulmonary Associates affiliated with the Scripps Health Network in San Diego, California. She also serves as a Voluntary Assistant Professor of Medicine at the University of California San Diego School of Medicine while volunteering for the UCSD Medical Student-Run Free Clinic for uninsured patients. With over 15 years of experience, Dr. Liang specializes in pulmonary and respiratory medical concerns, mindfulness teaching, physician wellness, and integrative medicine. Dr. Liang received her Doctor of Medicine (MD) from the University of Maryland School of Medicine. Dr. Liang was voted as a San Diego Top Doctor in 2017 and 2019. She was also awarded the 2019 American Lung Association San Diego Lung Health Provider of the Year.
There are 12 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 4,694 times.
Amid the COVID-19 pandemic, exposure to other people is a scary and risky concept. However, thanks to recent scientific breakthroughs and developments, many new technologies have come into the usage of common folk. One of these technologies is the COVID-19 rapid antigen test, which can be purchased at any convenience store and provides a safe and professionally approved [1] way to test for COVID-19 at home, [2] which can help eliminate the need for exposure, as well as being required for that clean bill of health you need to provide for your next flight. [3] Now, with self-tests being replacements for lab-examined testing, everyone needs to know the tips and tricks for safe sampling for COVID-19 at home. This guide provides help on safe sampling, covering all different approved methods as well as ample information on helping kids with this process.
Steps
Preparing to Sample
-
1Check for any physical requirements the test may require. This should be located in either the introduction of the instructions card or on the face of the box. This is especially important, as some tests are not suitable for certain people.[4]
- Some tests have a minimum age requirement.[5] Before helping your child take the test, check if they are old enough for the particular product.
-
2Check the expiration date for the test. This should be located on the face of the box. Expired tests do not function properly, so make sure that the test in hand is not expired before purchase or use.[6]Advertisement
-
3Read the instructions card. This will include information on how you can administer your samples to get test results, as well as other important information provided by the producer. Read thoroughly and carefully.
- The instructions card includes information on what to do with your sample and how to get your result, which varies greatly from kit to kit. Make sure that you prepare all necessary equipment before continuing to take the sample. The card can also help to identify the type of sample needed.
- Make sure to set up the test as per the card before moving on, as you will have a limited time after testing to administer the sample.
-
4Find and disinfect a flat, cool, surface that is not in direct sunlight. These conditions are vital for the accuracy and validity of the test results. After you have located such a surface, use any suitable cleaning agent to perform the disinfection.
- If you are using commercial cleaners, try to use those that include alcohol, peroxide, or chlorine contents. These are more effective for this goal.
- If you lack commercial cleaners in the pandemic, use preferably undiluted alcohol or hydrogen peroxide solutions.
-
5Wash your hands. The test needs to be taken in a sterile environment, and unclean hands may mean germs and other microbes contaminating the test results. Wash your hands thoroughly, preferably with soap and water.
- It is required that you keep your hands clean and sterile throughout the test, so make sure to not touch anything that has a chance of contaminating the samples.
-
6Check for the type of sample required for the test. Through the instructions leaflet, locate the section on sample collection and see what type of sample the test requires. There are 3 types of samples, though many tests require more than one of them. However, keep in mind that these combinations are mostly fluid, and if you do not fit all the criteria for the sampling method below, you can change to another (e.g. mouth + nostril can be substituted with 2 nostrils).
- Nasal sampling refers to samples collected through the nose and is not suitable for toddlers. The nostrils of smaller kids are underdeveloped, and using nasal collection might cause damage to the nose. Discomfort is inevitable. You will need to remove your nose ring(s) if you have any on.[7]
- Oral sampling refers to samples collected through the mouth. This is suitable for people of all ages. Similarly, to nasal sampling, there can be a certain amount of discomfort while performing this test. Do not use if you have had any form of medical operation previously (e.g. wisdom tooth removal, etc.).
- Spit tubing refers to sampling by saliva administered into a test vial. It is suitable for smaller children. This method also tends to be the most inaccurate,[8] but is a great option for little kids, since it causes no discomfort. However, it is usually not recommended due to its difficulty to administer and provide results.
-
7Locate and unwrap the collection swab carefully, holding it by the shaft.[9] Carefully pull on the labeled part of the wrapping. Pull from the bottom up to avoid touching the tip. After you expose the bridge of the Q-tip, use it to pull the rest out.
- Do not touch the tip of the swab from here on out. This limits the possibility of contamination and guarantees more accurate results.
- Before testing, make sure that you are not allergic to the Q-tip materials. The tips are hypoallergenic, but a small number of people may still be allergic, potentially causing them to sneeze during the test and causing dangerous consequences.
- Note that both oral samples and nasal samples must be conducted with the same swab, so do not test the swab immediately after use: all specimens have to be collected onto it before you administer the test.
Performing a Nasal Sampling
-
1Blow your nose. This helps to bring mucus to the sampling area.[10]
-
2Insert the tip of the swab into your nose slowly until you feel resistance. [11] There will be a certain level of discomfort involved, so keep that in mind before administering the test. The length usually required to insert is about 2–2.5 cm (0.79–0.98 in) in adults, but can vary from person to person.[12]
- The length of the swab you insert into the nostril will be greatly different in children and minors. Try not to pressure a child’s nose too much if you are helping them administer the test. This may cause damage to the nose. Instead, insert only a little at a time, asking the child when they feel resistance and adjusting the swab based on their description. Explain to them beforehand what resistance feels like, and that the test is meant to be uncomfortable.
-
3Rotate and swirl the swab around in your nose about 5-10 times, pressing it gently onto the nasal walls.[13] This ensures the collection of a wide range of samples, including cells and mucus. Refrain from moving the swab further or farther down the nostril.
- Take it slowly and avoid any sudden or violent actions to ensure the safety of the person being tested. Remember that the nose is a very sensitive organ and should be treated delicately to avoid injury.
-
4Extract the swab from your nostril slowly.[14] The tip of the swab must not come into contact with any other surface or your face to ensure the validity of the specimen.
- If you are helping children execute this maneuver, get them to hold still until the swab is completely out of their nostrils. Often, it can feel like the swab has left the nostril when in reality it has only been lifted from resistance.
-
5Repeat the process with the other nostril if a nasal sample has been instructed on the instructions card. [15] If your instructions card informs you to use nasal sampling, it requires a specimen from both nostrils. Carefully reread this section and repeat for your other nostril using the same cotton swab.
Performing an Oral Sampling
-
1Refrain from food and drink for at least 30 minutes before the test.[16] You cannot eat anything before receiving an oral sampling. This ensures the purity and validity of the sample.
- Brushing your teeth could also help to make sure no food residue remains, as it is important not to contaminate the specimen.
-
2Enter the swab into your mouth and press the swab onto the tonsils, between the teeth and gums in the back of the mouth.[17] This ensures for collection of saliva and cells that are secreted by the saliva ducts, ensuring the purity of the samples. Avoid your teeth and tongue during this step.
- If you have had your tonsils removed, simply place the swab where they should have been.
- If you are suffering from tonsil stones, infection, or any other form of tonsil medical issues, place the swab relatively closer to the lips, but on the same horizontal axis as your tonsils.
-
3Rotate the swab in place for 5-10 seconds. There should be no discomfort in this step. Be sure to be extra light, as the tonsils are sensitive and how hard you press on the surface does not affect the success of the sampling as long as the swab is in place.
-
4Repeat for the other cheek. Once again, make sure to avoid your teeth and gums, and rub the swab gently against the side of your cheek.
-
5Move the swab as far toward the back of the throat or tongue as you can comfortably reach. [18] If it helps you locate the area, try sticking out your tongue as well. [19] Do not go too far down the throat, as this could become a potentially dangerous choking hazard.
- A gag reflex is a good thing, simply telling you that the swab is in place. To collect mucus for testing, the swab should be able to trigger a gag reflex. This is your signal that the swab is in place.
- When helping children, tell them to sick out their tongue and make the “ahhh” sound. Look for an arch at the back of the mouth and position the swab on it. [20] Make sure they do not stop making the sound, as this helps to eliminate the gag reflex and allow you to execute the move easily.
-
6Rub the swab against the back of the throat or tongue in a circular fashion for 5-10 seconds. [21] This should provide the test with ample mucus sampling from the throat. This could be mildly uncomfortable, but should not be painful.
- If you are concerned about your gag reflex activating, make the “ahh” as you would at a dentist. The sound comes from the throat and helps to eliminate the gag reflex, allowing for easier collection.
-
7Extract the swab. Make sure it does not come into contact with any other surfaces to avoid contamination.[22]
Performing an Oral Fluid Collection (Spit-tubing)
-
1Assemble the spit tube. [23] Locate the plastic funnel and specimen vial. Hold the funnel by the neck and, using force on the specimen vial, press the opening of the specimen tube together with the neck of the funnel. They should fit into each other, with the funnel neck fitting over the vial.
- Be sure not to touch the inside of the funnel or tube during this process. You want to make sure that the sample is exposed to as little outside material as possible.
-
2Cough 3-5 times deeply. [24] Making sure not to spit saliva outwards, bring up a cough from the back of the throat. This helps to guarantee that mucus is brought into the saliva and collected in the following steps.
Warning! Do NOT swallow any saliva after coughing. You want to make sure that the saliva which will be collected contains mucus from your throat, so swallowing the mucus-filled saliva at this point will render this step pointless.
-
3Bring your head over the opening of the funnel and spit into the funnel until oral fluid reaches the scale line marked on the vial. [25] Do not come into contact with the mouth of the funnel. Keep spitting until you reach the scale line, as this is the necessary amount of specimen required for a conclusive result.
- If you seem to be unable to locate the scale line or unsure which of the numbered markers is the scaled line, consult the instructions card, it should include a description on which number value to spit to.[26]
- Make sure not to move on until all the spit left in the funnel has drained into the test vial.
-
4Disconnect the funnel. Gently, making sure not to spill the specimen, lift the funnel off of the opening of the test vial. Anchor the hand holding the vial to a surface, such as a table, and use your other hand to pull the funnel off.[27]
After Sampling
-
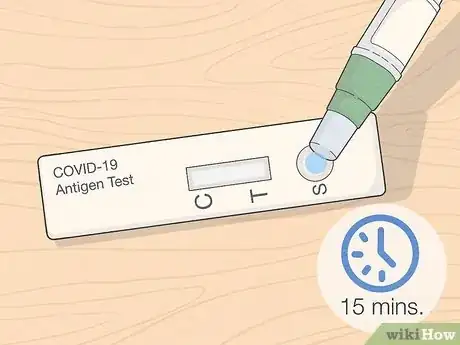
1Administer the rest of the test within 15 minutes of sampling. The sample should not be allowed to sit for more than a quarter of an hour after being taken from the body, as this will not allow for the most accurate results.[28]
- The instructions card outlines the rest of the procedure, which will vary from product to product.[29]
-
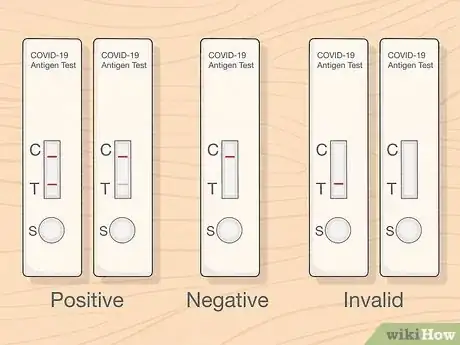
2Check and respond correctly to your results. The instructions for reading your test results will be outlined in the manufacturer's guide. Make sure to understand each result as well, as a correct interpretation of results can prove important in the protection of yourself and your loved ones. Learn how to react to these results with this article.
-
3
-
4Set a date for later testing. Many test kits require you to take a sample test 36 hours after the first test.[34] Check the instructions card to find out whether a second test is necessary. Mark down the next date in your calendar for the most conclusive results.
References
- ↑ https://www.tga.gov.au/covid-19-rapid-antigen-self-tests-are-approved-australia
- ↑ https://www.ontario.ca/page/rapid-testing-home-use
- ↑ https://www.nytimes.com/wirecutter/reviews/at-home-covid-test-kits/
- ↑ https://www.verywellhealth.com/best-at-home-covid-tests-5208810
- ↑ https://www.verywellhealth.com/best-at-home-covid-tests-5208810
- ↑ https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antigen-tests-guidelines.html
- ↑ https://www.coronavirus.vic.gov.au/rapid-antigen-tests
- ↑ https://www.coronavirus.vic.gov.au/rapid-antigen-tests
- ↑ https://www.youtube.com/watch?v=XQlTGs6CIJo
- ↑ https://www.youtube.com/watch?v=fJEIpwsb6Yk&t=23s
- ↑ https://www.coronavirus.vic.gov.au/rapid-antigen-tests
- ↑ https://www.youtube.com/watch?v=XQlTGs6CIJo
- ↑ https://www.youtube.com/watch?v=XQlTGs6CIJo
- ↑ https://www.youtube.com/watch?v=XQlTGs6CIJo
- ↑ https://www.youtube.com/watch?v=fJEIpwsb6Yk&t=23s
- ↑ https://www.youtube.com/watch?v=LJhdIWWdXT4
- ↑ https://www.youtube.com/watch?v=LJhdIWWdXT4
- ↑ https://www.youtube.com/watch?v=S9XR8RZxKNo&t=220s
- ↑ https://www.youtube.com/watch?v=LJhdIWWdXT4
- ↑ https://www.youtube.com/watch?v=S9XR8RZxKNo&t=220s
- ↑ https://www.youtube.com/watch?v=LJhdIWWdXT4
- ↑ https://www.youtube.com/watch?v=S9XR8RZxKNo&t=220s
- ↑ https://www.youtube.com/watch?v=m_SbsHwwjkA
- ↑ https://www.youtube.com/watch?v=m_SbsHwwjkA
- ↑ https://www.youtube.com/watch?v=m_SbsHwwjkA
- ↑ https://www.youtube.com/watch?v=BJGNHCJ4qo4&t=15s
- ↑ https://www.youtube.com/watch?v=m_SbsHwwjkA
- ↑ https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antigen-tests-guidelines.html
- ↑ https://www.coronavirus.vic.gov.au/rapid-antigen-tests
- ↑ https://www.verywellhealth.com/best-at-home-covid-tests-5208810
- ↑ https://www.coronavirus.vic.gov.au/rapid-antigen-tests
- ↑ https://www.youtube.com/watch?v=BJGNHCJ4qo4&t=15s
- ↑ https://www.coronavirus.vic.gov.au/rapid-antigen-tests
- ↑ https://www.verywellhealth.com/best-at-home-covid-tests-5208810














































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...