This article was medically reviewed by Shari Forschen, NP, MA. Shari Forschen is a Registered Nurse at Sanford Health in North Dakota. Shari has worked in healthcare since 1996 and her expertise lies in acute care bedside nursing on a medical oncology floor. She received her degree from Medcenter one College of Nursing in 2003 and her Family Nurse Practitioner Masters from the University of North Dakota in 2014. Shari is a member of the American Nurses Association.
There are 8 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 462,218 times.
Sleep apnea is a sleep disorder characterized by not breathing continuously while sleeping, but rather breathing irregularly in starts and stops. It can result in loud snoring, extreme fatigue and daytime somnolence due to sleep deprivation.[1] One treatment is using a continuous positive airway pressure (CPAP) machine. When you use a CPAP machine, a mask is needed while sleeping. The mask is connected to a machine that produces air pressure, which helps keep your airways open and improves the quality of your sleep. In order to have this machine available a diagnosis from your physician of obstructive sleep apnea is needed. Also, a sleeps study (polysomnography) is needed to conclude that this is the condition causing secondary symptoms. If you are concerned that the pressure setting isn't right, consult your doctor again to see how you can rectify it.
Steps
Contacting Sleep Professionals
-
1Do an overnight sleep study. When you sleep overnight in a specialized sleep laboratory and get diagnosed with sleep apnea, the team of doctors will determine what the optimum average constant pressure is for you on your CPAP machine. The process by which they figure out the most appropriate air pressure is called a titration study.[2] A titration study is done with a mask and air machine for the purposes of calibrating a CPAP machine to a level that stops your sleep apnea events.
- The events are measured in a point system called an apnea hypopnea index. An index below five indicates no sleep apnea.
- Mild OSA: AHI of 5-15. Involuntary sleepiness during activities that require little attention, such as watching TV or reading
- Moderate OSA: AHI of 15-30. Involuntary sleepiness during activities that require some attention, such as meetings or presentations.
- Severe OSA: AHI of more than 30. Involuntary sleepiness during activities that require more active attention, such as talking or driving.[3]
- Sleep clinics typically do not recommend that new CPAP users change their pressure settings until they've had their first sleep study and used the prescribed pressure settings for several weeks at minimum.
- While you are in the sleep lab, the doctor or sleep specialist may also:[4]
- Measure your activity levels and movement as you sleep
- Record your brain activity, eye movements, blood pressure, heart rate, and blood oxygen levels
- Fine-tune the fit of your mask and the air pressure settings
- The events are measured in a point system called an apnea hypopnea index. An index below five indicates no sleep apnea.
-
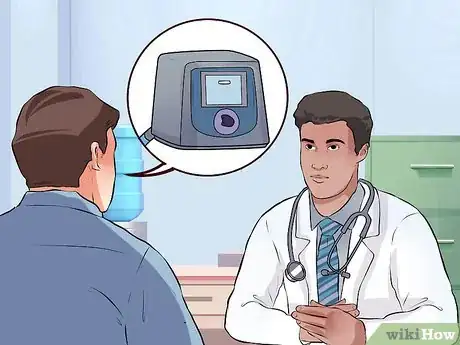
2Consult with your doctor. Doctors and manufacturers recommend that the air pressure settings of your CPAP machine be personalized for you by a medical professional based upon a titration study at a sleep clinic — you should then use those recommended settings for at least a few weeks to get used to them at night. If you think those initial settings need to be adjusted, you should contact your doctor or sleep clinic to have them checked.[5] [6] Adjustment of the air pressure settings may be necessary when:[7]
- You gain or lose weight
- You are extra tired
- You have had a few alcoholic drinks
- You are on prescribed sedatives
- You have sinus congestion
- You are using a different mask
- You are at a different altitude
- You have jet lag
- You change stages in your sleep cycle
Advertisement -
3Ask your doctor about an auto-adjusting CPAP. If you're considering changing your CPAP air pressure settings, the safer method is to upgrade from a constant-pressure machine to an auto-CPAP machine.[8] These fully automated machines continually measure the air pressure needed to keep your airways open and then self-adjust on a regular basis according to your ongoing needs.[9]
- An auto-CPAP machine is likely the best long-term option, since your air pressure needs change day by day (and even hour by hour) as you sleep.
- A one-time titration study within a sleep clinic cannot account for various personal changes that impact air pressure needs, such as: what sleep stage you're in, sleeping position, what you eat / drink, your body weight, and various drugs you take.
- Auto-adjusting helps prevent you from swallowing air at times when your standard pressure is too high. Swallowing air can make people feel bloated and disrupt their sleep.
Making Adjustments Yourself
-
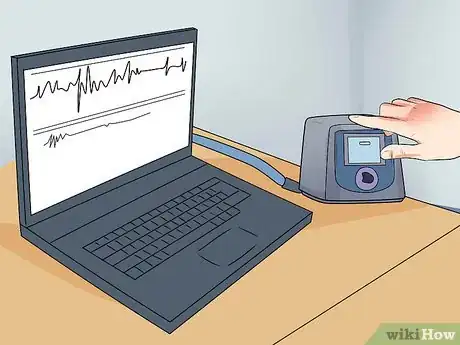
1Read the operating manual. Before you touch and manipulate the settings of your CPAP machine, make sure to read the operating manual and gain an understanding of your machine type and the available options. There are 2 main types of constant-pressure CPAP machines (data recording and non-data recording) and the methods used to adjust the pressure settings is dependent upon which type you have.[10]
- A data recording machine usually stores patient data that is viewable on the machine or from a removable "smart card" or other memory card on your computer.
- A data recording machine records several variables that help determine optimum air pressure, including your Apnea/Hypopnea Index or AHI.
- In contrast, a non-data recording machine records very little or no health information or variables, so you're kind of adjusting these machines by feel.
- Contact the manufacturer to obtain patient and clinician manuals to get a better understanding of your machine.
-
2Adjust a data recording CPAP machine. Adjusting this type of Respironics CPAP machine is easier because you have data to guide you, particularly your AHI. You want to have an AHI of less than 5.0, which means that you experience less than 5 incidents of apnea or hypopnea per hour (considered normal sleep).[11] If your AHI is already less than 5.0 (or even better, less than 3.0), then you shouldn't adjust the air pressure. If it's greater than 5.0, then read the instructions on how to increase the pressure.
- Most CPAP machines have a range of adjustment from 4cmH20 (the lowest pressure) to 20cmH20 (the highest pressure).
- For the Respironics CPAP machine, you need to highlight the Setup option on the display screen and then hold down the ramp and wheel buttons at the same time for a few seconds until you hear a few beeps.
- After the beeps, access the Setup option and scroll down the menu to select the Auto Max and the Auto Min options. These represent the maximum and minimal pressures the machine oscillates between during the night.
- Try increasing the Auto Min setting first (so it's closer to the Auto Max setting). After adjusting very slightly, leave it at that for a few weeks to adequately evaluate the improvement, or lack of sleep quality and daytime alertness.
- You may have to increase both the Auto Max and Auto Min pressure settings, but use your AHI as a guide of how you're responding in the night while sleeping.
-
3Adjust a non-data recording CPAP machine. Adjusting a non-data recording Respironics CPAP machine is more difficult because you don't have an objective AHI to guide you to either raise or lower the air pressure.[12] Instead, you must use the very subjective "how-do-I-feel" approach when you wake up in the morning. If you don't feel rested upon waking or if your partner informs you of your sleep apnea / snoring / gasping, then you'll likely want to increase the pressure settings.
- To change the settings on a non-data recording Respironics CPAP machine, follow the instructions above on how to change them on a data recording machine.
- The main difference is that you won't be able to access the Data option beforehand to see your AHI.
- In the vast majority of cases, people unhappy with the settings on their CPAP machine want to increase the pressure in order to get more air.
- In a minority of cases, people may want to lower the settings because the pressure is too great and creating noisy leaks from their masks, causing bloating or leading to excessive dry mouth.
-
4Make your adjustments gradually. Whichever type of CPAP machine you have, the key is making small adjustments and then see how your AHI number responds (a more objective measure), or how you feel in the morning after waking up (a completely subjective measure). As such, you should not change your air pressure more than 0.5 cm/H20 at any one time, on either your Auto Max or Auto Min settings.[13] After the change, give it at least a week or so before you assess the effectiveness of the change.
- Changing air pressure too much at a time can decrease the effectiveness of your therapy and potentially lead to dangerous health complications.
- Always start by raising your Auto Min setting, which is often set between 5-8cm/H20, and then gauge effectiveness before changing the Auto Max setting — usually set at around 15cm/H2O.
- Even if your have access to your AHI, keep a written log of how you feel each morning, afternoon and evening.
- Don't make dramatic lifestyle / dietary changes that could change your optimum air pressure and confuse you while altering settings to your CPAP machine.
-
5Change your mask instead. Sometimes the problem isn't actually with your air pressure — it has more to do with the type of mask you're wearing.[14] The design of some partial and full-face breathing mask don't allow the air to flow through them (especially through the nose piece) as well as others. In essence, some masks create more resistance than others do.
- Before changing your pressure settings on your Respironics CPAP machine, ask your doctor or sleep clinician to try a different type of mask.
- Switching to a more comfortable mask may necessitate raising or lowering your pressure settings depending on it's design.
- For many people, having an Auto Min setting greater than 10cm/H20 starts to cause uncomfortable side effects such as bloating, belching and dry mouth.
-
6Investigate the legality of changing the settings. It appears that changing your CPAP settings requires a prescription from your doctor because the machines are classified as Class II Medical Devices. As such, changing the settings requires a physician's oversight either directly (in person) or indirectly (faxed prescription). This gives you two options: going to your doctor's office with your machine, or calling the physician and getting them to fax the prescription (changed settings) to the medical equipment company.
- If it's a hassle or too great of an expense to see your physician, call and talk to their secretary or nurse and explain that you want to change the settings and need a faxed prescription.
- Alternatively, call the medical equipment company and ask them to contact the doctor's office on your behalf.
- Without proper medical training and licensing, changing the settings on a CPAP device can get you into legal trouble, so make sure you know the law in your area.
References
- ↑ http://www.mayoclinic.org/diseases-conditions/sleep-apnea/basics/definition/con-20020286
- ↑ http://www.apneaboard.com/adjust-cpap-pressure/how-to-find-optimum-pressure-on-cpap
- ↑ http://www.aasmnet.org/resources/factsheets/sleepapnea.pdf
- ↑ https://www.nhlbi.nih.gov/health/health-topics/topics/slpst/during
- ↑ http://www.mayoclinic.org/diseases-conditions/sleep-apnea/basics/treatment/con-20020286
- ↑ https://www.sleepapnea.com/treatment/cpap-devices-masks/
- ↑ http://www.cpap.com/DisplayNewsletter/56/Whats-New-In-CPAP-Machines-AutoAdjusting-CPAPs.html
- ↑ http://www.apneaboard.com/adjust-cpap-pressure/how-to-find-optimum-pressure-on-cpap
- ↑ http://www.cpap.com/DisplayNewsletter/56/Whats-New-In-CPAP-Machines-AutoAdjusting-CPAPs.html
- ↑ http://www.apneaboard.com/adjust-cpap-pressure/how-to-find-optimum-pressure-on-cpap
- ↑ http://www.apneaboard.com/adjust-cpap-pressure/how-to-find-optimum-pressure-on-cpap
- ↑ http://www.apneaboard.com/adjust-cpap-pressure/how-to-find-optimum-pressure-on-cpap
- ↑ http://www.apneaboard.com/adjust-cpap-pressure/how-to-find-optimum-pressure-on-cpap
- ↑ http://www.apneaboard.com/adjust-cpap-pressure/how-to-find-optimum-pressure-on-cpap
- ↑ http://www.mayoclinic.org/diseases-conditions/sleep-apnea/basics/symptoms/con-20020286

































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...