This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 13 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 117,884 times.
Fevers are reflective of an increase in the body's temperature. Mild fevers are typically beneficial because they represent the body's natural ability to defend itself against infections, as many pathogens can only reproduce in a narrow temperature range.[1] However, high fevers—for example, temperatures of 103 °F (39 °C) or greater for an adult, are dangerous and should be closely monitored and potentially treated with medication. A digital ear thermometer, also called a tympanic thermometer, is a quick and easy way to monitor either your own or a child’s body temperature. Ear thermometers measure the infrared radiation (heat) coming off the eardrum (tympanic membrane) and are considered quite accurate under most conditions.
Steps
Age Guidelines
-
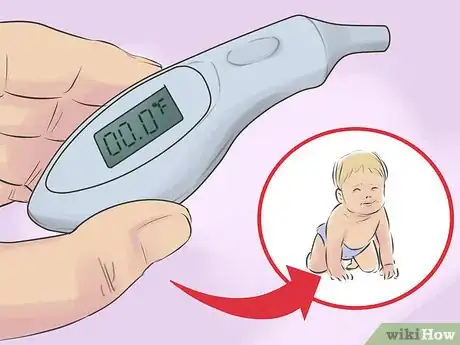
1Select a rectal thermometer for newborns. The best or most appropriate type of thermometer to use to measure body temperature depends mainly on age. From birth to about 6 months of age, using a regular digital thermometer to take a rectal (anal) temperature is recommended because it's considered the most accurate.[2] Earwax, ear infections, and small, curved ear canals interfere with the accuracy of ear thermometers, so they are not the best types to use for newborns.
- Some medical research suggests that temporal artery thermometers, which you use by pressing a sensor against the baby’s temple, are also good options for newborns due to accuracy and reproducibility.
- Newborns have lower body temperatures than adults—typically less than 97.5 °F (36.4 °C), versus a normal of 98.6 °F (37.0 °C) in adults.[3] Babies may not regulate their body temperature very well when they're sick, and they may become cooler rather than warmer and feverish.
-
2Use an ear thermometer cautiously with toddlers. Up to an age of about 3 years, a rectal thermometer still provides the most accurate readings for core body temperature.[4] You can use an ear thermometer at a younger age to get a general reading (which is better than no reading at all), but until about the age of 3, readings from the rectum, armpit, and temporal artery (in the temple region of the head) are considered more accurate. Mild-to-moderate fevers in toddlers can be more dangerous than in adults, so accuracy during the younger years is especially important.
- Ear infections are quite common in babies and toddlers, and that affects the readings of ear thermometers due to the inflammation within the ear. This means an ear thermometer typically gives too high of a reading with ear infections, so check both ears in case one is infected.
- Regular digital thermometers can record temperatures from the mouth (under the tongue), armpit, or rectum, and are appropriate for newborns, toddlers, older kids, and adults.
Advertisement -
3Choose any thermometer for children 3 years or older. Beyond the age of 3 years, kids tend to get fewer ear infections and it's much easier to clean their ears and remove wax buildup. Wax in the ear canal prevents ear thermometers from accurately reading the infrared radiation coming off the eardrum.[5] Furthermore, the child's ear canal has grown by this age and become less curved. For this reason, beyond the age of 3 years, all types of thermometers used in all parts of the body are pretty comparable in terms of accuracy.
- If you use an ear thermometer to take a child's temperature and you're skeptical of the results, then take a rectal temperature with a regular thermometer and compare the results.
- Ear thermometers have become much more affordable over the last decade and can be widely found in pharmacies and medical supply stores.
Taking a Temperature Reading
-
1Clean the ear first. Because wax buildup and other debris in the ear canal can reduce the accuracy of ear thermometers, be sure to clean the ear you're taking a reading from thoroughly. Avoid using a Q-tip or similar method, because the wax or other debris can easily become impacted against the eardrum. The safest and most effective way to clean ears is by using a few drops of warm olive oil, almond oil, mineral oil, or special ear drops to soften the earwax, then rinse it all out (irrigate it) with some squirts of water from a little rubber device made for ear cleaning.[6] Allow the ear canal to dry before proceeding with your reading.
- Ear thermometers will give too low of a temperature reading if there is earwax or debris in the ear canal.
- Do not use an ear thermometer on an ear that is sore, infected, injured, or recovering from surgery.
-
2Put a clean cover on the thermometer's tip. Once you take the ear thermometer out of its box and read the instructions, put a disposable sterile cover over the tip. Because you're inserting the tip into the ear canal, you want to make sure it's clean so there's much less risk of causing an ear infection — something that young kids are predisposed to already. If, for some reason, your ear thermometer doesn't include sterile covers or you've run out, then clean the tip with an antiseptic solution such as rubbing alcohol or hydrogen peroxide.[7]
- Colloidal silver is an excellent antiseptic and something you can learn to make at home, making it much more economically friendly.
- You can re-use thermometer tip covers only if you thoroughly sanitize them. Make sure to clean them after and before each use.
-
3Pull the ear back and insert the thermometer. After turning the hand-held ear thermometer on, try not to move your head (or hold your child's head still) and pull back on the top part of the ear in order to help straighten out the ear canal a little bit and make it easier to insert the tip. More specifically, if it's an adult ear, then gently pull it up and then back; if it's a child's ear, then gently pull it straight back.[8] Straightening the ear canal will help prevent injuring or irritating it with the tip of the thermometer and allow for the most accurate reading.
- Follow the directions to ensure that you insert the thermometer the correct distance into the ear canal—there's no need to touch the eardrum (tympanic membrane), because the thermometer is designed to take a remote reading.
- The ear thermometer bounces an infrared signal off of the eardrum to read the temperature, so creating a seal around the thermometer by placing it far enough into the canal is important also.
-
4Check the temperature reading on the digital display. Once the thermometer has been gently inserted into the ear canal, hold it firmly in place until the thermometer signals that it's taken a reading—typically with a beeping sound. Then, slowly and carefully remove the ear thermometer from the ear canal and read the number that's displayed digitally. Write down the temperature reading and don't rely on your memory, because a caregiver or health professional may want or need that information.
- It also makes it easier to compare readings over a specific period of time if you're monitoring a fever.
- An advantage of using an ear thermometer is that, when positioned properly, they are quick and fairly accurate.[9]
Interpreting the Results
-
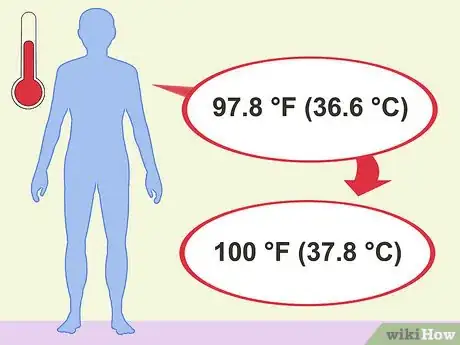
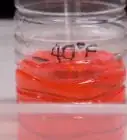
1Understand normal body temperature differences. Not every area in the body is supposed to have the same temperature at all times. For example, while the average normal oral (under the tongue) temperature of an adult is 98.6 °F (37.0 °C), ear (tympanic) temperature is typically 0.5 to 1 °F higher and can hover close to 100 °F (38 °C) and be considered normal. Furthermore, normal body temperature varies depending on gender, activity levels, food and beverage consumption, time of day, and stage of menstruation.[10] So, consider these factors if you’re trying to determine if you or someone else has a fever.
- For an adult, in reality, normal body temperature ranges from 97.8 °F (36.6 °C) to slightly under 100 °F (38 °C).
- Research indicates that temperature discrepancies as much as 1 °F in either direction can occur with ear thermometers when compared with rectal readings, the most accurate way of measuring.[11]
-
2Take multiple readings to determine if a fever exists. Due to all the factors mentioned above, and the fact that there may be some thermometer error and/or poor measuring technique, try to take multiple readings, ideally with different types of thermometers in different parts of the body. Compare all the readings and average them out. Furthermore, understand the other common indicators of mild-to-moderate fevers, such as: sweating while inactive, headache, achy muscles, weakness, loss of appetite, and increased thirst.[12]
- A single ear reading from a thermometer should not be used to determine the course of action or treatment.
- Children can be very ill without a fever, or appear normal with a temperature a little over 100 °F (38 °C). Don't make conclusions just based on numbers; look for other symptoms.
-
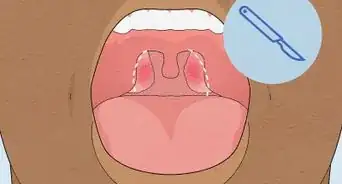
3See your doctor for a fever combined with other severe symptoms. Fevers are common symptoms of illness, but that's not usually a bad thing as they seem to play a key role in fighting infections.[13] Although an ear temperature of 100.4 °F (38.0 °C) or greater is considered a fever, if your child is older than 1 year and is drinking lots of fluids, acting playful, and sleeping normally, there's usually no reason or need to treat it. However, if they have temperatures of around 102 °F (39 °C) or greater combined with symptoms such as unusual irritability, discomfort, lethargy, and moderate-to-severe coughing and/or diarrhea, then a trip to the doctor is certainly warranted.[14]
- Symptoms of high fevers of 103–106 °F (39–41 °C) often include hallucinations, confusion, severe irritability, and convulsions. Severe fevers with these kinds of symptoms are usually considered medical emergencies.[15]
- Your doctor may recommend acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin, others) to help reduce a fever. However, ibuprofen can't be given before 6 months of age and aspirin should not be given to anyone younger than 18 years due to the risk of Reye's syndrome.
Expert Q&A
-
QuestionHow do I know if my ear thermometer is reading accurately?
 Luba Lee, FNP-BC, MSLuba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
Luba Lee, FNP-BC, MSLuba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
Board-Certified Family Nurse Practitioner If you have a new thermometer, or use one that has been properly stored and cared for, and you are practicing a good temperature taking technique, it is most likely that your thermometer is reading accurately. However, if your thermometer reads low or “normal” temperature but you feel feverish or suspect that you might have an elevated body temperature, it is a good idea to try a different thermometer.
If you have a new thermometer, or use one that has been properly stored and cared for, and you are practicing a good temperature taking technique, it is most likely that your thermometer is reading accurately. However, if your thermometer reads low or “normal” temperature but you feel feverish or suspect that you might have an elevated body temperature, it is a good idea to try a different thermometer.
Tip
- Temperature strips (which are stuck to the forehead and use liquid crystals that react to heat) are also quick and convenient, but are not as precise as ear thermometers in recording body temperature.[16]
- If you’re using an ear thermometer on an older adult or child, pull the outer edge of the ear up and back to help you guide the thermometer into the ear canal. For infants and toddlers under 3, it’s easier to gently pull the lobe down.
Warnings
- If your child develops a fever after being left in a hot car, then seek medical care immediately.⧼thumbs_response⧽
- Always insert the tip of the thermometer gently into the opening of the ear canal. Never force it in, or you could injure or damage the ear.⧼thumbs_response⧽
- The above information is not intended as medical advice. Talk to a doctor, nurse, or pharmacist if you suspect a fever.⧼thumbs_response⧽
- See your doctor if your feverish child vomits repeatedly or has a severe headache or stomachache.⧼thumbs_response⧽
- Call your doctor if your child has a fever that lasts longer than 3 days.⧼thumbs_response⧽
References
- ↑ https://medlineplus.gov/fever.html
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/measuring-a-babys-temperature
- ↑ https://www.nhs.uk/conditions/baby/health/how-to-take-your-babys-temperature/
- ↑ https://www.nhs.uk/conditions/baby/health/how-to-take-your-babys-temperature/
- ↑ http://www.mayoclinic.org/diseases-conditions/fever/in-depth/thermometers/art-20046737
- ↑ http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072538/
- ↑ https://my.clevelandclinic.org/health/articles/9959-thermometers-how-to-take-your-temperature
- ↑ http://www.drugs.com/cg/how-to-take-an-ear-temperature.html
- ↑ http://www.mayoclinic.org/diseases-conditions/fever/in-depth/thermometers/art-20046737
- ↑ https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=85&ContentID=P00866
- ↑ https://wa.kaiserpermanente.org/kbase/topic.jhtml?docId=tw9223
- ↑ http://www.mayoclinic.org/diseases-conditions/fever/basics/symptoms/con-20019229
- ↑ http://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/in-depth/thermometer/art-20047410?pg=2
- ↑ https://my.clevelandclinic.org/health/symptoms/10880-fever
- ↑ https://my.clevelandclinic.org/health/symptoms/10880-fever
- ↑ https://www.cebm.net/covid-19/accuracy-of-strip-like-forehead-thermometers/




























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...