This article was medically reviewed by Janice Litza, MD. Dr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 27,104 times.
Orthostatic hypotension, also called postural hypotension, is when your blood pressure drops when you move from sitting or lying down to standing. This can make you dizzy or lightheaded, and can even cause you to lose consciousness. Orthostatic hypotension is often nothing to worry about, but if it occurs regularly it may be a sign that you have a medical condition needing treatment.[1] Treat your orthostatic hypotension by avoiding preventable causes, treating underlying medical conditions, and making lifestyle changes. If you have dizziness with changing your position once in a while, then it is important to think about what might be causing it in your day to day activities and make adjustments.
Steps
Making Lifestyle Changes
-
1Sit or lie down when you’re dizzy. Most orthostatic hypotension is mild and resolves on its own. When you feel lightheaded, sit or lie down until it passes. You can also get into a squat position and then slowly go back to a standing position. This is often the easiest way to ease your symptoms.[2]
- Stand up slowly from sitting, lying down, or crouching.
-
2Stay hydrated. Dehydration is a common cause of low blood pressure. In general, men should drink around 13 cups of water and other fluids daily (about 3 liters), and women should aim for 9 cups (2.2 liters).[3] Drink more if you sweat a lot, work out, or live in a hot climate.
- Drink extra fluids if you have diarrhea, vomiting, or a high fever. If you’re really nauseated, try sucking on ice chips or popsicles.
- If you’re dizzy, quickly drink 2 8-ounce glasses of cold water.[4]
Advertisement -
3Stay cool in hot environments. When you exercise or go outside in hot climates, you can sweat enough to get dehydrated and lower your blood pressure. Other than hydrating well, keep yourself cool when exercising or outdoors in the heat. Try the following:
- Wear light-colored, loose-fitting clothing
- Take frequent rest breaks to drink water and cool down
- Acclimate yourself to hot environments by starting slow and increasing your activities gradually
-
4Eat more salt in your diet. Salt raises your blood pressure, so if you don’t have high blood pressure, you can increase the amount of salt that you eat to 6-10 grams daily.[5] Only do this with your doctor’s help, because too much salt can raise your blood pressure too high.
- The ideal blood pressure is 120/80.
-
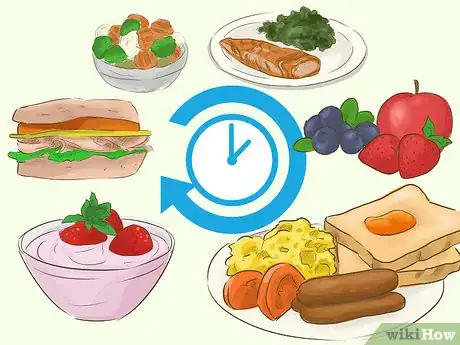
5Eat small meals that are low in carbohydrates. This is especially helpful if you tend to get dizzy after you eat.[6] Refrain from eating large amounts of bread and pasta, and focus on eating lean meats and fresh fruits and vegetables. Eat several smaller meals throughout the day instead of large meals.
-
6Stop drinking alcohol. Alcohol can increase your risk for orthostatic hypotension. If you currently drink multiple alcoholic beverages in a day, start to cut back your drinking. Consult a doctor for help or gradually limit your consumption on your own.
-
7Exercise regularly. Getting at least 30 minutes of aerobic exercise 5 days a week has many health benefits, including lowering your risk of having orthostatic hypotension. Aim to walk, run, swim, bike, play a sport, or do another physical activity on most days of the week.
- Talk to your doctor before starting a new exercise regimen if you’re not used to being active or have any medical conditions.
-
8Wear compression stockings. Compression stockings are tight, knee-high socks that limit how much blood can pool in your legs. It can be helpful to wear them if you’re on your feet a lot, or if you often sit for a long time. Your doctor can probably give you a prescription for compression stockings.[7]
- Abdominal binders can be used to accomplish a similar goal.
-
9Pump blood flow from your legs to your heart. Exercise your calf muscles before you get out of bed or stand up – squeeze the muscles tight and release them several times to improve blood flow. If you have to stand for a long time and start to feel dizzy, cross your legs like scissors and squeeze your thighs together to push blood from your legs to your heart.
- Try to avoid bending at the waist. Squat down to pick items up, instead.
- Avoid crossing your legs when you’re sitting down.[8]
-
10Elevate the head of your bed. This can help if you have chronic orthostatic hypotension. Raise the head of your bed by 10-20° or about 4 inches (10 cm).[9]
-
11Get stronger after prolonged bed rest. If you’re stuck in bed for a while due to illness or injury, you’ll probably get weaker. This can cause orthostatic hypotension when you try to stand up. Prepare for this and have someone help you stand and walk for a while, or keep something sturdy near your bed to hold onto. Try sitting up in bed regularly if you’re not allowed or able to stand.[10]
- Consider working with a physical therapist who can help you regain your strength.
Determining the Cause of the Problem
-
1Visit your doctor. It’s normal to occasionally feel dizzy when you stand up, but if it occurs frequently or lasts longer than a few seconds, see your doctor.[11] They will do a physical exam and take a medical history, check your blood pressure, and possibly do some lab tests or an ECG to try to figure out a cause.[12]
- See your doctor right away if you become so dizzy upon standing that you pass out.
-
2Get a blood test done. Often, your regular doctor can figure out what is causing your orthostatic hypotension with a blood test. They can check your blood sample to see if there’s a problem with your thyroid, adrenal gland, or nervous system, and to see if you’re anemic.
-
3Keep a diary of your symptoms. If you notice that you have symptoms of hypotension – dizziness, lightheadedness, nausea, confusion, blurry vision, weakness, or passing out – start to keep a journal. Record what symptoms you experience and how long they last. Note what you were doing right beforehand and earlier that day, such as exercising or being in the sun. Take this record with you to your doctor’s office.
- Some people get low pressure after they eat. Take note if your symptoms occur after a meal.
-
4Recognize hypotension during pregnancy. It’s normal to experience low blood pressure when you’re pregnant because of the changes your body goes through to accommodate for the baby. Usually, your blood pressure will return to normal after you give birth. Talk to your doctor about it if your symptoms last longer than a few seconds or make you so dizzy you feel like you might faint or fall.
-
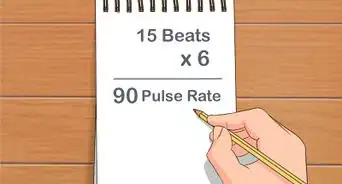
5See a cardiologist to check your heart health. Sometimes, postural hypotension can be a sign that something is wrong with how your heart is working. Valve problems, slow heart rate, heart failure, and a history of heart attack can all limit how well your heart works and cause low blood pressure when you stand up. Ask your doctor for a referral to a heart specialist, or cardiologist.
- Cardiologists can do special tests to check your heart valves and see how well your heart pumps blood.
Getting Treated Medically
-
1Stop taking medications that cause low blood pressure. Some medications can cause postural hypotension. Take a list of your medications to your doctor including any herbal supplements or beverages and ask whether stopping or switching your medicine might help with your symptoms. Never stop taking your medicine without your doctor’s supervision.
- Common medications that cause hypotension are those that treat high blood pressure and heart problems (diuretics, alpha-blockers, beta-blockers, calcium channel blockers, ACE inhibitors, and nitrates). Sometimes lowering the dose you take can ease symptoms.
- Other medications that can cause hypotension as a side effect are some antidepressants and antipsychotics, drugs for Parkinson’s disease, muscle relaxants, narcotics, and medicines for erectile dysfunction.
-
2Get a prescription for fludrocortisone (Florinef). The medication fludrocortisone raises your blood pressure by increasing how much fluid there is in your blood. For severe, persistent symptoms, this medication can be helpful.[13] See your doctor to discuss this medication, and get a prescription for it.
- Medications are only prescribed for chronic, i.e. persistent rather than occasional, orthostatic hypotension.[14]
-
3Try midodrine (ProAmatine). This medication also increases your blood pressure, making it far less likely you’ll experience orthostatic hypotension.[15] Remember that all medications may have side effects.
- Midodrine may cause you to have high blood pressure when you lie down. Discuss this risk with your healthcare provider.[16]
-
4Discuss other medication options with your doctor. If a specific disease is causing your postural hypotension, then taking the right medication may help. You doctor can prescribe one of these with other medications to treat the underlying cause:[17]
- Droxidopa (Northera) is used when Parkinson’s disease causes your orthostatic hypotension.
- Epoetin (Epogen, Procrit) can help if the problem is due to chronic anemia.
- Pyridostigmine (Regonol, Mestinon) can be helpful for those with neurological problems, and unlike midodrine it doesn’t cause hypertension when you lie down.[18]
- Nonsteroidal anti-inflammatories (NSAIDs) can be used, as well, but not if you have kidney problems.[19]
-
5Control your blood sugar. Low blood sugar and diabetes can cause hypotension. If you’re diabetic, work with your doctor, endocrinologist, or diabetes nurse to keep your blood sugar in a safe range. Low blood sugar can be just as dangerous as high blood sugar, if not more so.
- If you’re not diagnosed as diabetic but you often have postural hypotension, discuss your symptoms with your doctor and have your blood sugar and A1C checked.
References
- ↑ http://www.mayoclinic.org/diseases-conditions/orthostatic-hypotension/basics/definition/con-20031255
- ↑ http://www.mayoclinic.org/diseases-conditions/orthostatic-hypotension/basics/treatment/con-20031255
- ↑ http://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/water/art-20044256
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2888469/
- ↑ http://www.merckmanuals.com/professional/cardiovascular-disorders/symptoms-of-cardiovascular-disorders/orthostatic-hypotension
- ↑ http://www.mayoclinic.org/diseases-conditions/orthostatic-hypotension/basics/treatment/con-20031255
- ↑ http://www.mayoclinic.org/diseases-conditions/orthostatic-hypotension/basics/treatment/con-20031255
- ↑ http://my.clevelandclinic.org/health/articles/orthostatic-hypotension
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2888469/
- ↑ http://my.clevelandclinic.org/health/articles/orthostatic-hypotension
- ↑ http://www.mayoclinic.org/diseases-conditions/orthostatic-hypotension/basics/definition/con-20031255
- ↑ http://www.mayoclinic.org/diseases-conditions/orthostatic-hypotension/basics/tests-diagnosis/con-20031255
- ↑ http://www.mayoclinic.org/diseases-conditions/orthostatic-hypotension/basics/treatment/con-20031255
- ↑ http://www.aafp.org/afp/2011/0901/p527.html
- ↑ http://www.mayoclinic.org/diseases-conditions/orthostatic-hypotension/basics/treatment/con-20031255
- ↑ http://www.medscape.com/viewarticle/490777
- ↑ http://www.mayoclinic.org/diseases-conditions/orthostatic-hypotension/basics/treatment/con-20031255
- ↑ http://www.medscape.com/viewarticle/490777
- ↑ http://www.uptodate.com/contents/nsaids-and-acetaminophen-effects-on-blood-pressure-and-hypertension






















-Step-3-Version-3.webp)





















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...