This article was co-authored by Joel Warsh, MD and by wikiHow staff writer, Jessica Gibson. Dr. Joel Warsh is a board certified Pediatrician and the Owner & Founder of Integrative Pediatrics and Medicine in Los Angeles, California. With over a decade of experience, Dr. Warsh specializes in holistic and integrative medicine. He holds a Bachelor’s degree in Kinesiology and Health Sciences, a Master’s degree in Epidemiology and Community Health, and a Doctor of Medicine (MD) from Thomas Jefferson Medical College, where he was elected president of the Jefferson Pediatric Society. Dr. Warsh then completed his Pediatric Residency at Children’s Hospital of Los Angeles (CHLA), where he received the George Donnell Society Research Fellow.
This article has been viewed 17,151 times.
It's easy to feel distressed when your baby vomits. Often, whatever's causing your baby to vomit will soon work its way out of your baby's system, but you do need to keep your baby hydrated and comfortable. Pay close attention to your baby's fluid intake as well as whether or not they have a fever. Don't hesitate to get medical attention if your baby has a fever, seems overly tired, or can't keep breastmilk or formula down.
Steps
Keeping Your Baby Hydrated
-
1Wait 30 to 60 minutes before giving your baby fluids. If your baby has just thrown up, you might worry that they'll become dehydrated. Instead of giving them breastmilk or formula right away, give their stomach a little time to settle. If your baby vomits multiple times within an hour, call the doctor or nurse helpline.[1]
- Most babies won't want to eat or drink anything for a while after they throw up.
-
2Offer your baby 1 to 2 teaspoons (4.9 to 9.9 ml) of breastmilk or formula. Once you've waited a while, try to feed your baby for 5 to 10 minutes. Then see if your baby can keep it down. If they do, continue to feed 1 to 2 teaspoons (4.9 to 9.9 ml) for at least 1 to 2 hours.[2]
- If your baby can't keep the breastmilk or formula down, wait for 30 to 60 minutes before trying again.
Advertisement -
3Give your baby electrolyte solution to prevent dehydration. If your baby has vomited more than 3 times within a few hours, they may lose too much water and electrolytes. Purchase an electrolyte solution to give your baby if they're over 3 months old. If your baby is under 3 months old, get medical advice. Continue to feed your baby formula or breastmilk as well.[3]
- If your baby is over 6 months old, you can also offer 1⁄2 teaspoon (2.5 ml) of apple juice.
Electrolyte Amounts:
For a baby who's at least 6 to 7 pounds (2.7 to 3.2 kg), offer 2 cups (470 ml) of solution during a 24-hour period.
For a baby that's at least 11 pounds (5.0 kg), offer 3 cups (710 ml) of solution during a 24-hour period. -
4Feed your older baby bland foods. If your baby is over 6 months old and has already started eating solids, gradually reintroduce food. Wait to reintroduce food until your baby has kept down fluids for 8 hours. Then give a few spoonfuls of soft, bland food, such as:[4]
- Applesauce
- Pear puree
- Mashed bananas
- Infant cereal mixed with water, formula, or breastmilk
Making Your Baby Comfortable
-
1Position your baby so they're upright or on their side. If your baby is awake, hold them so they're sitting upright or cradled on their side against you. This will make it easier to keep your baby from swallowing vomit if they begin to throw up.[5]
- If you're putting your baby down to sleep, lay them on their side or back to prevent them from choking on vomit. If your baby has a birth defect, such as a cleft palate, position them on their side when putting them down.
-
2Ask your doctor before giving the baby any medication. If your baby has a fever, the doctor might recommend that you give an over-the-counter (OTC) infant fever reducer. If your baby doesn't have a fever, ask the doctor before giving an anti-nausea medication.[6]
- If your baby is under 6 months old, you should also ask before giving them an OTC infant fever reducer.
- If your baby is under 2 months and has a fever, call your doctor right away to see what they recommend.
Did You Know? You should never give aspirin to babies or children because of the risk for developing Reye's syndrome.
-
3Sing or talk to your baby in soothing tones. Your baby is probably frightened and needs extra comforting from you. Most babies prefer to be held more when they're feeling unwell, so hold your baby and walk around. While some babies might enjoy being rocked, it may make your baby feel nauseated. Talk or sing to your baby in a calm voice to help reassure them.
- If you're feeling exhausted caring for your baby, it's important to ask for help from a partner, family, or friends.
-
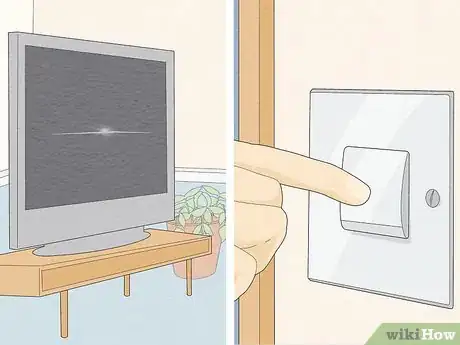
4Keep the house quiet and calm while your baby is sick. Try to limit the amount of noise and activity so your baby can feel rested during recovery. Dim the lights and play relaxing music in order to make a comfortable environment for your baby.[7]
- Avoid running loud machines or appliances if the noise seems to bother your baby.
- Since you know your baby best, you'll know when your baby is feeling better and ready to resume their usual routine.
Getting Medical Attention
-
1Track how often your baby vomits. Because so many different things can cause your baby to vomit, it's important to pay attention to how frequently your baby vomits. Write down every time your baby vomits and whether they vomited after eating. This will be valuable information for your baby's doctor.[8]
- Keep in mind that vomiting is more forceful than spitting up. There will also be more vomit than when your baby spits up.
Did You Know? Spitting up usually happens when your baby has indigestion or swallows air while eating. Your baby shouldn't be distressed by spitting up.
-
2Monitor your baby's fluid intake and number of wet diapers. If your baby vomits more than once, you'll need to ensure that your baby doesn't become dehydrated. Pay attention to how much breastmilk, formula, or water your baby is drinking and track how many wet diapers your baby has throughout the day.
- The recommended amount of fluid for your baby will depend on your baby's weight and overall health, so doctors usually ask you to track how many wet diapers they produce in a day.
- If your baby has fewer than 6 wet diapers in a 24-hour period, they're becoming dehydrated.
-
3Take your baby's temperature to check for fever. Insert a digital thermometer into your baby's ear, armpit, or rectum until it reads your baby's temperature. If your baby has a temperature of 100.4 °F (38.0 °C) or higher, they have a fever.[9]
- Because they're inaccurate, avoid using digital pacifier thermometers or fever strips.
-
4Contact the doctor if your baby vomits more than once or has a fever. You should also pay attention to any strange colors in the vomit. For example, call the doctor right away if you see blood or green in the vomit.[10]
- If your baby continues to retch without producing any vomit, contact your doctor.
- Let the doctor know if your baby is projectile vomiting.
-
5Get emergency attention if your baby is dehydrated or lethargic. It's good to seek emergency medical attention if your baby is under 3 months old and shows any signs of illness. You should also get emergency attention if your older baby suddenly seems very tired or dehydrated. Signs of dehydration include:[11]
- Listlessness
- Dry lips or mouth
- No wet diapers within 4 to 6 hours
- A sunken fontanel (soft spot on the head)
- No tears when crying
Warnings
- If your newborn experiences vomiting and fever, call the doctor right away.⧼thumbs_response⧽
References
- ↑ https://www.parents.com/health/stomach-ache/vomiting/
- ↑ https://www.parents.com/health/stomach-ache/vomiting/
- ↑ https://www.healthychildren.org/english/health-issues/conditions/abdominal/pages/treating-vomiting.aspx
- ↑ https://www.parents.com/health/stomach-ache/vomiting/
- ↑ https://www.babycenter.com/0_vomiting-in-babies_9955.bc
- ↑ https://www.babycenter.com/0_vomiting-in-babies_9955.bc
- ↑ https://www.babycentre.co.uk/x25005629/my-baby-is-vomiting-what-should-i-do
- ↑ https://www.babycenter.com/0_vomiting-in-babies_9955.bc
- ↑ https://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/in-depth/thermometer/art-20047410