This article was medically reviewed by Lacy Windham, MD. Lacy Windham, MD, is a Board-Certified Obstetrician & Gynecologist in Cleveland, Tennessee. Dr. Windham attended medical school at the University of Tennessee Health Science Center in Memphis. Her residency was completed at Eastern Virginia Medical School in Norfolk, Virginia. She was the recipient of multiple awards during her residency training, including Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, Most Outstanding Resident Overall, and Special Award in Minimally Invasive Surgery.
There are 16 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 504,736 times.
Experts say that the best birth control (also called contraceptives) for you depends on what's easiest and most comfortable for you and your partner.[1] Birth control helps you prevent pregnancy and may provide other benefits, like regular menstrual cycles. Research suggests that different contraceptives can be more effective than others, and some also help prevent sexually transmitted infections (STIs).[2] Fortunately, there's a method of birth control that works for everyone's needs, so pick the one that appeals to you.
Steps
Determining the Right Type of Birth Control
-
1Consider your family wishes and lifestyle. When you decide to use birth control, there are many factors you should consider such as if and when you want children, if you want to take pills or not worry about taking daily medication, and your lifestyle, including if you travel frequently. Thinking about these questions can help you determine the most appropriate form of birth control for you.[3]
- Make an honest assessment of yourself, your partner and your relationship. If you are not in a monogamous relationship this can also influence your choice(s) for birth control.[4] For example, if you are in a long term relationship and want to wait a few years to have children, you might opt for a long term birth control method such as an intrauterine device (IUD). If you have multiple partners, you may opt for birth control pills and condoms to protect from pregnancy and sexually transmitted diseases.[5]
- If you are in a long-term relationship, involve your partner in the decision so that you can make it mutually and it fits with both of your lifestyles.
- Consider questions such as “do I want to plan every time I have sex?,” “do I want to remember to take a pill every day?,” “do I want to end my fertility permanently?”.[6]
- You’ll also want to think about your health. For example, if you suffer from migraines, birth control pills may not be a good choice for you.
-
2Explore the different types of birth control. There are many different options for birth control that you can use. Exploring the various types of birth control can help you decide which option is appropriate for you.
- You can choose barrier methods that are put on or inserted right before sex including male and female condoms, a diaphragm, a cervical cap, and spermicide.[7]
- If used properly, these methods can help protect against pregnancy, but you may want to use a secondary method to help ensure that you don’t get pregnant. For example, if you’re using condoms, which have a failure rate of 2-18%, you may want to also use a spermicide.[8]
- Hormonal birth control, which has a low failure rate of less than 1% to 9%, are a good option if you want to avoid pregnancy and are in a long-term relationship.[9] The different types of hormonal birth control are the Pill, a patch, or a vaginal ring.[10] Birth control pills can have the added benefit that they can help regulate your menstrual cycle.[11]
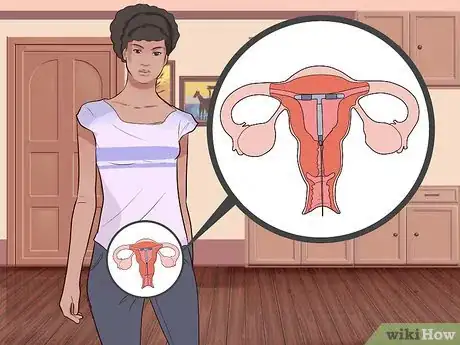
- You can choose a long-acting reversible contraception (LARC) method such as an IUD, hormonal shots, or a contraceptive implant if you want to wait to have children. It can take some time to return to fertility after using these methods, but they will not affect your ability to conceive in the long-term.[12]
- Sterilization is a birth control option if you are sure you never want children. Vasectomies and tubal ligations are generally irreversible procedures and must be seriously considered before making a final decision to go through with them.[13]
- Natural Family Planning, or NFP, avoids medications and more immediate methods such as condoms altogether. This might be a choice if you can’t use other contraceptives or simply don’t want to use other methods. However natural family planning has a high failure rate and should not be used if a pregnancy would be unacceptable. NFP includes the rhythm method, checking cervical mucus and checking basal temperature, or withdrawal.[14] These methods require a lot of planning and diligence but have the benefit of not costing anything or having side effects.[15]
Advertisement -
3Be aware of potential risks of different birth control methods. Every birth control method comes with potential risks, including unwanted pregnancy. Being aware of potential risks and side effects of the different birth control methods can help you choose the best method for you.
- Hormonal birth control, such as pills, patches, and vaginal rings increase risk of deep vein thrombosis (DVT), but decrease risk of ovarian cancer.
- Barrier methods such as condoms, spermicides, and caps can cause allergic reactions and may increase your risk for urinary tract infections or STDs.[16]
- The risks for long-acting reversible contraception (LARC) methods include perforation of the uterus, increased risk of pelvic inflammatory disease and ectopic pregnancy, and pain and heavy menstrual bleeding.[17]
- Although there are no particular medical risks to NFP, you are at an increased risk for unwanted pregnancy because this method isn’t as effective as other forms of birth control.[18]
-
4Decide on the right birth control method for you. Once you’ve had a chance to explore your different options for birth control, make an informed decision which method is right for you. Not only should you talk to your partner, but also consult with your doctor, who will need to prescribe methods such as birth control pills, LARCs, and sterilization.
Using Barrier Methods
-
1Purchase male and female condoms for use just before sex. Condoms are a thin sheath of latex (male) or plastic (female) that are either put on the penis or inserted into the vagina immediately before sexual intercourse. You don’t need to see a doctor to use this method and can start using it right away.
- You can purchase male and female condoms over the counter at most drug stores and some grocery stores.
- It’s important to make sure that you or your partner use the condom properly. This will help ensure that you don’t get pregnant or transmit any STDs.[19]
- Condoms are the only type of birth control that come with the benefit of helping to prevent STDs if used properly.[20]
-
2Insert and leave spermicide or a sponge in place before and after sex. Spermicide and sponges are barrier methods that are inserted into the vagina up to 30 minutes before sex and left in place for 6-8 hours after sex.[21] Like condoms, you don’t need to see a doctor to use spermicide and can start using it right away.
- You can purchase spermicide and sponges at most drug stores and grocery stores, and it is not very expensive.[22]
- Spermicide comes in different delivery methods such as foams, creams, jellies, thin films, and suppositories that melt when inserted into the vagina.[23]
- Sponges are doughnut shaped devices coated with spermicide. You insert a sponge yourself and it covers the cervix.[24]
-
3Get fitted for a diaphragm or cervical cap. Diaphragms and cervical caps are barrier methods made of latex, silicone, or plastic. Both are used with spermicides and require a prescription from your doctor.[25]
- Diaphragms are small dome-shaped devices that are inserted into the vagina to cover the cervix. They are made of latex or silicone and you must use it with a spermicide.[26]
- Cervical caps are also small dome-shaped devices that tightly cover the cervix using suction. They are made of plastic and you must use it with a spermicide.[27]
- Make an appointment with your doctor if you decide to get a diaphragm or cervical cap. She will fit you for a diaphragm and give you a prescription.[28]
- To start using this method, have the prescription filled. Insert your diaphragm or cervical cap 2-6 hours before sex and reapply spermicide each time you have intercourse.[29]
Choosing Hormonal Birth Control
-
1See you doctor. If you decide to use a hormonal form of birth control such as the Pill, a patch, or vaginal ring, you need to make an appointment with your doctor. She will discuss your different options and then prescribe the best choice for your health and your lifestyle.
- You must get a prescription to start birth control pills, a patch, or a vaginal ring.[30]
- There are different options for birth control pills that range from 21 day pills to 365 day pills and have different combinations of estrogen and progestin.[31] During the time that you do not take these pills, you will have your menstrual period.[32]
- The vaginal ring is a flexible plastic ring that is inserted into the vagina for 21 days. It releases hormones into your vaginal tissues and from here are carried through your body. After the 21 days, you get your period.[33]
- The contraceptive skin patch is a small adhesive patch that you apply to your skin for three consecutive weeks. You get your period the fourth week and reapply a new patch thereafter. It releases estrogen and progestin into your system through your skin.[34]
-
2Get a prescription and fill it. In order to get started using hormonal birth control, have your doctor prescribe the method you choose. You can fill this at a local pharmacy and begin using the method in most cases immediately.
- Be aware that some pharmacies will not fill hormonal birth control prescriptions for ethical reasons. Likewise, some insurance will not cover hormonal birth control, which can be expensive.
-
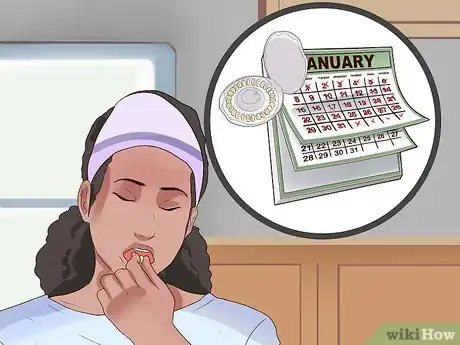
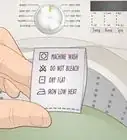
3Begin taking your hormonal birth control. Once you’ve filled your prescription, you can start using the method. If you are menstruating, you should wait until the end of your period to start these methods.
- Begin taking pills either on the day that you start your period or the Sunday after you start. If your periods are very infrequent, your doctor may recommend starting immediately.
- Until the hormonal birth control begins to regulate your cycle, it’s not uncommon to experience breakthrough bleeding and breast tenderness.[35]
-
4Use hormonal birth control consistently to prevent pregnancy. It’s important to use hormonal birth control methods consistently. Taking birth control pills daily, applying the patch or inserting the vaginal ring after four weeks can help prevent pregnancy. This will also help ensure that your cycle remains regular.[36]
- If you take the pill at the same time every day, it can help you remember to take it regularly, making it less likely that you forgot and get pregnant.
- For some pills, such as the mini-pill, it’s important to take them at the same time every day so they have maximum effectiveness.[37]
- If you travel frequently, it can be difficult to time these methods exactly. If you are unsure because of time difference when traveling, consider using a backup contraceptive method like condoms until you resume regular use of hormonal birth control.
Getting Long-Term Contraception
-
1Have an intrauterine device implanted. If you want a long acting reversible contraception, or LARC, method of birth control that doesn’t interfere with daily activities and which most women can safely use, have your doctor implant an intrauterine device. This plastic or copper T-shaped device can protect against pregnancy for 3-10 years.[38]
-
2Get contraceptive implants. Contraceptive implants stops ovulation and can help prevent pregnancy for up to 3 years.[41] Like other LARCS, your doctor must administer a contraceptive implant by inserting it under the skin of your upper arm.[42]
- The procedure to insert the contraceptive implant doesn’t require surgery or any incisions. It will only take only a few minutes for your doctor to insert this small and flexible rod with a special tool.[43]
- There is a possibility that your insurance will not cover a contraceptive implant, which can be expensive.
-
3Receive contraceptive injections. You may opt to receive contraceptive injections of the hormone depot medroxyprogesterone acetate, which can help prevent pregnancy for three months.[44]
- Your doctor will inject the hormone every 13 weeks for the most effective use. You can get the first injection any time during your cycle.[45]
- Like hormonal birth control such as the Pill, you must be consistent in getting injections. If you get your injection more than two weeks late, you will need to use a backup form of birth control.[46]
- There is a possibility that your insurance will not cover contraceptive injections, which can be expensive.
- Injections can also cause weight gain.
-
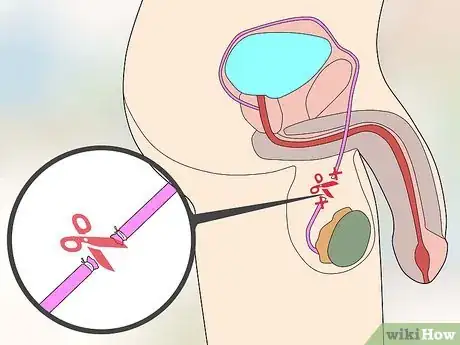
4Consider sterilization as a permanent form of birth control. If you are absolutely certain that you do not want children, consider sterilization. This form of permanent birth control is available to both men and women and requires surgery.[47]
- The only sterilization option for men is a vasectomy, which is where the tubes that carry sperm are cut and sealed. If a vasectomy is successful, a man will not be able to father a child.[48]
- Women may opt for either tubal ligation or the Essure system, which blocks the fallopian tubes. Tubal ligation, commonly called “getting your tubes tied,” requires surgery.[49]
- In general, sterilization is permanent, though in some cases it may fail.[50]
- Make sure to take proper time if deciding on sterilization since you will probably not be able to reverse the procedure.
- Be aware that some care providers will not sterilize women under a certain age.
- Be aware that insurance may not cover sterilization and it can be very expensive.
Using Natural Family Planning
-
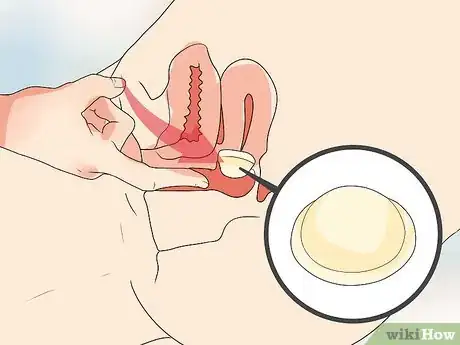
1Recognize changes in cervical mucous. The mucous present in a woman’s cervix changes consistency according to the stage of her menstrual cycle. By recognizing the changes in your cervical mucous you may be able to prevent pregnancy.[51]
- You do not need to see a doctor to use this method and can start using it immediately.[52]
- Just before ovulation, cervical mucous increases and becomes stretchy and rubbery. Just after ovulation, cervical mucous decreases and becomes thicker and less noticeable.[53]
- You’ll need to be very comfortable with your body and be extremely diligent in examining your cervical mucus to your cycle to use this method effectively.[54]
-
2Follow the Standard Days method. The Standard Days method observes the “standard rule” that a woman’s menstrual cycle averages between 26 and 32 days. Following this method will require you to avoid sexual intercourse on certain days of your cycle.[55]
-
3Measure your basal body temperature. This method holds that your basal body temperature, or your body’s temperature while resting, will increase slightly during ovulation. You’ll need to monitor your temperature every day and avoid intercourse at times if you choose to monitor your basal body temperature.[58]
- You do not need to see a doctor to use this method and can start using it immediately.[59]
- An increase of .5-1 degree Fahrenheit can indicate ovulation. If your temperature measures slightly high, you should avoid sexual intercourse to help prevent getting pregnant.[60]
- You must consistently monitor your temperature for this method to have any efficacy. For example, take your temperature every morning when you get up to use as your baseline.[61]
-
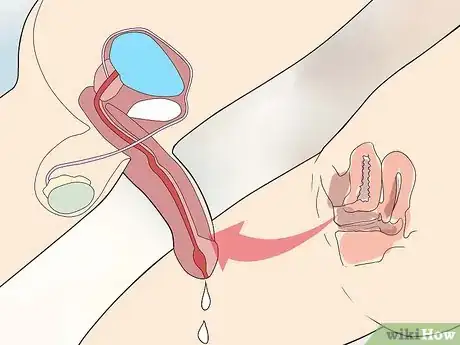
4Interrupt ejaculation by withdrawal. The withdrawal method of birth control, which is also called coitus interruptus, is when a man withdraws his penis from a woman’s vagina and away from her external genitals before ejaculation. This is generally an ineffective form of birth control and has an increased risk of pregnancy.[62]
- Coitus interruptus doesn’t require you to see a doctor and you may start it immediately.
- This method will require you and your partner to have significant self control.[63]
- Even if a man withdraws, sperm can still enter the vagina through pre-ejaculate or if the penis isn’t removed in a timely manner.[64]
Warnings
- Read any warnings that accompany any method of birth control. If you have questions, ask your doctor, health professional, or a pharmacist for further advice.⧼thumbs_response⧽
References
- ↑ https://www.mayoclinic.org/healthy-lifestyle/birth-control/in-depth/birth-control-options/art-20045571
- ↑ https://www.cdc.gov/reproductivehealth/contraception/index.htm
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/birth-control-basics/hlv-20049454
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/birth-control-basics/hlv-20049454
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/birth-control-basics/hlv-20049454
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/birth-control-basics/hlv-20049454
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/birth-control-basics/hlv-20049454
- ↑ http://www.plannedparenthood.org/learn/birth-control/condom
- ↑ http://www.plannedparenthood.org/learn/birth-control/birth-control-pill
- ↑ http://www.acog.org/Patients/FAQs/Combined-Hormonal-Birth-Control-Pill-Patch-and-Ring
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/birth-control-pills/hlv-20049454
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/seo/hlv-20049454
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/sterilization/hlv-20049454
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/natural-family-planning/hlv-20049454
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/natural-family-planning/hlv-20049454
- ↑ https://www.acog.org/Patients/FAQs/Barrier-Methods-of-Birth-Control-Spermicide-Condom-Sponge-Diaphragm-and-Cervical-Cap
- ↑ https://www.acog.org/Patients/FAQs/Long-Acting-Reversible-Contraception-Intrauterine-Device-and-Implant
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/natural-family-planning/hlv-20049454
- ↑ https://www.acog.org/Patients/FAQs/Barrier-Methods-of-Birth-Control-Spermicide-Condom-Sponge-Diaphragm-and-Cervical-Cap
- ↑ https://www.acog.org/Patients/FAQs/Barrier-Methods-of-Birth-Control-Spermicide-Condom-Sponge-Diaphragm-and-Cervical-Cap
- ↑ https://www.acog.org/Patients/FAQs/Barrier-Methods-of-Birth-Control-Spermicide-Condom-Sponge-Diaphragm-and-Cervical-Cap
- ↑ https://www.acog.org/Patients/FAQs/Barrier-Methods-of-Birth-Control-Spermicide-Condom-Sponge-Diaphragm-and-Cervical-Cap
- ↑ https://www.acog.org/Patients/FAQs/Barrier-Methods-of-Birth-Control-Spermicide-Condom-Sponge-Diaphragm-and-Cervical-Cap
- ↑ https://www.acog.org/Patients/FAQs/Barrier-Methods-of-Birth-Control-Spermicide-Condom-Sponge-Diaphragm-and-Cervical-Cap
- ↑ https://www.acog.org/Patients/FAQs/Barrier-Methods-of-Birth-Control-Spermicide-Condom-Sponge-Diaphragm-and-Cervical-Cap
- ↑ https://www.acog.org/Patients/FAQs/Barrier-Methods-of-Birth-Control-Spermicide-Condom-Sponge-Diaphragm-and-Cervical-Cap
- ↑ https://www.acog.org/Patients/FAQs/Barrier-Methods-of-Birth-Control-Spermicide-Condom-Sponge-Diaphragm-and-Cervical-Cap
- ↑ https://www.acog.org/Patients/FAQs/Barrier-Methods-of-Birth-Control-Spermicide-Condom-Sponge-Diaphragm-and-Cervical-Cap
- ↑ https://www.acog.org/Patients/FAQs/Barrier-Methods-of-Birth-Control-Spermicide-Condom-Sponge-Diaphragm-and-Cervical-Cap
- ↑ http://www.acog.org/Patients/FAQs/Combined-Hormonal-Birth-Control-Pill-Patch-and-Ring
- ↑ http://www.acog.org/Patients/FAQs/Combined-Hormonal-Birth-Control-Pill-Patch-and-Ring
- ↑ http://www.acog.org/Patients/FAQs/Combined-Hormonal-Birth-Control-Pill-Patch-and-Ring
- ↑ http://www.acog.org/Patients/FAQs/Combined-Hormonal-Birth-Control-Pill-Patch-and-Ring
- ↑ http://www.acog.org/Patients/FAQs/Combined-Hormonal-Birth-Control-Pill-Patch-and-Ring
- ↑ http://www.acog.org/Patients/FAQs/Combined-Hormonal-Birth-Control-Pill-Patch-and-Ring
- ↑ http://www.acog.org/Patients/FAQs/Combined-Hormonal-Birth-Control-Pill-Patch-and-Ring
- ↑ http://www.mayoclinic.org/tests-procedures/minipill/basics/definition/prc-20012857
- ↑ https://www.acog.org/Patients/FAQs/Long-Acting-Reversible-Contraception-Intrauterine-Device-and-Implant
- ↑ https://www.acog.org/Patients/FAQs/Long-Acting-Reversible-Contraception-Intrauterine-Device-and-Implant
- ↑ https://www.acog.org/Patients/FAQs/Long-Acting-Reversible-Contraception-Intrauterine-Device-and-Implant
- ↑ https://www.acog.org/Patients/FAQs/Long-Acting-Reversible-Contraception-Intrauterine-Device-and-Implant
- ↑ https://www.acog.org/Patients/FAQs/Long-Acting-Reversible-Contraception-Intrauterine-Device-and-Implant
- ↑ https://www.acog.org/Patients/FAQs/Long-Acting-Reversible-Contraception-Intrauterine-Device-and-Implant
- ↑ http://www.acog.org/Patients/FAQs/Progestin-Only-Hormonal-Birth-Control-Pill-and-Injection
- ↑ http://www.acog.org/Patients/FAQs/Progestin-Only-Hormonal-Birth-Control-Pill-and-Injection
- ↑ http://www.acog.org/Patients/FAQs/Progestin-Only-Hormonal-Birth-Control-Pill-and-Injection
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/sterilization/hlv-20049454
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/sterilization/hlv-20049454
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/sterilization/hlv-20049454
- ↑ http://www.mayoclinic.org/healthy-lifestyle/birth-control/basics/sterilization/hlv-20049454
- ↑ http://www.acog.org/Patients/FAQs/Fertility-Awareness-Based-Methods-of-Family-Planning
- ↑ http://www.acog.org/Patients/FAQs/Fertility-Awareness-Based-Methods-of-Family-Planning
- ↑ http://www.acog.org/Patients/FAQs/Fertility-Awareness-Based-Methods-of-Family-Planning
- ↑ http://www.acog.org/Patients/FAQs/Fertility-Awareness-Based-Methods-of-Family-Planning
- ↑ http://www.acog.org/Patients/FAQs/Fertility-Awareness-Based-Methods-of-Family-Planning
- ↑ http://www.acog.org/Patients/FAQs/Fertility-Awareness-Based-Methods-of-Family-Planning
- ↑ http://www.acog.org/Patients/FAQs/Fertility-Awareness-Based-Methods-of-Family-Planning
- ↑ http://www.acog.org/Patients/FAQs/Fertility-Awareness-Based-Methods-of-Family-Planning
- ↑ http://www.acog.org/Patients/FAQs/Fertility-Awareness-Based-Methods-of-Family-Planning
- ↑ http://www.acog.org/Patients/FAQs/Fertility-Awareness-Based-Methods-of-Family-Planning
- ↑ http://www.acog.org/Patients/FAQs/Fertility-Awareness-Based-Methods-of-Family-Planning
- ↑ http://www.mayoclinic.org/tests-procedures/withdrawal-method/basics/definition/prc-20020661
- ↑ http://www.mayoclinic.org/tests-procedures/withdrawal-method/basics/definition/prc-20020661
- ↑ http://www.mayoclinic.org/tests-procedures/withdrawal-method/basics/definition/prc-20020661








































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...