This article was medically reviewed by Jonas DeMuro, MD. Dr. DeMuro is a board certified Pediatric Critical Care Surgeon in New York. He received his MD from Stony Brook University School of Medicine in 1996. He completed his fellowship in Surgical Critical Care at North Shore-Long Island Jewish Health System and was a previous American College of Surgeons (ACS) Fellow.
There are 9 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 16,316 times.
There are many signs and symptoms that can be indicative of left ventricular heart failure. If you suspect that you may have heart failure, it is important to see a doctor immediately to receive appropriate evaluation and treatment. The diagnosis can be confirmed by a physical exam, as well as blood tests and other imaging and heart function tests.
Steps
Recognizing Common Signs and Symptoms
-
1Watch for shortness of breath.[1] One of the cardinal signs of left ventricular heart failure is shortness of breath, which often becomes worse over time. The shortness of breath is caused by less effective blood flow throughout the body (which results in less effective oxygen delivery to the tissues), as well as the pressure on the lungs as a result of the congestion in the heart (which can lead to fluid in the lungs - called pulmonary edema - and overall more difficulty breathing).
- In left ventricular heart failure, shortness of breath typically becomes worse with exertion (and improves with rest).
- Over time, you may notice that your ability to tolerate exercise decreases, and that you become short of breath faster. This may be a sign of worsening heart failure.
-
2Notice if your shortness of breath increases when you are lying down. In left ventricular heart failure, many people experience increased breathlessness when they lie down. This symptom is called "orthopnea." People often sleep in a semi-upright position, either with several pillows under their head or in a chair, to ease the sensation of shortness of breath during the night.[2]
- Another common symptom of left ventricular heart failure is called "paroxysmal nocturnal dyspnea" (PND).
- PND is when you get a sudden attack of shortness of breath in the middle of the night, that somewhat resembles an asthma attack. These episodes are generally short-lived, but they can be disruptive to sleep and they often go hand-in-hand with the diagnosis of heart failure.
Advertisement -
3Tell your doctor if you develop a cough. Another one of the hallmark signs of left ventricular heart failure is a cough. You may cough up fluid, or even blood-tinged mucus.[3]
- The cough is caused by fluid in the lungs due to the pressure exerted on the lungs from the force of congestion in the heart.
- Your cough will likely get worse with time. It will not resolve on its own, and it may be exacerbated with exercise.
-
4Observe for "palpitations." Palpitations are unusually fast heartbeats, or skipped heartbeats, leading to the sensation of being aware of your heart "doing funny things" or "fluttering" in your chest. Palpitations often accompany heart failure, and it is important to tell your doctor if you are experiencing them.[4]
-
5Consider your energy level.[5] Left ventricular heart failure is typically accompanied by fatigue and overall weakness. Again, this is due to less effective flow of blood throughout your body, and thus less efficient delivery of oxygen. It may also be due to breathing challenges from pulmonary edema (fluid in the lungs).
- You may notice your exercise tolerance decreases, followed by a decrease in your energy levels for doing day-to-day tasks around the house.
- You may find it challenging to walk up stairs, and you may feel tired, weak, and short of breath doing activities (such as walking up stairs) that you previously found easy.
-
6Look out for weight gain due to fluid retention.[6] When left ventricular heart failure progresses, it may begin to affect the right side of your heart as well, leading to concurrent right-sided heart failure. Right-sided heart failure presents with fluid retention (swelling of the ankles and legs), which in turn leads to weight gain. It is very important to tell your doctor if you are experiencing this.
-
7Be aware of the progression of your condition. Heart failure tends to be a condition that gets worse, progressively, with time. It is not a condition that improves, or gets better on its own.
- At some point, you may go into something called "decompensated heart failure."
- Decompensated heart failure is when your symptoms suddenly get worse, because your heart is no longer able to "compensate" through adaptive changes.
- If you experience a sudden worsening of your symptoms, it is key to go to the Emergency Room immediately for prompt medical evaluation and treatment.
Using Diagnostic Tests
-
1Receive a physical exam.[7] After asking you about your symptoms, the next step is for your doctor to perform a physical exam. Signs of heart failure that he or she will look for include:
- High blood pressure - this is a risk factor for heart failure.
- Abnormal heart sounds when your doctor listens to your heart with a stethoscope (doctors are trained how to pick up the signs of heart failure this way).
- A high "JVP" (jugular venous pressure), which is basically when your doctor observes fluid build-up in the veins of your neck, which often goes hand-in-hand with heart failure and similar conditions.
- Fluid build up in your legs.
- Crackles in your lungs when your doctor listens with a stethoscope, which may indicate fluid in the lungs (from pulmonary edema).
-
2Get a blood test.[8] Another step when your doctor evaluates for heart failure will be to get a blood test. There is a specific test called "BNP," which, if elevated, has a strong correlation to heart failure.
- A blood test can also be used to rule out other conditions that may present similarly to heart failure.
-
3Ask your doctor for a chest x-ray. A chest x-ray can look for signs of heart failure including fluid in the lungs and an enlarged heart. A chest x-ray can also help to rule out other conditions that may present similar.[9]
-
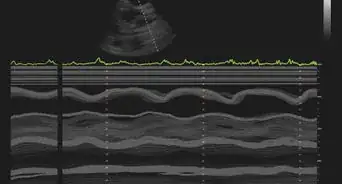
4Opt for an ECG (electrocardiogram). An ECG is a tracing of the electrical activity of your heart. It can detect things such as heart attacks, which may be the underlying reason that caused you to go into heart failure. An ECG can also be used to rule out other conditions that may present similarly to heart failure such as an arrhythmia.[10]
-
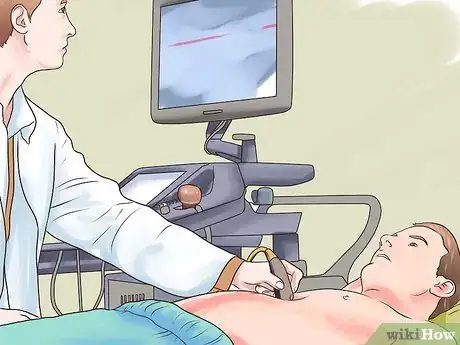
5Receive further testing as needed.[11] If the diagnosis of heart failure remains uncertain after all of these initial tests, your doctor may order further investigations. These may include:
- An echocardiogram, which can identify whether the problem is systolic or diastolic.[12]
- A stress test
- A CT or MRI
- A coronary angiogram
- A biopsy of your heart
Reducing Your Risk and Getting Treatment
-
1Quit smoking. One of the ways to reduce your risk of all types of heart disease, including left ventricular heart failure, is to quit smoking (if you currently smoke). If you are interested in quitting smoking, your doctor can support you by offering medications and/or nicotine replacement strategies to help reduce your cigarette cravings.[13]
-
2Monitor your weight. Being overweight is one of the major risk factors for various types of heart disease, including left ventricular heart failure. If you are overweight, some strategies you can try for prevention of heart disease include:[14]
- Increasing your aerobic exercise - speak to your doctor about an exercise plan that is safe for you.
- Eating a "heart-healthy diet" that is low in salt and fats, and rich in fruits, vegetables, and whole grains.
- Consuming less calories daily - in addition to your choice of foods, your quantity of food intake is also important. Ask your doctor how many calories someone with your body type should be consuming daily, and use this as a guideline to monitor (and possibly reduce) your daily caloric intake.
-
3Reduce your cardiovascular risk factors. There are many conditions which play a role in overall heart health. Identifying if you have any of these, and treating them as needed, can help to prevent left ventricular heart failure. Conditions that may increase your risk of heart disease include:[15]
- Diabetes (high blood sugar levels) - this can be treated with medications such as Metformin or Insulin.
- High blood pressure - this can be treated with medications to reduce blood pressure, such as Ramipril or Hydrochlorothiazide.
- High cholesterol - this can be decreased through dietary strategies, as well as exercise. It can also be reduced by taking medication such as Atorvastatin.
-
4Talk to your doctor about treatment options. Treatment options will vary based on your situation, so it is best to meet with your doctor and discuss your options. Some common treatment options for heart failure include:[16]
- open heart surgery to unblock and artery and improve blood flow
- percutaneous interventions to widen a valve or unblock an artery
- implanting a pacemaker to regulate your heartbeat
References
- ↑ http://www.heart.org/HEARTORG/Conditions/HeartFailure/AboutHeartFailure/Types-of-Heart-Failure_UCM_306323_Article.jsp#.Vzyafou4kXo
- ↑ https://my.clevelandclinic.org/health/diseases/22181-left-sided-heart-failure
- ↑ https://my.clevelandclinic.org/health/diseases/22181-left-sided-heart-failure
- ↑ https://www.nhs.uk/conditions/heart-palpitations/
- ↑ https://www.ucsfhealth.org/conditions/heart_failure/signs_and_symptoms.html
- ↑ http://www.heart.org/HEARTORG/Conditions/HeartFailure/AboutHeartFailure/Types-of-Heart-Failure_UCM_306323_Article.jsp#.Vzyafou4kXo
- ↑ https://my.clevelandclinic.org/health/diseases/22181-left-sided-heart-failure
- ↑ http://www.mayoclinic.org/diseases-conditions/heart-failure/basics/tests-diagnosis/con-20029801
- ↑ https://www.mayoclinic.org/diseases-conditions/heart-failure/diagnosis-treatment/drc-20373148
- ↑ https://www.mayoclinic.org/diseases-conditions/heart-failure/diagnosis-treatment/drc-20373148
- ↑ http://www.mayoclinic.org/diseases-conditions/heart-failure/basics/tests-diagnosis/con-20029801
- ↑ http://www.ncbi.nlm.nih.gov/books/NBK2218/
- ↑ https://www.mayoclinic.org/diseases-conditions/heart-failure/diagnosis-treatment/drc-20373148
- ↑ https://www.mayoclinic.org/diseases-conditions/heart-failure/diagnosis-treatment/drc-20373148
- ↑ https://medlineplus.gov/howtopreventheartdisease.html
- ↑ http://www.heart.org/HEARTORG/Conditions/HeartFailure/Recognizing-Advanced-Heart-Failure-and-Knowing-Your-Options_UCM_441926_Article.jsp#.V1HPVZErLIV





-Step-13.webp)


































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...