This article was co-authored by Tiffany Douglass, MA. Tiffany Douglass is the Founder of Wellness Retreat Recovery Center, a JCAHO (Joint Commission on Accreditation of Healthcare Organizations) accredited drug and alcohol treatment program based in San Jose, California. She is also the Executive Director for Midland Tennessee at JourneyPure. She has over ten years of experience in substance abuse treatment and was appointed a Global Goodwill Ambassador in 2019 for her efforts in residential addiction treatment. Tiffany earned a BA in Psychology from Emory University in 2004 and an MA in Psychology with an emphasis on Organization Behavior and Program Evaluation from Claremont Graduate University in 2006.
There are 13 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. This article received 11 testimonials and 100% of readers who voted found it helpful, earning it our reader-approved status.
This article has been viewed 363,040 times.
Smoking damages your lungs, reduces blood quality, affects your heart, impairs brain function, reduces fertility, and causes shortness of breath. Tobacco has been shown to cause cancer in virtually any part of the body, as well as an increased risk of cardiovascular disease and respiratory disease.[1] Quitting smoking should be the first step in controlling the effects of smoking, but there are many additional choices you can make to help reverse or slow down the damage caused by long-term smoking once you've already quit smoking. Learning how to manage the effects of smoke damage can help you feel better and live a healthier life.
Steps
Quitting Smoking
-
1Seek medical assistance. Though many people are able to quit "cold turkey," the best way to devise a treatment plan is in consultation with a medical professional. For some people, this may simply mean a brief information session with a primary care giver. For others, a more long-term treatment plan may be necessary.[2]
- Talk to your doctor about devising a smoking cessation plan that's right for you.
- Try the START method:
- S= Set a quit date.
- T= Tell friends and family members that you plan on quitting.
- A= Anticipate hard times ahead and plan for them.
- R= Remove tobacco products from the house, car, and work.
- T= Tell you Doctor so that you can get help.
-
2Join a counseling program.[3] Counseling is available through most healthcare providers. Counseling may range from individual (one-on-one) counseling sessions, group counseling sessions, or remote counseling by telephone, depending on the individual's needs and the options available through a given healthcare provider.[4]
- Some people find behavioral therapy to be an effective tool in quitting smoking.[5]
- There are a number of smartphone apps available that can help smokers quit. One such app, called quitSTART, was designed in conjunction with the U.S. Department of Health and Human Services.[6]
- You can get help by calling a free phone hotline 1-800-QUIT-NOW. You can also find many resources for quitting at www.smokefree.gov.
Advertisement -
3Try medication. There are many medication options available that can help you quit smoking. These medications range from over-the-counter options to prescription-strength medicine. Prescription medication will help reduce your cravings for tobacco and help unwanted withdrawal symptoms.[7]
- Over-the-counter options typically involve nicotine replacement products, such as the nicotine patch, nicotine gum, and nicotine lozenges.[8]
- Prescription-strength nicotine replacements are available as patches, inhalers, and nasal sprays. Other prescription medications that may help you quit smoking include bupropion SR (Zyban) and varenicline tartrate (Chantix).[9]
-
4Understand why quitting is important. Smoking cessation is the most effective way to reverse the effects of smoking. Any other plan that does not incorporate quitting tobacco will not be as effective at reducing the health impact on your body.[10] Studies have shown that quitting smoking has both immediate and long-term effects on your health. After quitting smoking, you can expect the following results[11] :
- Your heart rate and blood pressure will return to a more normal range within 20 minutes of quitting
- The carbon monoxide levels in your blood will return to a normal range within 12 hours of quitting
- Your blood circulation and lung function will improve within two weeks to three months after quitting
- Coughing and shortness of breath will decrease and cilia function will resume within one to nine months after quitting
- Your risk of coronary heart disease will drop by up to 50 percent within one year of quitting
- Your risk of mouth, throat, esophagus, and bladder cancers will drop by 50 percent within five years of quitting, your risk of cervical cancer and stroke will drop to that of a non-smoker
- Your risk of fatal lung cancer will drop by approximately 50 percent after 10 years of quitting
- Your risk of coronary heart disease returns to that of a non-smoker within 15 years of quitting
Improving Your Ability to Breathe
-
1Learn controlled breathing. If you suffer from respiratory ailments, there are a number of breathing positions and relaxation techniques that can be used to assist you when you find yourself feeling short of breath. Talk to your doctor or a qualified respiratory therapist about controlled breathing techniques to help you improve your lung function.[12]
- Sit upright. This can help increase the capacity of your lungs, which may be invaluable during times when you are short of breath.[13]
- Breathe in through the nose and out through pursed lips. This can help you find a slow, steady rhythm to regulate your breath.[14]
- Use your diaphragm to breathe. That means taking deeper, more substantial breaths, rather than the shallow breaths associated with the upper chest.[15]
- Using your diaphragm to breathe will also have the added benefit of activating the parasympathetic nervous system and relaxing you. When you are short of breath you may feel very anxious.
- Relax your neck, shoulders, and upper torso while breathing. If at all possible, have a friend or relative stand behind you and gently rub your shoulders while you sit and breathe.[16]
-
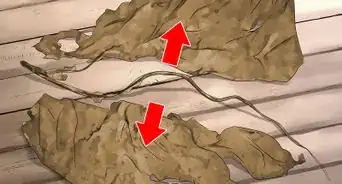
2Allow yourself to cough. Coughing is a side-effect that some people may experience in the weeks or months after giving up smoking. It may seem counter-intuitive, but coughing is actually good for your body once you've quit smoking. It helps clear irritants (including mucus) out of your lungs, which is often considered a sign that the lungs are healing.[17]
- If your coughing persists for more than a month or is accompanied by any blood, call your doctor right away, as this may be a sign of a more serious respiratory condition.[18]
-
3Reduce mucus. Many current and former smokers experience elevated levels of mucus in the lungs. To combat this, you may need to cough more frequently (unless it is painful to do so). You can also help combat mucus and airway irritation by using a humidifier in your home to moisturize the airways. You should also drink plenty of water to help keep your body hydrated each day.[19]
-
4Get plenty of exercise. For some people with respiratory problems, exercise is exhausting and difficult; however, regular exercise — especially cardiovascular exercise — has been shown to improve the respiratory muscles and provide you with stronger lungs.[20] Just don't overdo your workout or push yourself too hard.
- According to the President’s Council on Fitness, Sports, and Nutrition you should aim 150 minutes of moderate-intensity exercise each week.[21] This is equivalent to working out for 30 minutes five time a week.
- You can further break down your exercise into 10-minute increments. Any shorter than that, however, and you won't receive all the benefits.
- Moderate intensity exercise includes walking, biking slowly, gardening, using a wheelchair, and water aerobics.
-
5Maintain a healthy diet. Some people may not think of diet as a factor in respiratory health, but being overweight can put an additional strain on the lungs and may restrict breathing. Being underweight also puts you at risk of missing vital nutrients. Ask your doctor whether a healthier, more-balanced diet may help your respiratory condition.[22]
- Dietary guidelines for Americans include consuming more healthy foods like vegetables, fruits, whole grains, low fat dairy products, lean meats, and seafood. Limit sodium, saturated and trans fatty acids, and simple sugars.
Reducing the Effects of COPD
-
1Take medications. There are a number of medications available that can help reduce the effects of chronic obstructive pulmonary disease (COPD). The medication your doctor recommends will vary, depending on your symptoms and the treatment plan your doctor has devised for you.
- Bronchodilators — This class of medications is designed to relax the muscles along your airways to alleviate shortness of breath and chronic coughing. Most bronchodilators are prescribed as an aerosol inhaler, and come in short-acting forms (such as albuterol, levalbuterol, and ipratropium) and long-acting forms (such as tiotropium, salmeterol, formoterol, and arformoterol).[23]
- Inhaled steroids — These medications involve a form of corticosteroids that are inhaled to reduce inflammation of the airways. Some commonly-prescribed inhaled steroids are fluticasone (Flovent) and budesonide (Pulmicort).[24]
- Combination inhalers — These medications combine bronchodilators and inhaled steroids into a single inhaler. Some common combination inhalers include Advair, which combines salmeterol and fluticasone, and Symbicort, which combines formoterol and budesonide.[25]
- Oral steroids — This class of medication is usually prescribed to patients with moderate to severe acute exacerbation of COPD. Oral steroids are usually given in short courses that last around five days.[26] Common oral steroids for COPD exacerbation include methylprednisolone (Medrol), prednisolone (Prelone), and prednisone.[27]
- Phosphodiesterase-4 inhibitors — This medication helps reduce inflammation of the airways and relaxes the muscles that line the respiratory system. The most common phosphodiesterase-4 inhibitor is roflumilast (Daliresp).[28]
- Theophylline — This medication can help improve breathing in patients suffering from COPD and may help prevent exacerbations of COPD. Theophylline is available in a number of oral forms, including syrup, capsules, and tablets, some of which are extended release pills. Common brand names of Theophylline include Elixophyllin, Norphyl, Pyllocontin, and Quibron-T.[29]
- Antibiotics — Certain respiratory infections can cause COPD symptoms to worsen. Antibiotics can help treat exacerbations of COPD associated with respiratory infections, while some studies suggest that one particular antibiotic - azithromycin - may actually prevent exacerbations altogether.[30]
-
2Try lung therapy. There are a number of lung therapy options that can help patients suffering from moderate to severe COPD. These therapy options are designed to increase the function of a patient's lungs if COPD has made breathing difficult.
- Oxygen therapy — This option involves using a tank or portable unit of supplemental oxygen. Some patients only need supplemental oxygen use during strenuous activities or while sleeping, while others may need supplemental oxygen around the clock, depending on the severity of symptoms. Oxygen therapy is the only COPD treatment option that has been proven to extend the patient's life.[31]
- Pulmonary rehabilitation programs — This option combines training/education, exercise, nutritional guidance, and counseling. Pulmonary rehabilitation programs are designed to reduce the length of hospital stays and increase the patient's quality of life.[32]
-
3Consider surgery. Surgical options are usually reserved for patients with severe COPD and/or emphysema who have not responded to medication and traditional therapy options. Surgery usually falls into one of two treatment options:
- Lung volume reduction surgery involves a surgeon removing small portions of damaged lung tissue, allowing the healthier tissue to expand and work more efficiently. This treatment option may improve a patient's quality of life and could extend a patient's life.[33]
- Lung transplantation improves the patient's ability to breathe and resume physical activity; however, it is a very serious procedure with many possible complications and side-effects, including the risk of death. There is also a very specific set of criteria which prospective transplant recipients must meet. Talk to your doctor about whether a lung transplant may be right for you.[34]
Expert Q&A
-
QuestionHow do I cope with the effects of stopping smoking?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician You should follow the S.T.A.R.T. acronym listed in this article to cope with the effects of quitting smoking.
You should follow the S.T.A.R.T. acronym listed in this article to cope with the effects of quitting smoking. -
QuestionI quit smoking, but how can I make my lungs healthier?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician By quitting smoking you made a big step. Try to avoid air polluted areas, and choose a job that does not affect the lungs. For example, coal miners have problems with “Black Lung Disease.” Your lungs will naturally begin to heal themselves over time. Be patient and remain healthy.
By quitting smoking you made a big step. Try to avoid air polluted areas, and choose a job that does not affect the lungs. For example, coal miners have problems with “Black Lung Disease.” Your lungs will naturally begin to heal themselves over time. Be patient and remain healthy.
Warnings
- Do not reward yourself with a "celebratory smoke."⧼thumbs_response⧽
- Try not to start smoking again. Even a single cigarette will nullify all the repair which your body has done.⧼thumbs_response⧽
- Do not over-work yourself.⧼thumbs_response⧽
References
- ↑ http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/
- ↑ http://www.cdc.gov/tobacco/data_statistics/fact_sheets/cessation/quitting/index.htm
- ↑ Tiffany Douglass, MA. Substance Abuse Treatment Specialist. Expert Interview. 10 May 2020.
- ↑ http://www.cdc.gov/tobacco/data_statistics/fact_sheets/cessation/quitting/index.htm
- ↑ http://www.cdc.gov/tobacco/data_statistics/fact_sheets/cessation/quitting/index.htm
- ↑ https://smokefree.gov/tools-tips/apps/quitstart
- ↑ http://www.cdc.gov/tobacco/data_statistics/fact_sheets/cessation/quitting/index.htm
- ↑ http://www.cdc.gov/tobacco/data_statistics/fact_sheets/cessation/quitting/index.htm
- ↑ http://www.cdc.gov/tobacco/data_statistics/fact_sheets/cessation/quitting/index.htm
- ↑ http://www.cancer.org/healthy/stayawayfromtobacco/guidetoquittingsmoking/guide-to-quitting-smoking-why-quit-now
- ↑ https://www.cancer.org/healthy/stay-away-from-tobacco/benefits-of-quitting-smoking-over-time.html
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/lifestyle-home-remedies/con-20032017
- ↑ http://patient.info/health/controlled-breathing-pursed-lips-breathing
- ↑ http://patient.info/health/controlled-breathing-pursed-lips-breathing
- ↑ http://patient.info/health/controlled-breathing-pursed-lips-breathing
- ↑ http://patient.info/health/controlled-breathing-pursed-lips-breathing
- ↑ http://www.mayoclinic.org/healthy-lifestyle/quit-smoking/expert-answers/quit-smoking/faq-20057818
- ↑ http://www.mayoclinic.org/healthy-lifestyle/quit-smoking/expert-answers/quit-smoking/faq-20057818
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/lifestyle-home-remedies/con-20032017
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/lifestyle-home-remedies/con-20032017
- ↑ http://www.fitness.gov/be-active/physical-activity-guidelines-for-americans/
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/lifestyle-home-remedies/con-20032017
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/treatment/con-20032017
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/treatment/con-20032017
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/treatment/con-20032017
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/treatment/con-20032017
- ↑ http://www.webmd.com/lung/copd/corticosteroids-for-chronic-obstructive-pulmonary-disease-copd
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/treatment/con-20032017
- ↑ http://www.mayoclinic.org/drugs-supplements/theophylline-oral-route/description/drg-20073599
- ↑ http://www.mayoclinic.org/drugs-supplements/theophylline-oral-route/description/drg-20073599
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/treatment/con-20032017
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/treatment/con-20032017
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/treatment/con-20032017
- ↑ http://www.mayoclinic.org/diseases-conditions/copd/basics/treatment/con-20032017
About This Article
To reverse the effects of smoking after you've quit, try to exercise every day, even if it's just going for a walk on your lunch break, since exercise can help strengthen your lungs. Also, try to maintain a healthy diet, with plenty of vegetables, fruits, whole grains, low fat dairy products, and lean meats, which cover all of the nutrients your body needs. Additionally, avoid eating foods that are high in salt, sugar, or fat since they can put strain on your lungs. If you have a humidifier, use it in your house to moisturize your airways and reduce irritation. For more tips from our Medical co-author, including how to reduce respiratory problems with controlled breathing, read on!