This article was medically reviewed by Sarah Gehrke, RN, MS. Sarah Gehrke is a Registered Nurse and Licensed Massage Therapist in Texas. Sarah has over 10 years of experience teaching and practicing phlebotomy and intravenous (IV) therapy using physical, psychological, and emotional support. She received her Massage Therapist License from the Amarillo Massage Therapy Institute in 2008 and a M.S. in Nursing from the University of Phoenix in 2013.
There are 17 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 63,537 times.
Pelvic inflammatory disease (PID) is a bacterial infection of a woman’s reproductive organs. It often develops alongside untreated STDs like gonorrhea and Chlamydia, but can also be caused by non-sexually transmitted infections. The good news is that receiving early medical care can reduce the possibility of severe complications from PID, such as infertility. Be on the watch for any possible symptoms of PID, which include varying degrees of pelvic pain. If you suspect something, make an appointment with your doctor.[1] Follow their recommendations for treatment and you’ll be on the road to recovery.
Steps
Identifying Possible Symptoms
-
1Monitor any abdominal pain. This is usually the main symptom for women suffering from PID. The cramping and tenderness might start out as mild and build up over time or go directly into severe pain. You may feel as if you cannot move your midsection or flex it enough to stand up straight.[2]
-
2Note any changes in appetite. Along with cramps, your stomach may be upset constantly or during odd times. This may result in you vomiting up any food that is consumed. Or, you might find yourself facing nausea at the very sight of food or immediately after eating.[3]Advertisement
-
3Make note of flu-like symptoms. Coinciding with nausea, PID can trigger a high fever (over 100.4 degrees Fahrenheit) or off-and-on bouts of chills. Your fever may hold over time or come and go at random.[4]
-
4Monitor any vaginal fluids. Keep an eye on your undergarments to see if you notice any increased vaginal discharge. It might also be unusual in texture or have an unpleasant odor. Seeing heavy spotting or bleeding in between periods is another possible symptom of PID.[5]
-
5Watch for painful intercourse. If you begin to experience a sharp pain during sex or a continual dull ache afterwards, this could be a sign of PID. The pain could come on suddenly or it could slowly develop and increase in severity over time.[6]
-
6Seek emergency assistance. It’s a smart idea to head to an emergency clinic if you run a temperature of 105 °F (40.6 °C) or more, if you have a fever that stays at or rises over 103 degrees, or if you can’t keep any liquid or food down. If the pain in your abdomen turns severe, then seek out emergency treatment, too. If nothing else, they may be able to provide you with fluids and pain meds until you can be seen by your regular doctor.[7]
-
7Go in for regular check-ups. It is very possible to have PID and show no physical symptoms at all, also called being asymptomatic. Or, your symptoms may be so subtle or the pain so mild that you really don’t pay attention to them until they turn severe. Pay close attention to your body and go to regular yearly checkups with your OBGYN as a preventative measure.[8]
- If PID continues to develop unchecked, you can face some really serious medical consequences. The scarring can result in permanent infertility. It can also cause an egg to stay in the fallopian tube (not heading over to the uterus as usual), creating a potentially dangerous ectopic pregnancy. You might also suffer from lifelong severe pelvic pain.[9]
Diagnosing and Treating PID
-
1See your doctor. As soon as you suspect PID, make an appointment to talk with your OBGYN. They will ask you about your medical and sexual history and then will do a general pelvic exam. If they find that you are tender in your abdomen and around your cervix, then they will likely order additional testing. If your OBGYN is booked up, try contacting your primary care physician. You could also go to a clinic, such as Planned Parenthood.[10]
- They may order a blood test to see if your cells appear to be fighting off an infection. They may also send off cervical fluid and urine samples to be tested for STDs.[11]
- There is no one clear way to diagnose PID. That means that, unfortunately, it is often misdiagnosed as another problem with similar symptoms, such as appendicitis.[12]
- Your doctor may also recommend hospitalization as part of your treatment if you: are very ill, won’t respond to antibiotics, have an abscess, or are pregnant.
-
2Consent to an ultrasound. If your doctor believes that a PID diagnosis is possible, but needs more evidence they may request permission to complete an ultrasound, or in-depth image of your body’s interior. For example, an ultrasound can show whether or not an abscess is blocking or stretching out part of your fallopian tubes, something that is not only painful but very dangerous to your overall health.[13]
-
3Consent to laparoscopic surgery. This is a procedure where your doctor will make a small incision in your abdominal area and then insert a small, lighted camera. This will allow them to view your internal organs up close and personal. They can also take tissue samples, if needed, to conduct additional testing.[14]
- Even though it is only minimally invasive, a laparoscopic procedure is still surgery. So, you’ll want to be very clear on the possible risks and benefits before agreeing to go forward.
-
4Take all medications as directed. The most common treatment for PID is antibiotics. Because PID infections are usually quite severe and may involve a number of different harmful organisms, you’ll probably have to take at least two different types of antibiotics at once. They will come in either pill form or an in-office shot.[15]
- If you get pills, make sure to read the directions carefully and finish the entire run of the drugs, even if you start to feel better before they are finished.
- Most doctors will want you to make a follow-up appointment about three days in so they can check your progress.
-
5Notify your sexual partners. While PID is not contagious, the STDs that it often develops from, chlamydia and gonorrhea, are easily passed between sexual partners. This makes it possible for you to be cured of PID only to be infected once more. Once you’ve been diagnosed with PID, talk with your sexual partner(s) and suggest that they seek out treatment. Remember that they may not show symptoms, but still have an STD and be capable of spreading it.[16]
Knowing the Risk Factors
-
1Get tested for STDs. If you are sexually active, visit with your OBGYN each year and request STD testing. PID is very often linked with two widespread bacterial STDs, gonorrhea and chlamydia. A quick pelvic exam and a few labs can let you know whether or not you have these infections, which can make it possible to treat them before they develop into PID.[17]
-
2Be on guard after previous PID episodes. Having PID once makes it far more likely that you will contract it again. Basically, it means that your body is vulnerable to some of the types of bacteria which cause PID. So, if you’ve gotten it before, make sure to keep a close eye on any possible symptoms, using your past experiences as your guide.[18]
-
3Pay particular attention in your teens and 20s. Younger, sexually active women have an increased odds of getting PID. Their internal reproductive organs are not fully developed, which makes them easier targets for bacteria and STDs. They are also more likely to “skip” regular OBGYN appointments.[19]
-
4Practice safe sex. With every additional sex partner, your risk of getting PID or an STD grows. This is especially the case if you have sex without using a condom, as birth control will not protect you against STD and other infections. By reducing your number of partners, and having them all go for regular STD tests, you can improve your own health.[20]
-
5Stop douching. This is when you shoot water or another cleansing solution into your vaginal area in the hopes of making it cleaner. The problem here is that you can push nasty bacteria up into your reproductive organs, including your cervix, where they can take hold and give you PID. Douching may also kill off the vagina’s natural, beneficial bacteria and change the its pH balance.[21]
-
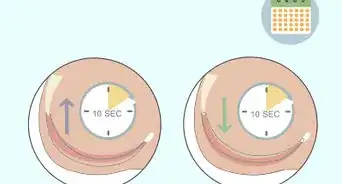
6Be watchful in the immediate period after IUD insertion. Most doctors will send you home with antibiotics following an IUD procedure, to minimize the possibility of infection. However, it is important to keep a close eye on your body for the first month or so following getting your new IUD, as this is the time when PID is most likely to develop.[22]
Warnings
- Be aware that smoking is a risk factor for PID as it compromises your immune system.[23]⧼thumbs_response⧽
- Having sex during menstruation has also been cited as a possible risk factor for PID. This is because the cervix is more open during this period and can allow the entrance of bacteria into the uterus as a result.[24]⧼thumbs_response⧽
References
- ↑ https://www.cdc.gov/std/pid/stdfact-pid-detailed.htm
- ↑ https://www.cdc.gov/std/pid/stdfact-pid.htm
- ↑ https://dph.illinois.gov/topics-services/diseases-and-conditions/diseases-a-z-list/pelvic-inflammatory-disease
- ↑ https://dph.illinois.gov/topics-services/diseases-and-conditions/diseases-a-z-list/pelvic-inflammatory-disease
- ↑ https://www.cdc.gov/std/pid/stdfact-pid.htm
- ↑ https://www.nhs.uk/conditions/pelvic-inflammatory-disease-pid/
- ↑ https://my.clevelandclinic.org/health/diseases/9129-pelvic-inflammatory-disease-pid
- ↑ https://my.clevelandclinic.org/health/diseases/9129-pelvic-inflammatory-disease-pid
- ↑ https://www.acog.org/womens-health/faqs/pelvic-inflammatory-disease?utm_source=redirect&utm_medium=web&utm_campaign=otn#
- ↑ https://www.plannedparenthood.org/learn/health-and-wellness/pelvic-inflammatory-disease-pid/how-do-i-get-tested-or-treated-pid
- ↑ https://www.plannedparenthood.org/learn/health-and-wellness/pelvic-inflammatory-disease-pid/how-do-i-get-tested-or-treated-pid
- ↑ https://www.nhs.uk/conditions/pelvic-inflammatory-disease-pid/diagnosis/
- ↑ https://www.nhs.uk/conditions/pelvic-inflammatory-disease-pid/diagnosis/
- ↑ https://www.nhs.uk/conditions/laparoscopy/why-its-done/
- ↑ https://www.cdc.gov/std/pid/treatment.htm
- ↑ https://www.cdc.gov/std/treatment-guidelines/pid.htm
- ↑ https://www.womenshealth.gov/a-z-topics/pelvic-inflammatory-disease
- ↑ https://www.nhs.uk/conditions/pelvic-inflammatory-disease-pid/complications/
- ↑ https://www.acog.org/womens-health/faqs/pelvic-inflammatory-disease
- ↑ https://medlineplus.gov/ency/article/000888.htm
- ↑ https://www.womenshealth.gov/a-z-topics/pelvic-inflammatory-disease
- ↑ https://www.womenshealth.gov/a-z-topics/pelvic-inflammatory-disease
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1695871/
- ↑ https://emedicine.medscape.com/article/256448-clinical
-Step-1-Version-2.webp)
-Step-2-Version-2.webp)
-Step-3-Version-2.webp)
-Step-4-Version-2.webp)
-Step-5.webp)
-Step-6.webp)
-Step-7.webp)
-Step-8.webp)
-Step-9.webp)
-Step-10.webp)
-Step-11.webp)
-Step-12.webp)
-Step-13.webp)
-Step-14.webp)
-Step-15.webp)
-Step-16.webp)
-Step-17.webp)
-Step-18.webp)

-Step-10-Version-4.webp)



















-Step-10-Version-4.webp)





































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...