This article was co-authored by Ni-Cheng Liang, MD. Dr. Ni-Cheng Liang is a board certified Pulmonologist and the Director of Pulmonary Integrative Medicine at Coastal Pulmonary Associates affiliated with the Scripps Health Network in San Diego, California. She also serves as a Voluntary Assistant Professor of Medicine at the University of California San Diego School of Medicine while volunteering for the UCSD Medical Student-Run Free Clinic for uninsured patients. With over 15 years of experience, Dr. Liang specializes in pulmonary and respiratory medical concerns, mindfulness teaching, physician wellness, and integrative medicine. Dr. Liang received her Doctor of Medicine (MD) from the University of Maryland School of Medicine. Dr. Liang was voted as a San Diego Top Doctor in 2017 and 2019. She was also awarded the 2019 American Lung Association San Diego Lung Health Provider of the Year.
There are 14 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. This article received 15 testimonials and 82% of readers who voted found it helpful, earning it our reader-approved status.
This article has been viewed 1,173,519 times.
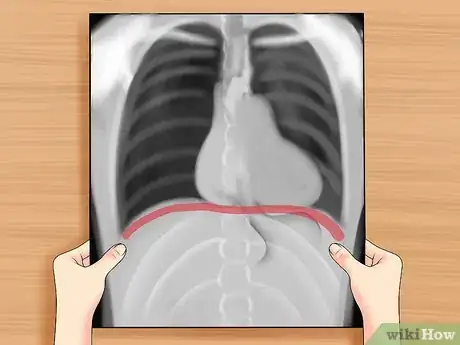
You have probably seen a chest x-ray (chest radiograph), or might even have had one taken. Have you ever wondered how to read a chest x-ray? When looking at a radiograph, remember that it is a 2-dimensional representation of a 3-dimensional object. Height and width are maintained, but depth is lost. The left side of the film represents the right side of the individual, and vice versa. Air appears black, fat appears gray, soft tissues and water appear as lighter shades of gray, and bone and metal appear white. The denser the tissue, the whiter it will appear on x-ray. Denser tissues appear radiopaque, bright on the film; less dense tissues appear radiolucent, dark on the film.
Steps
Making Initial Checks
-
1Check the patient's name. Above all else, make sure you are looking at the correct chest x-ray first. This sounds obvious, but when you are stressed and under pressure you can skip some of the basics. If you have the wrong x-ray you will be wasting time not saving it.
-
2Look up the patient's history. When you are preparing to read an x-ray make sure you have all the information on the patient, including age and sex, and their medical history. Remember to compare with old x-rays if there are any.[1]Advertisement
-
3Read the date of the radiograph. Make special note of the date when comparing older radiographs (always look at older radiographs if available). The date the radiograph is taken provides important context for interpreting any findings.
Assessing the Film Quality
-
1Check if the film was taken under full inspiration. Chest x-rays are generally taken when the patient is in the inspiratory phase of the respiration cycle, in layman's termed having breathed in. This has an important effect on the quality of the x-ray. When the x-ray beams pass through the anterior chest onto the film, it is the ribs closest to the film, the posterior ribs, that are the most apparent. You should be able to view ten posterior ribs if it was taken under full inspiration.
- If you can see 6 anterior ribs, then the film is of a very high standard.
-
2Check the exposure. Overexposed films look darker than normal, and fine details are very difficult to see. Underexposed films look whiter than normal, and cause the appearance of areas of opacification. Look for intervertebral bodies in a properly penetrated chest x-ray.
- An under-penetrated chest x-ray cannot differentiate the vertebral bodies from the intervertebral spaces.
- It is under penetrated if you can't see the thoracic vertebrae.
- An over-penetrated film shows the intervertebral spaces very distinctly.
-
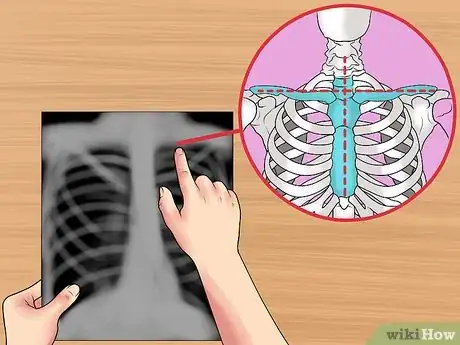
3Check for rotation. If the patient was not completely flat against the cassette, there may be some rotation evident on the x-ray. If this has happened the mediastinum can look very unusual. You can check for rotation by looking at clavicular heads and thoracic vertebral bodies.[2]
- Check that the thoracic spine aligns in the centre of the sternum and between the clavicles.
- Check if the clavicles are level.
Identifying and Aligning the X-Ray
-
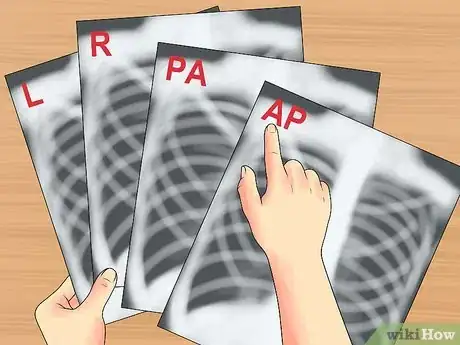
1Look for markers. The next thing to do is identify the position of the x-ray and align it correctly. Check for the relevant markers printed on the radiograph. 'L' for Left, 'R' for Right, 'PA' for posteroanterior, 'AP' for anteroposterior, etc. Note the position of the patient: supine (lying flat), upright, lateral, decubitus. Check for and mentally notate each side of the chest x-ray.
-
2Position the posteroanterior and lateral x-rays. A normal chest x-ray will consist of both posteroanterior (PA) and lateral films which are read together. Align them so they are viewed as if the patient were standing in front of you, so their right side would be facing your left.[3]
- If there are old films available you should hang these adjacent.
- The term posteroanterior (PA) refers to the direction of the x-ray traversing the patient from posterior to anterior, from back to front.
- The term antero-posterior (AP) refers to the direction of the x-ray traversing the patient from anterior to posterior, from front to back.
- The lateral chest radiograph is taken with the patient's left side of chest held against the x-ray cassette.
- An oblique view is a rotated view in between the standard front view and the lateral view. It is useful in localizing lesions and eliminating superimposed structures.
-
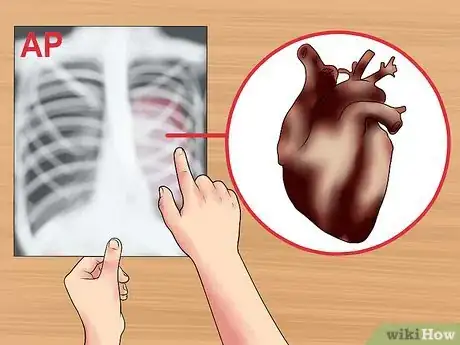
3Recognise an antero-posterior (AP) x-ray. Sometimes AP x-rays are taken, but usually only for patients who are too ill to stand up straight for the PA x-ray. AP radiographs are generally taken at shorter distance from the film compared to PA radiographs. Distance diminishes the effect of beam divergence and the magnification of structures closer to the x-ray tube, such as the heart.[4]
- Since AP radiographs are taken from shorter distances, they appear more magnified and less sharp compared to standard PA films.
- An AP film can show magnification of the heart and a widening of the mediastinum.[5]
-
4Determine if it is from a lateral decubitus position. An x-ray from this view is taken with the patient lying down on the side. It helps to assess suspected fluid (pleural effusion), and demonstrate whether the effusion is loculated or mobile.You can look at the non-dependent hemithorax to confirm a pneumothorax.
- The dependant lung should increase in density. This is due to atelectasis from the weight of the mediastinum putting pressure on it.
- If this doesn't happen it is an indicator of air trapping.[6]
-
5Align left and right. You need to make sure you are looking at it the right way. You can do this easily and quickly by looking for the gastric bubble. The bubble should be on the left.
- Assess the amount of gas and location of the gastric bubble.
- Normal gas bubbles may also be seen in the hepatic and splenic flexures of the colon.
Analyzing the Image
-
1Start with a general overview. Before you go on to focus on the specific details, it's good practice to take an overview. The major things that you might have skipped over may change the baseline normals you adopt as reference points. Beginning with this overview may also sensitize to look for particular things. Technicians often use what is called the ABCDE method: check the airway (A), bones (B), cardiac silhouette (C), diaphragm (D) and lung fields and everything else (E).[7]
-
2Check if there are any instruments such as tubes, IV lines, EKG leads, pacemaker, surgical clips, or drains.
-
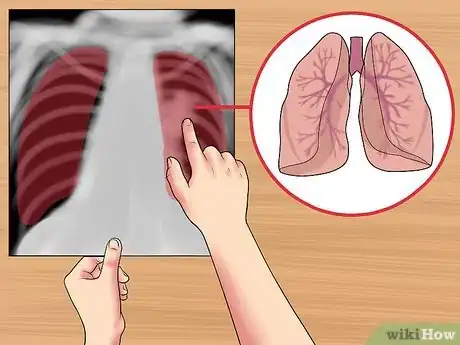
3Check the airway and lung fields. Check to see if the airway is patent and midline.[8] For example, in a tension pneumothorax, the airway is deviated away from the affected side. Look for the carina, where the trachea bifurcates (divides) into the right and left main stem bronchi. When checking the lung fields, start by checking the symmetry and look for any major areas of abnormal lucency or density. Train your eyes to peer through the heart and upper abdomen to the lung posterior. You should also be examining for vascularity, and the presence of any mass or nodules.
- Examine the lung fields for any infiltration, fluid, or air bronchograms.
- If fluid, blood, mucous, or tumor, etc. fills the air sacs, the lungs will appear radiodense (bright), with less visible interstitial markings.
-
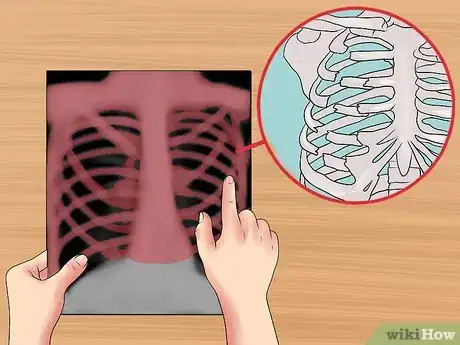
4Check the bones. Look for any fractures, lesions, or defects. Note the overall size, shape, and contour of each bone, density or mineralization (osteopenic bones look thin and less opaque), cortical thickness in comparison to medullary cavity, trabecular pattern, presence of any erosions, fractures, lytic or blastic areas. Look for lucent and sclerotic lesions.
- A lucent bone lesion is an area of bone with a decreased density (appearing darker); it may appear punched out compared to surrounding bone.[9]
- A sclerotic bone lesion is an area of bone with an increased density (appearing whiter).[10]
- At joints, look for joint spaces narrowing, widening, calcification in the cartilages, air in the joint space, and abnormal fat pads.
-
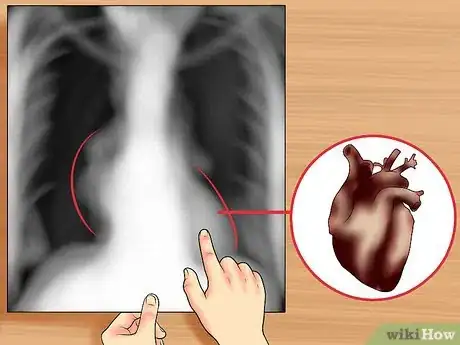
5Check the heart and look for the cardiac silhouette sign. Examine the edges of the heart; the silhouette margins should be sharp. Observe whether a radiopacity is obscuring the heart's border, in the right middle lobe and left lingula pneumonia, for example. Also, look at the external soft tissues for any abnormalities. The silhouette sign is basically the elimination of the silhouette or loss of lung/soft tissue interface, that occurs after a mass or flood in the lung.[11]
- Look at the size of the cardiac silhouette (white space representing the heart, situated between the lungs).[12] A normal cardiac silhouette occupies less than half the chest width.
- A heart with a diameter greater than half thoracic diameter is an enlarged heart.
- Note the lymph nodes, look for subcutaneous emphysema (air density below the skin), and other lesions.
- Look for water-bottle-shaped heart on PA plain film, suggestive of pericardial effusion. Get an ultrasound or chest Computed Tomography (CT) to confirm.[13]
-
6
-
7Observe the hila. Look for nodes and masses in the hila of both lungs. On the frontal view, most of the hila shadows represent the left and right pulmonary arteries. The left pulmonary artery is always more superior than the right, making the left hilum higher.
- Look for calcified lymph nodes in the hilar, which may be caused by an old tuberculosis infection.[18]
Expert Q&A
-
QuestionHow do you analyze the bones on a chest X-ray?
 Ni-Cheng Liang, MDDr. Ni-Cheng Liang is a board certified Pulmonologist and the Director of Pulmonary Integrative Medicine at Coastal Pulmonary Associates affiliated with the Scripps Health Network in San Diego, California. She also serves as a Voluntary Assistant Professor of Medicine at the University of California San Diego School of Medicine while volunteering for the UCSD Medical Student-Run Free Clinic for uninsured patients. With over 15 years of experience, Dr. Liang specializes in pulmonary and respiratory medical concerns, mindfulness teaching, physician wellness, and integrative medicine. Dr. Liang received her Doctor of Medicine (MD) from the University of Maryland School of Medicine. Dr. Liang was voted as a San Diego Top Doctor in 2017 and 2019. She was also awarded the 2019 American Lung Association San Diego Lung Health Provider of the Year.
Ni-Cheng Liang, MDDr. Ni-Cheng Liang is a board certified Pulmonologist and the Director of Pulmonary Integrative Medicine at Coastal Pulmonary Associates affiliated with the Scripps Health Network in San Diego, California. She also serves as a Voluntary Assistant Professor of Medicine at the University of California San Diego School of Medicine while volunteering for the UCSD Medical Student-Run Free Clinic for uninsured patients. With over 15 years of experience, Dr. Liang specializes in pulmonary and respiratory medical concerns, mindfulness teaching, physician wellness, and integrative medicine. Dr. Liang received her Doctor of Medicine (MD) from the University of Maryland School of Medicine. Dr. Liang was voted as a San Diego Top Doctor in 2017 and 2019. She was also awarded the 2019 American Lung Association San Diego Lung Health Provider of the Year.
Board Certified Pulmonologist Look at the ribs, shoulder bones, and neckbones to see if there's been any bone thinning, fractures, or healed fractures from before.
Look at the ribs, shoulder bones, and neckbones to see if there's been any bone thinning, fractures, or healed fractures from before. -
QuestionHow can you see fluid on a chest X ray?
 Ni-Cheng Liang, MDDr. Ni-Cheng Liang is a board certified Pulmonologist and the Director of Pulmonary Integrative Medicine at Coastal Pulmonary Associates affiliated with the Scripps Health Network in San Diego, California. She also serves as a Voluntary Assistant Professor of Medicine at the University of California San Diego School of Medicine while volunteering for the UCSD Medical Student-Run Free Clinic for uninsured patients. With over 15 years of experience, Dr. Liang specializes in pulmonary and respiratory medical concerns, mindfulness teaching, physician wellness, and integrative medicine. Dr. Liang received her Doctor of Medicine (MD) from the University of Maryland School of Medicine. Dr. Liang was voted as a San Diego Top Doctor in 2017 and 2019. She was also awarded the 2019 American Lung Association San Diego Lung Health Provider of the Year.
Ni-Cheng Liang, MDDr. Ni-Cheng Liang is a board certified Pulmonologist and the Director of Pulmonary Integrative Medicine at Coastal Pulmonary Associates affiliated with the Scripps Health Network in San Diego, California. She also serves as a Voluntary Assistant Professor of Medicine at the University of California San Diego School of Medicine while volunteering for the UCSD Medical Student-Run Free Clinic for uninsured patients. With over 15 years of experience, Dr. Liang specializes in pulmonary and respiratory medical concerns, mindfulness teaching, physician wellness, and integrative medicine. Dr. Liang received her Doctor of Medicine (MD) from the University of Maryland School of Medicine. Dr. Liang was voted as a San Diego Top Doctor in 2017 and 2019. She was also awarded the 2019 American Lung Association San Diego Lung Health Provider of the Year.
Board Certified Pulmonologist Inspect the outline of the heart to look at all the different shapes. Then, take a moment to examine the area between the diaphragm and where the diaphragm meets the chest wall. There are some little corners there that give clues to whether or not the fluid is there.
Inspect the outline of the heart to look at all the different shapes. Then, take a moment to examine the area between the diaphragm and where the diaphragm meets the chest wall. There are some little corners there that give clues to whether or not the fluid is there. -
QuestionCan TB be diagnosed with an x-ray?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician Yes. They can see granulomas (areas of inflammation, usually caused by infection) on an x-ray and use this for diagnosis.
Yes. They can see granulomas (areas of inflammation, usually caused by infection) on an x-ray and use this for diagnosis.
References
- ↑ https://www.med-ed.virginia.edu/courses/rad/cxr/interpretation1chest.html
- ↑ https://www.patientcareonline.com/view/interpreting-chest-x-rays
- ↑ http://www.med-ed.virginia.edu/courses/rad/cxr/technique1chest.html
- ↑ https://www.radiologymasterclass.co.uk/tutorials/chest/chest_quality/chest_xray_quality_projection
- ↑ https://www.radiologymasterclass.co.uk/tutorials/chest/chest_quality/chest_xray_quality_projection
- ↑ http://www.med-ed.virginia.edu/courses/rad/cxr/technique4chest.html
- ↑ Ni-Cheng Liang, MD. Board Certified Pulmonologist. Expert Interview. 18 June 2021.
- ↑ https://www.med-ed.virginia.edu/courses/rad/cxr/interpretation1chest.html
- ↑ http://www.rad.washington.edu/academics/academic-sections/msk/teaching-materials/online-musculoskeletal-radiology-book/lucent-lesions-of-bone
- ↑ http://www.rad.washington.edu/academics/academic-sections/msk/teaching-materials/online-musculoskeletal-radiology-book/sclerotic-lesions-of-bone
- ↑ https://radiopaedia.org/articles/silhouette-sign-x-rays
- ↑ Ni-Cheng Liang, MD. Board Certified Pulmonologist. Expert Interview. 18 June 2021.
- ↑ http://radiopaedia.org/articles/water-bottle-sign
- ↑ Ni-Cheng Liang, MD. Board Certified Pulmonologist. Expert Interview. 18 June 2021.
- ↑ http://radiopaedia.org/articles/flattening-of-the-diaphragm
- ↑ http://radiopaedia.org/articles/normal-position-of-diaphragms-on-chest-radiography
- ↑ http://radiologymasterclass.co.uk/tutorials/chest/chest_pathology/chest_pathology_page6.html
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2883201/
About This Article
To read a chest x-ray, start by looking for markers on it, like "L" for left, "R" for right, "PA" for posteroanterior, and "AP" for anteroposterior, to identify the positioning of the x-ray. Then, find the airway on the x-ray and check to see if it's patent and midline. You should also look at the bones to see if there are any fractures, lesions, or defects. Next, check to see if the diaphragm is flat, which could indicate emphysema, or raised, which could be a sign of pneumonia. Also, examine the heart, lung fields, cardiac silhouette, and hila. To learn how to analyze each section of a chest x-ray, keep reading!
































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...