This article was co-authored by Chris M. Matsko, MD. Dr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
This article has been viewed 31,687 times.
Learning how to accurately perform a cardiac auscultation — the action of listening to the heart with a stethoscope — is an important skill for medical students, as this procedure can help in the diagnosis of a number of major heart problems. A cardiac auscultation needs to be performed precisely, otherwise the results will not be accurate. Therefore, it's important to take your time with it and perform each step with confidence and precision.
Steps
Preparing the Patient
-
1Find an adequately lit, quiet room. A quiet room allows instant amplification of the heart sounds. This eliminates the chance of missing out on an abnormal heartbeat.[1]
- If you are a male medical professional, you may want to find a female companion before proceeding on physical examination of a female patient. The rationale behind this set-up is that a female companion will side with you if the female patient alleges that sexual harassment took place.
- This ensures the safety and professionalism of the medical professional and gives peace of mind and protection to the female patient.
- However, if the patient would rather not have someone else in the room, you should respect this.
-
2Introduce yourself and give an overview of what will take place during auscultation. Auscultation of the heart can cause anxiety for patients, especially first timers. Therefore, taking the time to inform them about what you're going to do lets the patient know what to expect during the examination and helps them to remain calm.
- This brief chat before the exam also helps to create a rapport between the patient and the medical professional and provides a sense of trust.
- Let the patient know that you'll need to ask them to remove their upper body clothing and wear a gown over their undergarments. Gowns are usually present in the examination room. Ask the physician you are working with where to find them if you are unsure.
Advertisement -
3Courteously ask the patient to remove his/her upper body clothing. Ask the patient to remove their upper body clothing and put on the gown. Tell him or her to lie down on the examination bed once they have done so. Leave the room while they undress to maintain privacy.[2]
- Warm the stethoscope with your hands as you wait. A cold stethoscope causes tightening of the skin. Tight skin will impede smooth traveling of heart sounds to the stethoscope.
- Knock before re-entering the examination room to ensure that the patient is already prepared for the exam.
Performing the Auscultation
-
1Stand at the right side of the patient. Standing at the right side makes auscultation easier.[3]
-
2Feel the patient's heart. Also known as palpation, place your right hand over the patient's left pectoral. The heel of your hand should be against the sternal border and your fingers should lie just below the nipple. You hand should lay flat against the chest, fingers extended. Make sure you tell the patient what you are going to do before you begin, and explain the purpose. While palpating, be aware of the following:[4]
- Can you feel a point of maximum impulse (PMI), which indicates the location of the left ventricle? Try to pinpoint its exact location, which is usually near the mid-clavicular line. If the ventricle is normal-sized and functioning, it should be about the size of a penny. If it is enlarged, it may be located closer to the armpit.
- What is the duration of the impulse? If the patient suffers from hypertension, the impulse will last longer. This is subtle and largely a subjective assessment, however.
- How strong is the impulse?
- Do you feel a vibration (or thrill)? If a valve is partially obstructed, you may detect this. If you notice a murmur during auscultation, then check again for a thrill.
-
3Start auscultation with the diaphragm of your stethoscope placed at the heart’s apex. The heart's apex is located about two fingerwidths below the left nipple. Gentle upward displacement of the left breast must be done in women to hear the heart sounds. Once the diaphragm of your stethoscope is in place, listen intently.[5]
- The diaphragm is the auscultatory part of the stethoscope with the wider circumference and flat surface. The diaphragm helps in auscultation of high-pitched normal heart sounds.
- There are two normal heart sounds, S1 and S2.[6] S1 corresponds to mitral and tricuspid heart valve closure during heart contraction. S2 corresponds to aortic and pulmonic valve closure during heart relaxation. S1 is louder than S2 at the apex since it is closer to the mitral valve.
-
4Listen in the other 3 auscultation spots. After auscultating the apex, it is important to listen to the following areas with your stethoscope:
- The left side of the patient's sternum, at the bottom (in the 5th intercostal space). This is the best place to auscultate the tricuspid valve.
- The left side of the patient's sternum, near the top (in the 2nd intercostal space). This is the best place to auscultate the pulmonic valve.
- The right side of the patient's sternum, near the top (in the 2nd intercostal space). This is the best place to auscultate the aortic valve.
- Note that listening to the heart's apex is the best spot to assess the mitral valve.[7]
-
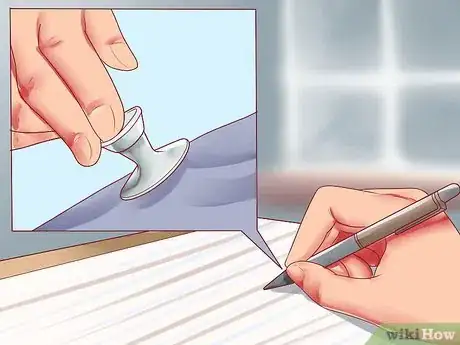
5Repeat steps 2 and 3, this time using the bell of your stethoscope. The bell is the auscultatory part of the stethoscope with the smaller circumference and concave surface. It is sensitive to abnormal heart sounds called murmurs.[8]
- The bell should be applied lightly over the skin to increase sensitivity to murmurs. Pinch the sides of the bell with your thumb and index finger. Rest the heel of your hand against the patient’s chest to ensure that the bell is placed lightly.
- The bell should create an air-tight seal with the skin to easily hear abnormal heart sounds.
-
6Ask the patient to lie on his/her left side and ensure proper draping. This position amplifies the apex’s heart sounds. Place the bell lightly on the apex and listen for murmurs.
- Ask the patient to sit up, lean forward, exhale completely and suspend breathing. This maneuver accentuates murmurs.
- Both of these maneuvers are "specialty techniques" used to better assess for any heart pathology or murmurs.
-
7Leave the examination room and allow the patient to get dressed. Do not discuss your physical examination findings with the patient still undressed.
Interpreting the Results
-
1Identify whether the cardiac rhythm is regular or irregular. While palpating the pulse, establish which sound is the first one (S1). The S1 sound is the one that is synchronized with the pulse. Then you need to establish whether the rhythm is a regular one or an irregular one, by following the S1 sound.[9]
- If the rhythm is irregular, an electrocardiogram must be taken immediately.
-
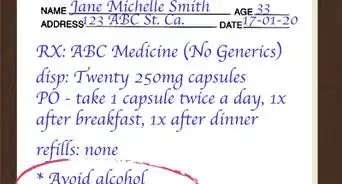
2Figure out the heart rate. By counting how many S1 sounds you hear in 10 seconds and then multiplying by 6, you will find out what the patient's heart rate is. If his resting heart rate is below 60 bpm or above 100 bpm, an electrocardiogram should also be taken and additional medication may follow.
- You need to keep in mind that sometimes a patient’s pulse may not be identical with his heartbeat, like in atrial fibrillation. For this reason, it is preferable to listen to the patient’s heart without taking his pulse when assessing his cardiac rhythm and rate.
- By counting how many sounds you hear between the S1 sounds, you can establish if it is a gallop rhythm (when you hear an extra two or even three sounds between the S1 sounds).[10] A gallop rhythm often indicates heart problems, but it is normal in children and athletes.
-
3Listen for the presence of murmurs. Murmurs are pathological heart sounds with long duration, usually lasting between either S1 to S2 or S2 to S1. "Systolic murmurs" are the ones that can be heard between S1 to S2, while "diastolic murmurs" are the ones that can be heard between S2 and S1.[11]
- Mitral insufficiency is characterized by a systolic murmur heard at the mitral area.
- Mitral stenosis is characterized by a diastolic murmur heard at the mitral area.
- Aortic insufficiency is characterized by a diastolic murmur heard at the aortic area.
- Aortic stenosis is characterized by a systolic murmur heard at the aortic area.
- Ventricular and atrial septal defects are characterized by both systolic and diastolic murmurs.
-
4Listen for gallops. A gallop is an extra heart sound that occurs following S2 (S3) or just before S1 (S4). The S3 and S4 heart sounds are best heard with the bell of the stethoscope.
- An S3 is normal in patients under 40, but in older patients it may indicate left ventricular failure. It occurs during ventricular filling and is usually due to an enlargement of the ventricular chamber.[12]
- The presence of an S3 indicates decreased contractility, myocardial failure, or volume overload of the ventricle.
- An S4 is due to decreased ventricular compliance, increased ventricular stiffness, and increased resistance. This can be heard in trained athletes or in older adults.
- Causes of S4 include hypertensive heart disease, coronary artery disease, aortic stenosis, and cardiomyopathy.
Warnings
- Cardiac auscultation requires extensive knowledge of the human anatomy, physiology, and physical examination by a medical professional. The article is intended for the use of medical professionals. Following the steps below does not necessarily lead to proper auscultation and diagnosis for non-medical professionals.⧼thumbs_response⧽
References
- ↑ https://www.sciencedirect.com/science/article/pii/B9780323392761000391
- ↑ https://meded.ucsd.edu/clinicalmed/heart.htm
- ↑ https://meded.ucsd.edu/clinicalmed/heart.htm
- ↑ https://patient.info/doctor/heart-auscultation
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK333/
- ↑ https://www.sciencedirect.com/science/article/pii/B9780323392761000391
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK333/
- ↑ https://depts.washington.edu/physdx/heart/tech.html
- ↑ https://www.msdmanuals.com/professional/cardiovascular-disorders/approach-to-the-cardiac-patient/cardiac-auscultation
About This Article
If you need to perform a cardiac auscultation, bring the patient to a quiet room and ask them to remove their upper body clothing and put on the gown. Then, leave the room so they can undress in private. Next, stand on the patient's right side and place your right hand over the left pectoral so you can feel their heartbeat, explaining what you're doing as you go. Position the stethoscope at the heart’s apex to listen to the heart. Finally, move the stethoscope to the upper and lower left side of the sternum and listen, followed by the right side of the sternum. For tips from our medical co-author on interpreting the results, read on!



















-Tube-Step-17.webp)

















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...