This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 12 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 68,369 times.
Taking care of your pancreas is incredibly important to your overall health. After a sudden bout of inflammation, or acute pancreatitis, it is doubly important. Lifestyle changes such as eating a healthy diet, losing weight, and avoiding alcohol and tobacco may reduce pain caused by chronic pancreatitis and slow progression of the disease. Your doctor may also recommend a medical treatment to help your pancreas heal or to prevent further complications.
Steps
Making Lifestyle Changes
-
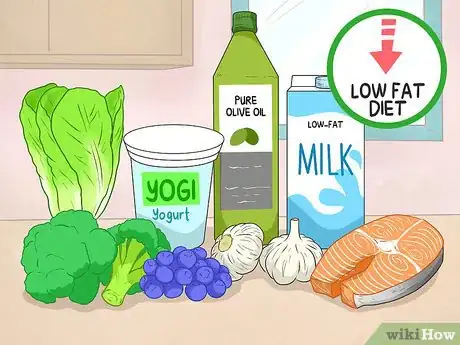
1Eat a healthy, low-fat diet. Eating a healthy diet can help reduce abdominal pain. It can also ease your pancreas’ workload, giving it an opportunity to recover from a bout of inflammation. A pancreas-friendly diet should consist of plenty of vegetables, fruits, whole grains, beans and lentils, low-fat or nonfat dairy, and lean meats. Eating small, frequent meals may also help speed your recovery.[1]
- Dark, leafy vegetables, blueberries, sweet potatoes, carrots, grapes, and walnuts are especially beneficial.
- Try to include animal-based omega-3 fats, like salmon, into your diet.[2]
- Garlic and probiotic-rich foods, such as yogurt, can help reduce inflammation and aid digestion.
- Eating a Mediterranean diet is a great way to help speed your pancreas’ recovery.
- Try to eat 6-8 small meals that are high in protein a day instead of 3 large meals.
- After pancreatitis treatment, your doctor may give you more specific information about what you should and should not eat.[3]
- Don’t go on a crash diet where you don’t eat anything to lose weight.
-
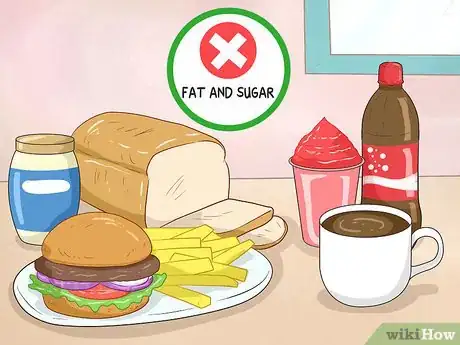
2Avoid eating foods that are high in fat and sugar. Foods high in fat and simple sugars increase levels of fat in your blood, which may increase your risk of pancreatitis. Since your pancreas processes most of the fat you eat, staying away from foods high in fat may also reduce your pancreas’ workload and speed your recovery.[4]
- Try to limit your daily fat intake to just 30 grams or less.
- Limit your consumption of red meat, organ meat, French fries, mayonnaise, butter, pastries, white bread, pasta, and sugary drinks.
- Avoid any fried, processed, or greasy foods to cut out fat.
- Try to cut caffeine from your diet if you can.
Advertisement -
3Work to lose weight, which may reduce stress on your pancreas. Your pancreas produces insulin, a hormone which controls your blood sugar levels. Obesity makes your body less sensitive to insulin, which forces your pancreas to produce more insulin to do the same amount of work.[5]
- Trying to lose weight can be difficult, but losing just 5–10 pounds (2.3–4.5 kg) may ease stress on your pancreas.
- Losing weight may also reduce your chances of getting gallstones, which are also a cause of pancreatitis.[6]
-
4Avoid excessive consumption of alcohol. To prevent damage to your pancreas, try to cut alcohol completely from your diet. If you need to, drink alcohol in moderation. This means no more than 2 drinks a day for men and just 1 drink a day for women.[7]
- If you have been diagnosed with acute or chronic pancreatitis, avoid drinking alcohol altogether.
- If you’ve been diagnosed with acute pancreatitis, continuing to drink alcohol may cause more episodes of acute pancreatitis and may lead to chronic pancreatitis.
- Drinking alcohol may cause severe complications and even death for people with chronic pancreatitis.[8]
-
5Do your best to stop smoking to reduce your risk of pancreatitis. Smoking increases the risk of getting pancreatitis, especially if coupled with drinking alcohol. If you’ve already been diagnosed with pancreatitis, it is even more important that you do your best to try to quit smoking, since doing so may make your condition even more severe.[9]
- Smoking with pancreatitis increases the risk of getting pancreatic cancer. Hence, cutting back on smoking is an important step in preventing pancreatic cancer.
- Taking enzyme supplements may improve symptoms such as fatty diarrhea, bloating, and abdominal pain.[10]
Treating Pancreatitis
-
1Seek immediate medical care if you detect signs of pancreatitis. Symptoms of severe pancreatitis include severe pain or tenderness in the abdomen, nausea and vomiting, a fever, a fast heartbeat, shortness of breath, and yellowish color of the skin or whites of the eyes. These symptoms may be caused by a serious infection, inflammation, or blockage of the pancreas.[11]
-
2Fast under the supervision of your doctor. If you visit a hospital for treatment of pancreatitis, your doctor may have you stop eating for a couple of days. This period of fasting may give your pancreas a chance to rest and recover, and it may help reduce inflammation.[12]
- After fasting, you may have to drink clear liquids and eat bland foods for a while before returning to your normal diet.
-
3Take pancreatic enzyme supplements to improve digestion. If you’re diagnosed with chronic pancreatitis, you may need to take enzyme supplements at each meal. These supplements help your body absorb nutrients in the foods you eat.[13]
- Your doctor may prescribe pancreatic enzymes for you if they believe it will help your condition.
-
4Consider gallbladder surgery if gallstones caused your pancreatitis. Gallstones are the most common cause of pancreatitis. If gallstones caused your pancreatitis, your doctor may determine that removing your gallbladder is the best way to prevent future episodes.[14]
- The surgery to remove a gallbladder is called cholecystectomy. It is a common surgery and the risk of complications is slight. You will likely be able to go home the same day as the surgery. It generally takes a week to fully recover.[15]
-
5Ask your doctor if pancreas surgery is necessary. In some severe cases, your doctor may recommend pancreas surgery. Surgery may be necessary if there is an infection in your pancreas that doesn’t respond to antibiotics. Surgery may also be required to remove scarred or diseased tissue in the pancreas. This surgery would involve either draining fluid from your pancreas or removing diseased tissue.[16]
- Pancreatic surgery is a major procedure. Your doctors will consider surgery only after exhausting other medical treatments to treat your condition.[17]
-
6Remove blockages from bile or pancreatic ducts with ERCP. Your doctor may use ERCP (endoscopic retrograde cholangiopancreatography) to remove gallstones that are blocking the bile or pancreatic ducts. Doctors may use this procedure to treat both acute and chronic pancreatitis.[18]
- ERCP may cause acute pancreatitis in some people.
References
- ↑ https://health.clevelandclinic.org/best-and-worst-foods-for-pancreatitis-pain/
- ↑ https://articles.mercola.com/pancreatitis/diet.aspx
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis/eating-diet-nutrition
- ↑ https://health.clevelandclinic.org/best-and-worst-foods-for-pancreatitis-pain/
- ↑ https://newsinhealth.nih.gov/2017/02/power-your-pancreas
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis/treatment
- ↑ https://www.mayoclinic.org/diseases-conditions/pancreatitis/diagnosis-treatment/drc-20360233
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis/treatment
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis/treatment
- ↑ https://www.uchicagomedicine.org/conditions-services/gastroenterology/pancreatitis/chronic-pancreatitis
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis/symptoms-causes
- ↑ https://www.mayoclinic.org/diseases-conditions/pancreatitis/diagnosis-treatment/drc-20360233
- ↑ https://www.mayoclinic.org/diseases-conditions/pancreatitis/diagnosis-treatment/drc-20360233
- ↑ https://www.mayoclinic.org/diseases-conditions/pancreatitis/diagnosis-treatment/drc-20360233
- ↑ https://www.mayoclinic.org/tests-procedures/cholecystectomy/about/pac-20384818
- ↑ https://www.mayoclinic.org/diseases-conditions/pancreatitis/diagnosis-treatment/drc-20360233
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4572252/
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis/treatment
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/17230607


































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...