This article was medically reviewed by Luba Lee, FNP-BC, MS and by wikiHow staff writer, Jessica Gibson. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 9 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 20,741 times.
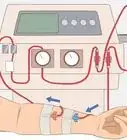
Diet is an important part of a treatment plan for chronic kidney disease.[1] Make sure to follow up with your doctor regularly to ensure you are getting the proper nutrition, as your recommended diet may change if your condition changes. Since dialysis will remove waste and fluids for your kidneys, you should cut back on minerals that could build up within your body between treatments. You'll also need to work with a renal dietitian to make adjustments to your diet. With a few simple steps, you can make dietary changes to make your dialysis treatments as effective as possible.
Steps
Before, During, and After Treatment
-
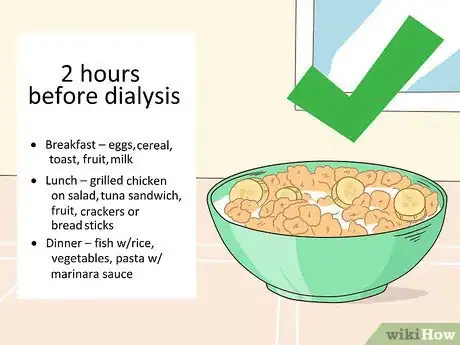
1Eat a small meal a few hours before the treatment. You should eat a meal that's easy on your stomach about 2 hours before dialysis. Choose foods that are low fat, low fiber, and high in sugar so your stomach digests it quickly. Consider eating some of these foods as part of the small meal:[2]
- Breakfast: eggs, cereal, toast, fruit, milk.
- Lunch: grilled chicken on salad, tuna sandwich, fruit, crackers, or bread sticks.
- Dinner: fish with rice, vegetables, pasta with marinara sauce.
-
2Avoid eating during dialysis. Eating while you're on dialysis can lower your blood pressure, cause nausea or vomiting, and cause cramping. Since you might have trouble swallowing, eating can increase your risk for choking. One of the biggest reasons to not eat during dialysis is because the risk for infection is high.[3]
- While your hospital space has been sanitized, there still is a possibility that bacteria in the room could be transferred through your food.
Advertisement -
3Pack a snack to eat after the treatment. You may be very hungry by the end of the dialysis treatment, so bring a snack along to eat once you leave the hospital. The snack should be small, so fill a little sandwich bag with a few of these:
- Salt-free popcorn or pretzels
- Fresh berries
- Hard-boiled egg
- Graham crackers or wafer cookies
Dietary Guidelines
-
1Create a nutrition plan with a dietitian. Your dialysis clinic should have a renal dietitian available to talk with you. You can ask your dietitian questions about specific foods, foods you should avoid, how many calories you need, and what nutrients to focus on getting in your diet. The dietitian can help you create a diet specific for your needs.[4]
- For example, you can ask, "How many calories do I need to add or cut every day?" or "How can I limit my fluids when I get thirsty?"
- You could also ask your dietitian to help you make meal plans that contain the right amount of calories.
- Your dietitian or doctor can also tell you what your ideal body weight should be. It’s a good idea to weigh yourself each morning and keep track of any changes.
-
2Take a supplement if your doctor or dietitian recommends one. You may not be getting enough vitamins and minerals because of dietary changes or dialysis itself. Ask your dietitian if you should be taking a daily vitamin and mineral supplement. Avoid taking over-the-counter supplements without talking with your dietitian because many of these will interact with your treatment.[5]
- The dietitian may recommend a vitamin and mineral supplement that's designed for people with chronic kidney disease who may not be getting as many vitamins from a restricted diet as they need.
-
3Ensure you get enough protein. It’s essential that your body gets an adequate amount of protein while you’re on dialysis. Protein will help you build muscle, fight infections, and repair tissue damage. Speak to your doctor or dietitian to find out how much protein you should eat each day.[6]
- Track what you eat each day in a diary or journal and share it with your doctor or dietitian regularly to get their input and make sure you are receiving the proper nutrition.
-
4Reduce your fluid intake. Dialysis works by removing waste and excess fluid from your body, but the treatment won't be effective if you have too much fluid. Work with your dietitian to determine how much liquid you should consume in a day. Remember that foods in a liquid state and some fruits and vegetables (such as oranges, grapes, melons, lettuce and celery) also count as fluids.[7]
- Easy ways to cut back on fluids include avoiding salty foods, measuring out your daily fluids, and eating cold fruits instead of drinking liquids.
-
5Build a support network. Realize that the nutrition plan you've made isn't just a change in diet, but a change in lifestyle. This change will usually involve your entire household if they prepare food and eat with you. Use your friends and family as a support network to help you stay on track. Get help from your support network if you find yourself struggling to follow your nutrition plan.[8]
Nutritional Adjustments
-
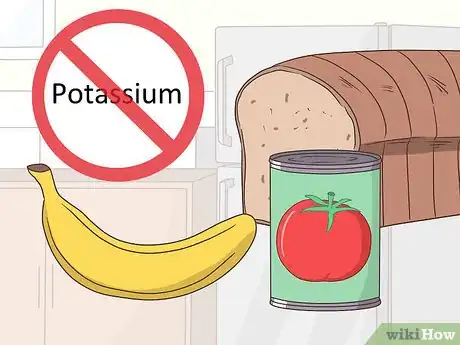
1Cut back on foods that are high in potassium. If you're on dialysis, your kidneys aren't managing mineral levels properly. Talk with your healthcare provider about keeping your potassium levels low so your nerves and muscles function correctly. Read food labels and avoid foods that contain potassium chloride. You should also try to eat smaller portions of protein during meals. For example, make healthier substitutions like:[9]
- Eating white rice, white bread, white pastas, and rice milk instead of brown rice, milk, or whole-wheat breads and pastas.
- Eating leafy greens, peppers, and green beans instead of cooked greens, tomato products, and legumes.
-
2Reduce your phosphorus intake. Your kidneys may not be able to remove phosphorus from your blood, so your doctor may prescribe a phosphorus binder for you to take with your meals and snacks. Phosphorous is a mineral that can build up in your body when you're on dialysis and cause bone damage and joint pain. To limit phosphorous in your diet:[10]
- Limit the amount of dairy (like milk, cheese, and yogurt) you eat to about 1/2 cup (120 ml). Use non-dairy substitutes to reduce your phosphorus intake.[11]
- Avoid packaged or processed foods, especially foods with vegetable oil, salt, or potatoes.
- Limit the amount of dried beans and peas you eat, such as lentils, split peas, and kidney beans.
- Reduce the amount of nuts and nut butters you eat, like peanut butter, almond butter, and mixed nuts.
- Avoid beverages like hot chocolate, beer, and dark colas.
-
3Ensure you get enough calcium. Many foods that are high in phosphorus are also high in calcium, so reducing your phosphorus intake may also reduce your calcium intake. However, calcium is an essential mineral to keep your bones healthy. Your doctor may recommend that you take calcium and/or vitamin D supplements in addition to a phosphate binder.[12]
-
4Limit your sodium intake. Your kidneys are probably struggling to filter out the mineral sodium. Too much sodium in your body can increase your blood pressure, so it's important to eat foods that are low in sodium. Ask your dietitian about eating fresh foods or meals cooked at home. Season your food with spices, herbs, and lemon instead of salt. You can also buy foods that are labeled sodium-free or no-salt added.[13]
- Avoid eating a lot of fast food, frozen packaged meals, and canned foods which are usually high in sodium.
- Cut back on salty snacks, like chips, pretzels, and crackers.
- Avoid eating take-out food as well as processed meats such as cold cuts, ham, bacon, and sausage.
References
- ↑ https://www.kidneyfund.org/kidney-disease/chronic-kidney-disease-ckd/kidney-friendly-diet-for-ckd.html
- ↑ https://www.nwkidney.org/wp-content/uploads/2014/07/Nutrition-Tips-Eating-on-Dialysis.pdf
- ↑ https://www.nwkidney.org/wp-content/uploads/2014/07/Nutrition-Tips-Eating-on-Dialysis.pdf
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis/eating-nutrition
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis/eating-nutrition
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis/eating-nutrition#protein
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis/eating-nutrition
- ↑ https://www.kidney.org/atoz/coping-effectively-guide-patients-and-their-families
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis/eating-nutrition#potassium
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis/eating-nutrition#phosphorous
- ↑ http://www.renalconsultants.com/wp-content/uploads/2014/06/nutri_chronic.pdf
- ↑ http://www.renalconsultants.com/wp-content/uploads/2014/06/nutri_chronic.pdf
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis/eating-nutrition#sodium































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...