This article was medically reviewed by Lacy Windham, MD. Lacy Windham, MD, is a Board-Certified Obstetrician & Gynecologist in Cleveland, Tennessee. Dr. Windham attended medical school at the University of Tennessee Health Science Center in Memphis. Her residency was completed at Eastern Virginia Medical School in Norfolk, Virginia. She was the recipient of multiple awards during her residency training, including Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, Most Outstanding Resident Overall, and Special Award in Minimally Invasive Surgery.
There are 18 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 59,722 times.
Studies show that hysterectomies are often recommended to those with a large uterus or a potential for an abdominal disease.[1] A hysterectomy is a surgical procedure used to remove the uterus and sometimes the ovaries. Depending upon the reason for a hysterectomy, the surgeon may decide to remove all or part of the uterus. Experts note that you should take your time when deciding whether or not to have a hysterectomy, since it's a big decision with lasting consequences.[2] Learning more about the procedure can help you feel empowered and informed as you weigh your options.
Steps
Making the Decision
-
1Find a doctor you trust. For women with sexual and reproductive health problems, a primary care physician and/or gynecologist who listens to you and pays attention to your concerns is crucial. You do not want to be rushed into the operating room by a doctor who does not take the time to hear about all of your symptoms and consider less invasive treatment options.
-
2Ask your doctor about watchful waiting. Watchful waiting is an option with some conditions, especially if you are close to menopause. Some conditions resolve as your estrogen levels reduce over time. Ask your doctor if watchful waiting is an option with your condition.[3]
- If you do not have cancer or an emergency hemorrhage, and your symptoms are mild to moderate, rather than severe or devastating, consider adopting a “wait and see” approach. This is often an effective strategy for women who have only mild symptoms and may still want to try to have children.
Advertisement -
3Try less drastic treatments first. Unless you have cancer or emergency hemorrhaging after a cesarean section, you can try other treatments first. Depending on your specific problems, these treatments might include pain medication, hormone therapy, and more targeted surgeries. For most conditions, there is no reason to rush; try these other options first.
- Your insurance and physician will likely require that you try some other treatments prior to considering surgery.
-
4Get a second opinion. If less drastic treatments do not relieve your symptoms, get a second opinion, even if you like and trust your doctor. It’s always a good idea to protect yourself by making sure that your doctor isn’t missing anything.
- If you are worried about offending your doctor, try to let go of that concern. A good doctor will understand (and even encourage!) your desire to get a second opinion.
-
5Talk to your spouse or significant other. If you have a spouse or partner, talk openly about the consequences of a hysterectomy — especially the loss of fertility, the recovery time, and, if your ovaries will be removed as well, the abrupt transition to menopause.
- Talk openly about the alternatives as well — what might it be like to live with your symptoms for a while longer? It’s vital that your significant other understands the issues involved and agrees to support you either way.
-
6See a therapist if you are feeling distraught. Deciding to have a hysterectomy is a major, life-changing decision. If you are feeling very distraught about the decision, you may wish to discuss it wit ha therapist. A therapist can help you navigate your options, examine your own feelings and concerns, and help you come to the best decision for you and your family.
- If you decide to have a hysterectomy, a therapist can also help you deal with the emotional and sexual impact of the surgery.
- If you decide not to have a hysterectomy, she can help you develop coping strategies for any pain or other symptoms you may be experiencing.
-
7Make the decision that feels best to you. On some level, you may be dissatisfied with all of your options: you may not want a hysterectomy, but, at the same time, you may feel unable to cope with your symptoms. In these cases, you may simply have to choose whichever option feels least objectionable overall.
Considering the Therapeutic Uses of a Hysterectomy
-
1Determine if a hysterectomy may be needed to remove uterine fibroids. Uterine fibroids are benign growths inside the uterus. These benign tumors are muscular and grow within the wall of the uterus. There can be a single tumor or many. They can be as small as an apple seed or grow larger than a grapefruit.[4] A hysterectomy may be necessary to remove large fibroids.
- Uterine fibroids may have a negative effect on your ability to become pregnant. Uterine fibroids may also cause excessive bleeding.
- Uterine fibroids may cause anemia due to excess blood loss during your period. As a result, you may require iron supplements or a blood transfusion.[5]
-
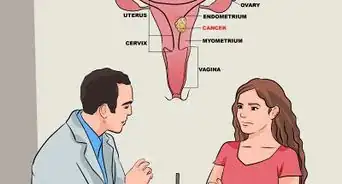
2Consider whether a hysterectomy may be a part of cancer treatment. If you are diagnosed with cancer of the uterus, cervix, or ovaries, then your physician may recommend that you have a hysterectomy. A hysterectomy will help to remove the cancer cells in your reproductive organs, which may improve the effectiveness of other treatments.
-
3Think about whether a hysterectomy may be necessary to treat endometriosis. Endometriosis causes the tissue that grows inside the uterus to begin growing on the surrounding tissues in the abdomen, such as the ovaries, fallopian tubes, the area between the vagina and rectum, the outer surface of the uterus, and the ligaments that support the uterus. A hysterectomy may be required to stop the excess tissue growth.[6]
- Tissue may also grow on the cervix, vulva, bladder, bowel, and in abdominal surgical scars.
- If left untreated, endometriosis may cause lesions, inflammation, pain, scar tissue, infertility, and bowel problems.
-
4Decide if a hysterectomy is the best option to stop abnormal bleeding. Abnormal vaginal bleeding is often the result of an underlying medical condition. Some causes of abnormal bleeding include fibroids, cancer, infection, changes in hormone levels, endometriosis, Polycystic Ovary Disease (PCOS), Pelvic Inflammatory Disease (PID), sexual abuse, hyperthyroidism, and diabetes.
- Depending upon the underlying condition and whether it can be controlled with medication or lifestyle changes, your physician may recommend a hysterectomy to prevent excessive blood loss each month.[7]
-
5Compare your options to treat a uterine prolapse. Uterine prolapse means that the uterus or womb has sagged or slipped out of its normal position. After diagnosis, your physician may recommend a surgical option of either a hysterectomy or uterine suspension. In a uterine suspension, the uterus is put back in place and suspended with a sling like apparatus or reattached to the back of the uterus.[8]
- When a prolapse happens, the uterus may even drop partway through the vagina. This creates a lump or bulge.
- Take steps to prevent uterine prolapse if you think you may be at risk.
-
6Determine if a hysterectomy is the best option for treating adenomyosis. Adenomyosis affects the inner lining of the uterus, also known as the endometrium. Adenomyosis can cause severe menstrual cramping, lower abdominal pressure, bloating, and heavy periods. The condition can affect the entire uterus or just one spot.
- Even though adenomyosis not life-threatening, the condition can have a negative effect on a woman’s quality of life. Hysterectomy is one of the options for treating adenomyosis.[9]
- Hysterectomy is often the best choice for this condition, but it can be delayed if you wish to have more children.
-
7Ask your doctor about dilation and curettage for polyps. A hysterectomy may be necessary to remove polyps if they are too large to be removed using dilation and curettage. Polyps can develop in the lining of the uterus and cause irregular bleeding. Polyps are not often cancerous and can often be removed through the vagina when they are near the opening of the cervix.[10]
- If your doctor has recommended a hysterectomy to remove polyps, ask if performing a dilation and curettage may be possible instead.
Understanding Alternatives to a Hysterectomy
-
1Find out if you are a candidate for a myomectomy. A myomectomy removes fibroids using laparoscopic surgery. In this procedure, the surgeon removes fibroids from the uterus through the navel or through the vagina and cervix. Both approaches are less invasive and less expensive than a hysterectomy.
-
2Discuss the possibility of hormone therapy for your condition. Hormone therapy may be a short-term option for treating uterine fibroids, but surgery is still required. Your doctor may recommend medications to shrink the size of uterine fibroids in preparation for surgery. The fibroids will grow back if they are not removed.[11]
- Some hormone medications block the production of estrogen, which can reduce symptoms. Other medications can be included to control pain and other symptoms.
-
3Explore endometrial ablation as an option. Endometrial ablation is a technique that removes the lining of the uterus, but also causes infertility. There are some variations on this method as well, including thermal balloon ablation, cryoablation and radiofrequency ablation.
- All forms of ablation cause infertility but are much less invasive and have faster recovery time than a hysterectomy. They each have success rates between 80 and 90 percent.[12]
- Be aware that this procedure is not a substitution for sterilization or contraception. Pregnancies absolutely occur after ablation, but they cannot be carried for long.
-
4Consider Kegel exercises for uterine prolapse. Uterine prolapse may respond to Kegel exercises because they help to strengthen the pelvic floor if they are not severe.[13] All women should start doing Kegel exercises when they reach their 40’s or after having their first child.
- Kegel exercises improve the strength of the pelvic floor, reduce the possibility of leaking urine while laughing or sneezing, and increase the strength of orgasm contractions.
-
5Ask about a pessary device. A pessary device may also be useful for a uterine prolapse. A pessary device is a plastic device that is placed in the vagina to help support the uterus and bladder without undergoing any surgery.[14]
- Your physician may also recommend a pessary device if you have urinary incontinence from bladder weakness.[15]
- You can remove and clean a pessary device.
- A pessary device may cause you to produce more vaginal secretions.
- Some pessary devices can be left in place during intercourse, but most cannot. Ask your physician about your options.
-
6Discuss birth control with your doctor. Ask your doctor if birth control pills might improve your condition. Birth control pills can be used to help reduce large amounts of blood loss during your menstrual period. They may be used to treat endometriosis and chronic pelvic pain as well.[16]
-
7Explore other treatments for abnormal bleeding. If a hysterectomy has been suggested to treat abnormal bleeding, ask your doctor about other treatments that might solve the problem. Other treatments that may be used to treat abnormal bleeding can include a dilation and curettage (D&C), hormonal medications such as progestins and oral contraception, or placement of a progesterone intrauterine device (IUD) to decrease the rate of bleeding and reduce pain.[17]
- A progesterone IUD can prevent hysterectomies in many patients.
-
8See if uterine artery embolization would help. Uterine artery embolization (UAE) reduces the size and blood supply to fibroid tissues growing in the uterus. Once the blood supply is blocked, the fibroids will shrink and die. Although this procedure is less invasive and has a quicker recovery time than a hysterectomy, it also causes infertility.[18] There is also a chance that it will trigger premature menopause, and it can be very painful for a day or two following the procedure.
Knowing What to Expect After Surgery
-
1Be prepared to give yourself time to recover. If you choose to undergo a hysterectomy it is important to understand the recovery period. There are several things that you will need to keep in mind as you recover from the surgery:[19]
- You may experience burning or itching around the incision or a numb feeling around the incision and down one leg. This may be present for up to two months after surgery.[20]
- You will be able to resume eating your normal diet after the surgery as long as you are able to tolerate it.
- You will be able to shower or bathe but should keep the area clean and dry otherwise.
- The area around the incision can be itchy. You can use lotions or creams to help relieve the itching.
- It is important to increase your activity level each day as long as you feel capable and aren’t in pain.
- Make sure to speak with your doctor about when you’ll be released to drive. Do not drive when taking pain medication.
- Avoid lifting anything heavier than 10 pounds for four weeks after surgery.
- Avoid any vigorous exercise for four weeks after surgery
- You should be able to go back to work between three and six weeks afterward.
-
2Know that your menstrual periods will stop after a hysterectomy. However, if the ovaries remain then you will continue to experience some hormonal changes to your body, including bloating and other symptoms that were normal for you while menstruating. You might even experience light vaginal bleeding for about four to six weeks after surgery.[21]
- If the ovaries were also removed you’ll experience more sudden symptoms of menopause. You experience hot flashes, emotional ups and downs, vaginal dryness, irritability, increased number of headaches or insomnia. Your physician may prescribe hormone replacement therapy initially to help your body ease into menopause more naturally as it would have if your ovaries had been left intact.[22]
-
3Keep in mind that you can still have sex. A hysterectomy will not affect your ability to enjoy sex. Your sexual desire and drive should not change unless the ovaries are also removed, which will put your body into menopause right away. Removing the ovaries will decrease sexual drive and increase vaginal dryness.[23]
- Even though a hysterectomy should not affect a woman’s sex drive, some women find that the emotional aspects of undergoing a hysterectomy have an effect on sexual desire and drive.
- Your physician will advise you to abstain from sexual intercourse, using tampons, or douching for four to six weeks after surgery or until you have fully healed.
-
4Consider the emotional repercussions. The emotional effects of this surgery will vary from woman to woman. You may feel freer and no longer worry about an unplanned pregnancy, or you may grieve the permanent loss of your period and ability to bear children.[24] Both of these responses are normal.
- If feelings of sadness continue for longer than two weeks after surgery, talk with your surgeon or primary care physician.
-
5Be aware that you may have some weight gain after surgery. Some women also discover that they gain weight after a hysterectomy. Along with this, you may have more trouble sleeping and be more irritable after the surgery. However, with good nutrition, exercise and stress reduction techniques, you can often lose weight and alleviate these other symptoms.[25]
References
- ↑ https://www.mayoclinic.org/tests-procedures/abdominal-hysterectomy/about/pac-20384559
- ↑ https://www.womenshealth.gov/a-z-topics/hysterectomy
- ↑ http://www.womenshealth.gov/publications/our-publications/fact-sheet/hysterectomy.html
- ↑ http://www.womenshealth.gov/publications/our-publications/fact-sheet/uterine-fibroids.html
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/uterine-fibroids
- ↑ http://www.endometriosisassn.org/endo.html
- ↑ https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/hysterectomy#reasons-for-a-hysterectomy
- ↑ https://my.clevelandclinic.org/health/diseases_conditions/hic_Uterine_Prolapse
- ↑ https://www.nhs.uk/conditions/hysterectomy/why-its-done/
- ↑ https://www.womenshealthnetwork.com/hysterectomy/vaginal-and-partial-hysterectomy-options/
- ↑ https://www.mayoclinic.org/diseases-conditions/uterine-fibroids/diagnosis-treatment/drc-20354294
- ↑ https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/endometrial-ablation
- ↑ http://www.womenshealth.gov/publications/our-publications/fact-sheet/hysterectomy.html
- ↑ https://my.clevelandclinic.org/health/treatments_and_procedures/hic-alternatives-to-hysterectomy
- ↑ http://familydoctor.org/familydoctor/en/drugs-procedures-devices/procedures-devices/vaginal-pessary.html
- ↑ https://youngwomenshealth.org/2011/10/18/medical-uses-of-the-birth-control-pill/
- ↑ https://my.clevelandclinic.org/health/treatments_and_procedures/hic-alternatives-to-hysterectomy
- ↑ http://www.womenshealth.gov/publications/our-publications/fact-sheet/hysterectomy.html
- ↑ https://my.clevelandclinic.org/health/treatments_and_procedures/hic_What_You_Need_to_Know_About_Hysterectomy
- ↑ https://my.clevelandclinic.org/health/treatments_and_procedures/hic_What_You_Need_to_Know_About_Hysterectomy
- ↑ https://my.clevelandclinic.org/health/treatments_and_procedures/hic_What_You_Need_to_Know_About_Hysterectomy
- ↑ https://my.clevelandclinic.org/health/treatments_and_procedures/hic_What_You_Need_to_Know_About_Hysterectomy
- ↑ https://my.clevelandclinic.org/health/treatments_and_procedures/hic_What_You_Need_to_Know_About_Hysterectomy
- ↑ http://www.upmc.com/patients-visitors/education/womens-health/Pages/hysterectomy.aspx
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2851125/
































-Step-11.webp)




















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...