This article was co-authored by Mohammad Dar, MD. Dr. Mohammad Dar (MoDar) is a board certified Internist based in Boston, Massachusetts. With over seven years of experience in the medical field, he is skilled in epidemiology, healthcare, and health policy. Dr. Dar has had a myriad of experiences in healthcare, including working on the implementation of the Affordable Care Act at the White House Office of Health Reform, volunteering in rural Uganda with public health initiatives, and leading policy and on-the-ground COVID-19 operations during the pandemic. He has also worked on a number of innovative public health and insurance reform initiatives in Massachusetts. Dr. Dar received a BS in Cell and Molecular Biology and History from The University of Michigan and an MD from The University of Michigan Medical School. He completed his residency training at Harvard Medical School and Brigham and Women’s Hospital, from which he received the Golden Stethoscope Award.
There are 13 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 35,884 times.
FSGS or (Focal Segmental Glomerulosclerosis) is a rare condition which attacks the filtering system of the kidneys and leads to serious scarring. FSGS is also responsible for a more serious disease called Nephrotic Syndrome. The relationship between Focal Segment Glomerulosclerosis and Gout is simple. Those suffering from Focal Segment Glomeruloscerosis have damaged kidneys. This means that waste products such as uric acid are not excreted properly from the body. When this happens, uric acid becomes trapped in the bloodstream. This leads to the accumulation of urate crystals in the joints, causing pain and inflammation.
Steps
Managing a Gout Attack in Your Ankle
-
1Elevate the painful joint. In doing so, gravity will help to reduce the inflammation of the ankle as the blood slowly drains from the inflamed area. The minimum elevation needed is 30 degrees over a period of one hour, so that all the blood will circulate back towards the heart.[1]
-
2Avoid putting pressure on the painful joint. The patient should try to keep their feet off the ground for as long as possible, until the pain and swelling subsides.Advertisement
-
3Take anti-inflammatory medication.[2] Gout causes inflammation and redness around the affected joint. Inflammation then leads to swelling which makes the pain worse.[3]
- Aspirin and Ibuprofen are highly recommended anti-inflammatories that can offer relief by reducing the inflammation and blocking the pain.
- 500 mg of ibuprofen or paracetamol can be taken 3 to 4 times a day, but only after checking with your physician for any possible adverse reactions to these reactions in FSGS patients.
-
4Keep your ankle stable. The aching joint should be immobilized for greater relief. A crepe bandage may be useful for this. It should be tied starting from the toes, then wrapped upwards gradually towards the ankle joint.
- This will give the joint support, reduce swelling and pain and keep it immobilized, allowing for faster recovery.
-
5Take medication to deal with your flare-up. In patients with FSGS, doctors suggest prednisone (steroid) to be given for a period of 6 months.[4] This will reduce the load of the kidneys as well as reduce the pain caused by gout. The exact dosage will be decided by the physician as steroids need to be monitored closely.[5]
- Colchicine (Colcrys) is suggested by many doctors in order to reduce the initial attack of gout. Colchicine causes inhibition of mitosis (inhibition of microtubule) and neutrophil activity leading to an anti-inflammatory effect.[6]
- This medication may be continued for life as it helps in controlling uric acid levels in the body.
Creating a Gout and FSGS-Friendly Diet
-
1Understand why a proper diet can help you deal with gout. The most important way to reduce the risk of gout in patients suffering from focal segment glomerulosclerosis is through a proper diet.[7]
- Remember that most of the purine in the body comes from the food we eat. Limiting purine consumption limits the uric acid in the body which decreases the risk of gout.[8]
- Another factor to consider is that due to FSGS the uric in the body is not excreted. Since purine it not excreted, limiting high purine food is necessary to prevent the accumulation of uric acid in the body.
-
2Lower your intake of animal-based proteins. Animal proteins are high in purine.[9] These foods include organ meat (liver, kidney, and brains), lamb, beef, pork, chicken, anchovies, sardines, mackerel and scallops.[10]
- Other seafood such as tuna, shrimp and lobsters also contain purines. Decreasing consumption of animal protein will help you prevent gout.
- Limit meat, poultry or fish to 113 to 170 grams per day.
-
3Avoid foods that are high in saturated fat. Saturated fat is also bad for those who are at high risks for gout. High saturated fat in the body may lead to obesity. Being overweight or obese increases the risk of having hyperuricemia.[11]
- Saturated fats also decrease the elimination of uric acid in the body. Food high in saturated fats include deep fried food, high fat cuts of meat, chicken with skin, butter, ice cream, lard, palm and coconut oil.
-
4Stick to foods that contain monosaturated fats. Opting for healthier alternatives that the foods listed above may help to decrease the saturated fat in your body. Instead of using oil that is high in saturated fat choose oil that contains monounsaturated fats.
- Olive oil, Canola oil, Sunflower oil, and peanut oil are examples of oil that are monounsaturated fats. Replace butter or margarine with healthier options such as peanut butter
- When preparing a meal with meat, remove the fat from the meat or the skin from the chicken. This will limit the saturated fat that gets into your body.
-
5Cut beer out of your diet. Studies have shown that beer is linked with gout. Beer interferes with the elimination of uric acid in the body.[12]
- A better option instead of beer is wine. Studies have shown that one to two five ounces of wine a day do not increase the risk of gout.
- When drinking wine, just remember that too much wine may still cause gout. Limiting your intake to 2 glasses is recommended.
-
6Stay away from foods that contain fructose. Fructose is also known to increase uric acid. This is because the metabolism of fructose in the liver drives increases the production of uric acid.[13]
- Foods that are high in fructose are table sugar, corn syrup, honey, molasses, maple syrup, fruits and fruit juices. You are advised against consuming more than 32 g (8 tsp.) of sugar based or fructose based foods daily in order to reduce the risk of gout.
- Instead of using the syrups and sugar stated above, use applesauce as a healthier alternative. Fruits such as watermelon, strawberry, avocado and kiwi have a low fructose content.
Making Lifestyle Changes
-
1Stay hydrated. Liquids, specifically water, play a major role in the body’s health. Water is needed by the body to help the kidneys get rid of waste in the body.[14]
- Drinking eight glasses of water every day makes the kidney more active in removing the excess uric acid produced in the body.
- It also lessens the formation of crystallized uric acid in the joints.
-
2Manage your weight if possible. Doctors usually advise FSGS patients suffering with gout to adopt any reduced-calorie diet containing low quantities of protein and low amounts of fat.[15]
- Obesity is closely associated with gout, although the exact link isn’t understood.
-
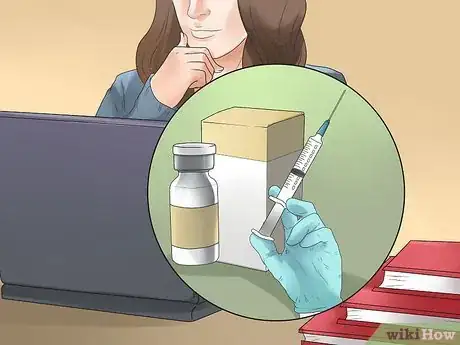
3Talk to your doctor about discontinuing certain medications. The traditional medications used for gout such as prednisone, allopurinol and colchicine are not usually used in kidney patients suffering from gout, as medications have negative side effects on the kidneys.
- These medications may worsen the disease and since the kidneys are the root cause of gout, the integrity of the kidneys must be maintained.
- Immunotherapy is the one of the best options for kidney patients suffering from gout.
Using Immunotherapy
-
1Understand the basics of immunotherapy. Immunotherapy is a treatment which stimulates the immune system to fight kidney disease. This type of therapy consists of six steps: exact diagnosis, blocking the immune reaction, immune tolerance, immune adjustment, immune clearance and immune protection.[16]
- In exact diagnosis, doctors run series of tests for autoimmune kidney damage. This test will confirm the type, amount and depositions of the antibodies the patient has.
- Blocking immune reaction is done to block the damages. Before progressing to the other steps of immunotherapy, it is important to block the autoimmune reaction of the body to the kidneys. This is because the body attacks the kidneys during the disease process. To stop that the immune system must blocked and reset. This is what immunotherapy does.
-
2Get your kidney biopsied. Before immunotherapy, a kidney biopsy must be done to determine the types of antibodies and immune complex that resulted in the kidney damage.[17]
- A biopsy is when a small section of the kidney is removed. With any kidney biopsy a patient must fast the day before, and then lie flat on a bed for 4 hours after the procedure.
- When the type of antibody and immune complex that attacks the kidneys is determined, immuno-suppresants are given to weaken these antibodies. This is when the blocking happens. The antibodies are weakened and this stops the damage to the kidneys.
-
3Protect yourself from infections when undergoing immunotherapy. Since antibodies are weakened during immunotherapy and since antibodies help our body fight infection, during this period of treatment the body may susceptible to diseases.
- Therefore, precautions must be taken to ensure that the patient will not contract any infection.
- Wearing a mask and avoiding contact with sick people are good precautionary measures.
References
- ↑ https://www.arthritis-health.com/blog/6-steps-gout-attack-relief
- ↑ Mohammad Dar, MD. Board Certified Internist & Health Policy Director. Expert Interview. Friday, September 3, 2021.
- ↑ https://www.hss.edu/conditions_gout-risk-factors-diagnosis-treatment.asp
- ↑ Mohammad Dar, MD. Board Certified Internist & Health Policy Director. Expert Interview. Friday, September 3, 2021.
- ↑ https://www.karger.com/Article/Pdf/454669
- ↑ Mohammad Dar, MD. Board Certified Internist & Health Policy Director. Expert Interview. Friday, September 3, 2021.
- ↑ https://nephcure.org/livingwithkidneydisease/diet-and-nutrition/
- ↑ Mohammad Dar, MD. Board Certified Internist & Health Policy Director. Expert Interview. Friday, September 3, 2021.
- ↑ Mohammad Dar, MD. Board Certified Internist & Health Policy Director. Expert Interview. Friday, September 3, 2021.
- ↑ https://familydoctor.org/low-purine-diet/
- ↑ https://www.health.harvard.edu/pain/lifestyle-changes-to-reduce-the-risk-of-gout-attacks
- ↑ https://familydoctor.org/low-purine-diet/
- ↑ http://blog.arthritis.org/gout/fructose-sugar-gout/
- ↑ https://www.mdedge.com/rheumatology/article/152779/gout/higher-water-intake-linked-less-hyperuricemia-gout
- ↑ https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/gout-diet/art-20048524
- ↑ https://www.mdanderson.org/content/dam/mdanderson/documents/for-physicians/algorithms/clinical-management/clin-management-nephritis-web-algorithm.pdf
- ↑ https://unckidneycenter.org/kidneyhealthlibrary/glomerular-disease/focal-segmental-glomerulosclerosis-fsgs/
- http://www.helpguide.org/life/healthy_diet_fats.htm



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...