This article was co-authored by George Sachs, PsyD. George Sachs is a Licensed Psychologist and the Owner of Sachs Center based in New York, New York. With over ten years of experience, Dr. Sachs specializes in treating ADD/ADHD and Autism Spectrum Disorders in children, teens, and adults. He holds a BS in Psychology from Emory University. Dr. Sachs earned his Doctorate of Psychology (PsyD) from the Illinois School of Professional Psychology, Chicago. He completed his clinical training in Chicago at Cook County Hospital, Mt. Sinai Hospital, and the Child Study Center. Dr. Sachs completed his internship and postdoctoral work at the Children’s Institute in Los Angeles, where he supervised and trained therapists in Trauma-Focused Cognitive Behavioral Therapy (TFCBT). He has been trained as a Gestalt Therapist and certified by the Gestalt Associates Training Program of Los Angeles. Dr. Sachs is the author of The Adult ADD Solution, Helping the Traumatized Child, and Helping Your Husband with Adult ADD. He has appeared on the Huffington Post, NBC Nightly News, CBS, and WPIX discussing his holistic approach to ADD/ADHD treatment.
There are 29 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 159,136 times.
Attention-Deficit/Hyperactivity Disorder (ADHD) is a brain-based disorder that impacts a person’s ability to concentrate and focus. In addition, the person may have trouble remaining still, fidgeting or talking excessively. While ADHD in children can be a difficult disorder to deal with, certain strategies will help manage symptoms while teaching children good habits. After your child has received a diagnosis, start establishing routines and consistent structure to provide a solid foundation for handling his or her ADHD.
Steps
Diagnosing ADHD in Kids
-
1Determine if your child has symptoms of inattentive ADHD presentation. There are three types of presentations of ADHD. In order to qualify for a diagnosis, children aged 16 and under must exhibit at least six symptoms in more than one setting, for at least six months. Symptoms must be inappropriate for the person’s developmental level and be seen as interrupting normal functioning in social or school settings. Symptoms for ADHD (inattentive presentation) include: [1]
- Makes careless mistakes, is inattentive to detail
- Has trouble paying attention (tasks, playing)
- Doesn’t seem to be paying attention when someone is talking to her or him
- Doesn’t follow through (homework, chores, jobs); easily sidetracked
- Is organizationally challenged
- Avoids tasks requiring sustained focus (like schoolwork)
- Can’t keep track of or often loses keys, glasses, papers, tools, etc.
- Is easily distracted
- Is forgetful
-
2Determine if your child has symptoms of hyperactive-impulsive ADHD presentation. Some symptoms must be at the level of “disruptive” for them to count in a diagnosis. Track if your child has at least six symptoms in more than one setting, for at least six months: [2]
- Fidgety, squirmy; taps hands or feet
- Feels restless, running or climbing inappropriately
- Struggles to play quietly/do quiet activities
- “On the go” as if “driven by a motor”
- Excessive talking
- Blurts out even before questions are asked
- Struggles to wait for their turn
- Interrupts others, inserts self into others’ discussions/games
Advertisement -
3Determine if your child has combination presentation ADHD. The third presentation of ADHD is when the subject meets criteria to qualify for both inattentive and hyperactive-impulsive criteria of ADHD. If your child has six symptoms from either category, he or she may have a combined presentation of ADHD. [3]
- If you are unsure of your child's behavior, ask other adults and friends of your child. For example, your child's friends, friends' parents, teacher, or sports coach. Educators and childcare professionals might have more context for your child's behavior because they have worked with so many children.
-
4Get a diagnosis from a mental health professional. As you determine your child’s level of ADHD, seek the guidance of a mental health professional to make an official diagnosis. This person will also be able to determine whether your child’s symptoms can be better explained by or attributable to another psychiatric disorder.
-
5Ask your child’s mental health professional about other disorders. Talk with your doctor or mental health professional about other disorders or conditions that might have symptoms that are similar to ADHD. As if having an ADHD diagnosis isn’t challenging enough, one out of every five with ADHD is diagnosed with another serious disorder (depression and bipolar disorder are common partners).
Establishing Organization and Structure at Home
-
1Make structure and routine your default. The key to success lies in establishing consistent schedules and routines combined with organization and structure. Not only will this alleviate the stress on the child with ADHD, it should decrease misbehaviors that are spurred on by that stress. The less stress, the more success; the more success—and resultant praise [6] —the better the self-esteem, which sets a child up for additional success in the future. [7]
- Have a whiteboard with the schedule for the day written down. Display it in the kitchen, living room, or somewhere else obvious.
- Displaying schedules and responsibilities in the house remind your kids what they have to do, and decrease their ability to say “I forgot.”
-
2
-
3Maintain structure during school breaks. Winter, spring, and summer breaks can be difficult times for parents of children with ADHD: the structure and schedule of the past school year suddenly ends. With less structure, children with ADHD can experience higher levels of stress and exhibit more symptoms. Keep to schedules and routines as much as possible to lower everyone’s stress.
- Try imagine walking a high wire without a net for nine months and then all of a sudden, the wire snaps and you are plummeting toward the ground. That’s summer break for a child with ADHD: falling without a net in place. Try to remember where your child is coming from to empathize with their experience.
- You can try to grandfather in changes in the schedule. For example, if your child woke up at 7am during the school year, the first week of summer break wake up at 7:30am; the second week, 8am. The long-term scheduled change can ease your child into different schedules.
-
4Help your child learn time management. A child with ADHD doesn’t have a great concept of time.[10] People with ADHD struggle with clock issues, both with gauging the amount of time it will take to accomplish a task and estimating how much time has passed. Give your child ways to report back to you or complete a task in the right amount of time. For example:
- Buy a kitchen timer to take outside when you want him or her to come in after 15 minutes—or play a CD and tell her she needs to complete her chores by the time it ends.
- You can teach a child to brush teeth the right length of time by humming the ABCs or the Happy Birthday song.
- Play beat the clock by trying to finish a chore before a particular song ends.
- Sweep the floor to the rhythm of a song.[11]
-
5Establish storage bin systems. Children with ADHD are constantly trying to make sense of their environment. Parents can help by organizing the home, especially the child’s bedroom and play area. Establish a storage system that separates items into categories and reduces the crowding that leads to overload.
- Consider color-coded storage cubes and wall hooks as well as open shelves.
- Use picture or word labels to remind them what goes where.[12] [13]
- Label storage tubs with corresponding pictures. Have separate storage tubs for different toys (dolls in the yellow bucket with a picture of Barbie taped on it, My Little Pony toys in the green bucket with the horse picture attached, etc.). Separate clothing so that socks have their own drawer and there’s a picture of a sock on it, and so on. [14] [15]
- Keep a box or a storage bin in a central location of the home where you can pile your child’s toys, gloves, papers, Legos, and other miscellany that tend to spread all over the place. It will be easier for the child with ADHD to empty that bucket than to be told to pick up all her things from the living room. [16]
- You also might establish a rule that the third time you find Darth Vader in the living room unattended, he gets confiscated for a week—or that if the bucket gets full, a lid will be put on it and it’ll vanish for a while with all those special treasures inside.
Helping Your Child Succeed in School
-
1Coordinate with your child’s teachers. Meet with your child’s teacher to discuss a variety of topics with the teacher. These include effective rewards and consequences, effective homework routines, how you and the teacher will communicate on a regular basis about problems and successes, how you can mirror what the teacher is doing in the classroom for greater consistency, and so on.[17]
- For some students, success will be obtained relatively easily by establishing consistent schedules, routines, and homework communication methods as well as utilizing effective organizational tools such as planners, color-coded binders, and checklists.
- Being on the same page with your teacher can remove the "teacher said differently" excuse.
-
2Use a daily planner for your child. Organization and consistent routines will save the day when it comes to homework, and it’s a good idea to coordinate with teachers whenever possible. Does the teacher provide a daily homework list or does the school promote the use of planners? If not, buy a planner that has plenty of space to write daily notes and show your child how to use it.
- If the teacher(s) can’t or won’t commit to initialing the planner every day, ask the teacher to help find a responsible student—a homework buddy [18] —to check the planner before dismissal each afternoon.
- If your child is struggling to remember assignments, check your child’s homework box in the planner every day as the first thing when you get home. If your kid remembered to write down the homework assignment, give your kid praise.
-
3Reward your child with praise. Praise is the best and easiest way to encourage learning and good behavior from your child. Giving your child positive feedback about something they did that makes you proud can also benefit your long term personal relationship.[19]
- Every day the planner comes home, make sure to give your child praise. Then make sure the planner back into the backpack every morning before school. Arrange for the homework buddy to give morning reminders to turn in the homework, too.
- Reward your child for trying and struggling to do the right thing, even when he or she fails. This teaches your child that work ethic, despite failing, is a good skill to have.
-
4Establish a consistent homework routine. Homework should be completed at the same time and same place every day. Have plenty of supplies on hand, organized in bins if you have the space.[20]
- Be sure homework doesn’t start the second your child walks in the door. Let him or her get rid of excess energy riding a bike or climbing trees for 20 minutes, or let her/him chatter and get that excess talking out of his system before telling him/her to do seatwork.
- Try to avoid allowing your kid to stall or put off work. Some kids use diversion techniques like asking for snacks, going to the bathroom, or complaining of tiredness and needing a nap. While these are all completely valid and normal things for a kid to ask for, try to notice when your kid is really trying to avoid work.
-
5Review homework assignments together. Show how you would organize the work and recommend ways to prioritize the assignments. Chunk big projects and set deadlines for individual stages to be completed.[21] [22]
- Provide a brain-food snack such as peanuts as you review the assignments.
- It is particularly important that you communicate with the teacher about what a good homework assignment looks like, and what doing the homework well looks like. You don't want to teach your child something that contradicts the teacher's methods or rules, even if just for consistency and structure.
-
6Help your child keep track of school belongings. Many children with ADHD have trouble keeping track of their belongings and struggle deciding or remembering which books to bring home each night—let alone remembering to take them back to school the next day.
- Some teachers will allow students to have a “home set” of textbooks. [23] This might be a recommendation for inclusion on an IEP as well.
- Consider having a list of items your child should leave home with near the door. Check this list every day before your child leaves for school.
- It is tempting for you to control and remember everything, even if your child is supposed to be responsible for it. However, your child not only needs his or her textbooks to do homework, but also needs to remember his or her textbooks to learn responsibility and how to follow a schedule.
- If applicable, try using online books or sources and post the passwords somewhere in the house. Some find using the computer for homework and reading more comfortable.
-
7Encourage peer interactions for your child. One of the big challenges people with ADHD face as adults is that they didn’t learn to socialize appropriately as a child.[24] Pick an activity your child likes and that can fit into your routine.
- Encourage your child to participate in peer interactions like scouting activities, sports teams, and dance.
- Find an organization which will allow you and your child to volunteer together, such as a local food pantry.
- Host parties and encourage attendance at parties that will help your child to live as normal a life as possible. If your child is invited to a birthday party, have a frank discussion with the hosting parents and explain that you need to attend to act as an anchor—and disciplinarian, as necessary. They will appreciate your candor and your child will benefit from the experience.
-
8Role play to prepare your child for unfamiliar events. You might be able to decrease your child's potential for anxiety by role playing out the anxiety-producing situation. In addition to providing familiarity and a comfort level for the upcoming event, role playing allows you to see how your child might react then guide him or her in appropriate responses. [25] This is especially helpful in preparing to meet new people, work out conflicts with friends, or going to a new school.
- If your child does not want to role play with you, ask a therapist or other trusted adult.
- When role-playing, explicitly identify skills and techniques for navigating the situation. Write them down and discuss why they are useful.
-
9Look into your school’s special services. In the United States, children qualify for free special education services based on one of two basic reasons: they have a qualifying disability or they have fallen far behind their peers academically. Once parents become aware that their child is not succeeding in school and they feel additional help is required (an opinion usually made in conjunction with the classroom teacher), parents may request a special education evaluation. If you live outside the United States, contact your local school board to ask about special services.[26]
- This request should be made in writing. [27]
- Assistance can take various forms from minor accommodations (such as extra time for taking tests) to self-contained classrooms with teachers and aides who are specially trained to deal with children who exhibit behavioral disruptions. [28]
- Once qualified, a child with ADHD may have access to other school-based services, as well, such as riding home in a smaller bus with extra staff who supervise students more closely than a lone driver is able to do.
- Beware the school that tells you ADHD is not a qualifying disability! It is true that ADHD is not listed as one of the 13 disability categories in the language of the Individuals with Disabilities Education Act (IDEA), but category 9 is “other health impairment,” which is later defined as “… chronic or acute health problems such as asthma, attention deficit disorder or attention deficit hyperactivity disorder… which adversely affect a child’s educational performance.”
-
10Get an individualized education plan (IEP) for your child. An IEP is a formalized document created by school staff and parents that spells out the academic, behavioral, and social goals of special-ed students. It includes how results will be determined, as well as specific interventions that will be used to achieve the goals. The IEP lists decisions made concerning self-contained classrooms, percentage of time in mainstream classrooms, accommodations, discipline, testing, and more.[29]
- In the United States, you must provide documentation of your child’s ADHD diagnosis in order to get an IEP. Complete a special education evaluation that shows the child’s disability is interfering with his or her education. Then, the school will ask you to participate in an IEP conference. If you live outside the United States, contact your local school board to ask about special services. The school is required to invite parents to regular IEP conferences to evaluate the progress of the child and the effectiveness of the plan. Then adjustments can be made as needed. The school is legally bound to follow the guidelines laid down in the IEP. Teachers who fail to follow the IEP can be held liable.
- Be sure that the IEP is specific to your child and that your input is included in the form. Do not sign a completed IEP until you have reviewed it and added your input. [30]
- Once a child has an initial IEP, it becomes easier to establish special education services when changing schools or transferring to a new school district.
-
11Consider a 504 plan. Many children who do not qualify for an IEP qualify for a 504 plan, a plan that makes milder accommodations for students with a disability that impacts a ‘major life function’.
- A 504 plan will usually be one or two pages that list your child’s learning differences and the services provided to assist them. Unlike an IEP, goals and adjustments for after high school will not be included.
-
12Act in your child’s best interests. Unfortunately, even with outstanding cooperation and effort by the adults, many children still will not succeed. They may require more intensive services available through the school or district special education department. In some cases, rigid teaching methods by inflexible teachers are the issue [31] and parents must seek administrative support or look into changing teachers, changing schools, or exploring special education options. Choose the best paths for your circumstance to ensure maximum success for your child.
Making Chores Successful
-
1Avoid chore wars with routines and consistency. Decrease the arguments and petulance of assigning chores by setting and enforcing a consistent time they occur. Tie them to a regular reward whenever possible. For example:
- Instead of serving dessert at the end of dinner, serve it after the table is cleared and dishwasher loaded.
- Afternoon snacks will hit the table after the trash is taken out.
- Beds must be made before going outside to play.
- The family pet must be fed before humans have breakfast.
-
2Give instructions one step at a time. Establish routines around chores that reflect consistent instructions that are given one step at a time. Then have your child repeat the instruction then getting praise at each step.[32] For example:
- Loading the dishwasher: First load all the plates on the bottom. (“Great job!”). Now load all glasses on the top. (“Excellent!”). Next is silverware …
- Laundry: First find all the pants and put them into a stack here. (“Awesome!”) Now put shirts in a stack there. (“Super-duper!”). Socks … then have the child fold each stack, then put the stacks in his or her room, one stack at a time.
-
3Post visual cues as reminders. Use calendars, written schedules and chore boards to remind your child of chores that need to be done. These tools remove the “I forgot” excuse.[33]
-
4Make chores more fun for your child. Whenever possible, find ways to make chores more fun and help remove the stress of the task. You need to teach your child compliance, teamwork, and the need to pull his weight—but there’s no reason it can’t be fun at the same time.[34]
- Belt out instructions in a variety of silly voices or have puppets give orders.
- Walk backward when checking progress and make back-up “beeps.”
- Have your child dress like Cinderella on a chore morning and play music from the movie that she can sing to as she works.[35]
- Keep an eye on your child’s attitude. If you sense he or she is getting frazzled, make the next chore super silly or assign movement to it. Say to your child, “Pretend you are a shark as you put this book on my desk.” Or, simply call for a cookie break. [36]
Disciplining Your Child
-
1Be consistent with discipline. All children need discipline and to learn that bad behavior comes with consequences. [37] [38] For discipline to be effective at changing behavior, it must be consistent. A lack of consistency can lead to a child developing confusion or willfulness.
- Your child should know the rules and the consequences for breaking the rules.
- The consequence should happen the same every time the rule is broken.
- In addition, the consequence should apply whether the misbehavior happens at home or in public.
- It’s crucial that all caretakers are on board, disciplining the same way. [39] When one person is a weak link amongst the adults in the child’s sphere, that weakness will be exploited every time. He or she will “shop for a better answer” or play the “divide and conquer” game. Be sure that the babysitter, daycare or after-school provider, grandparents, and other adults who have charge of your child are on board with your desire for consequences that are consistent, immediate, and powerful.
-
2Enforce the discipline immediately. The consequence for a problem behavior has an immediate impact. It is not delayed. Persons with ADHD often struggle with time concepts,[40] so postponing a consequence has no meaning. It invites an explosion if the child gets a forgotten consequence for a previous infraction that might as well have happened a year ago.[41] [42]
-
3Ensure your consequence is powerful. If the consequence for speeding was paying a fine of a buck for every mile per hour over the speed limit, we’d all speed constantly. This is not a powerful enough consequence to change our behavior.
- We tend to monitor our speed to avoid a $200 ticket plus higher insurance premiums. The same applies to children with ADHD. The consequence needs to be powerful enough to act as a deterrent.[43] [44]
- Be powerful, but fair. Sometimes, you can ask your child what he or she thinks is fair to get a gauge on what a powerful consequence might be.
-
4Control your own emotions. Much easier to say than do, you must not respond to misbehavior emotionally. Your anger or raised voice may cause anxiety or send a message that your child can control you by getting you angry. Remaining calm and loving will convey the message you want. Before taking action, do a self-check to make sure you are responding in the way you want to respond.[45]
- If you need time to calm down but also need an immediate consequence, you can tell your child, “I am so upset with you, that I cannot talk about the consequence of your action right now. We will discuss it tomorrow, but believe that you are in trouble as of now.” Say this in a calm and factual tone, not a threatening tone.
- Recognize the importance of emotions, while not being emotional. There is a fine line between acknowledging the influence of emotions and feelings on our love for our children, and letting those emotions control the important decisions we make to care for our children.
- Create mechanisms for yourself to calm down and handle your own emotions before responding to the situation emotionally.
-
5Be firm and stick to your rules. Your child may persistently ask you ten times to have a special privilege and you say no nine times. But if you finally cave in at the end, the message sent and received is that being a pest will pay off. [46]
- If your child is persistent in the moment, you can respond with, "If you care enough about it, we can have a discussion about changing the rules later this weekend. But right now, we're going to follow the rules that we decided on earlier."
-
6Avoid rewarding bad behavior with attention. Some kids crave attention badly enough to behave badly so they’ll get it. Instead, reward good behavior with an abundance of attention but consequence bad behavior with limited focus lest your attention be interpreted as a reward! [47]
-
7Refuse to argue or vacillate. Once you give a specific instruction, it is to be followed without exception, because you are the adult in charge. If you allow your child to argue, he or she sees that as an opportunity to win. Many children are willing to argue until the other party exhausts and caves in. Avoid giving your child that opportunity by setting rules you can call on as objective precedents. [48] [49]
- If your child is not acknowledging the authority of your rules, maybe change your rules up. In a calmer, different setting, ask your child what he or she thinks would be fair rules. See if you can negotiate any compromises so that your child follows the rules more, and you are both happier with the outcome.
-
8Follow through with consequences. If you threaten a dire consequence, and the bad behavior occurs, follow through on the promised punishment. If you don’t follow through, your child won’t listen the next time you try to coerce good behavior or prevent bad behavior. This is because you’ll already have a track record in his or her eyes.[50]
-
9Speak only when your child's attention is on you. Make sure your child is making eye contact with you. If you assign a task, make the instructions brief and have him/her repeat it back to you. Wait for the job to be completed before distracting her/him with anything else.[51]
-
10Remember your child is unique. Even if your child has other siblings, avoid comparisons with other kids, especially siblings. Children with ADHD have brain-based differences that often require accommodations.[52] Generally, you’ll find that you’ll have to give a child with ADHD multiple reminders, make the task shorter, require a different standard of completion, and more. Even then, kids with ADHD present symptoms and live very differently from one another. Your child is different and will act differently.
-
11Use timeouts effectively. Instead of a timeout being a prison sentence, use this time [53] as an opportunity for the child to self-calm and contemplate the situation. Then, he or she will discuss with you how this situation came about, how to resolve it and how to prevent it from happening again in the future. You’ll also talk about consequences if it should reoccur.
- Choose a designated spot in your house where your child will stand or sit quietly. This should be a place where he or she cannot see the television or otherwise be distracted.
- Designate an amount of time to remain quietly in place, self-calming (usually not more than one minute per age of the child). As the system becomes more comfortable, the child might remain in place simply until he or she has achieved a calm state.
- Then ask permission to come talk it over. The key is to allow the child time and quiet; give praise for a job well-done. Don’t think of timeout as a punishment; consider it a reboot.
-
12Anticipate problems. You need to become as adept at foreseeing the future when you have a child with ADHD. Anticipate what problems you might encounter and plan interventions to prevent them.[54]
- Help your child develop cause-and-effect and problem-solving skills by troubleshooting possible problems together. [55] Make it a habit to think about and discuss possible pitfalls with your child before going to dinner, the grocery, a movie, church, or other public places. [56]
- Before leaving, have your child repeat aloud what was decided regarding rewards for behaving and the consequence for misbehaving.[57] Then if you see your child struggling with behavior at that venue, you can ask him or her to repeat the agreed upon reward to be earned or consequence to be administered; it might be just enough to get you through!
Using Positive Reinforcement
-
1Use positive input. You can get someone to cooperate better by asking nicely than by demanding or threatening. Those with ADHD are even more sensitive to the threats or demands, as they tend to feel that they’re “always” messing up or in trouble. Regardless of your parenting style or personality, it’s extremely important that you keep the input ratio weighted to the positive side: A child with ADHD needs to feel that he or she is being praised more often than criticized. The positive input must significantly outweigh the negative input to counterbalance all the feelings of failure that is encountered in a typical day.[58]
- Praise your child for struggling and trying to do something good, rather than for success at anything.
-
2Write house rules as positive statements. Whenever possible, invert house rules so they read as positives.[59]
- For instance, instead of admonishing, “Don’t interrupt!” the rule can be reminded as “Wait your turn,” or “Allow your sister to finish what she was saying.”
- It might take practice to flip those negatives from “Don’t talk with your mouth full!” to “Finish what’s in your mouth before sharing.” But work to make it a habit.
-
3Use incentives. With young kids, use tangible rewards to motivate kids to follow routines and directions. As children get older, you can move on to more abstract rewards. Below is this idea outlined with examples and a metaphor.
- There’s an adage about a donkey moving faster for a carrot (reward) than a stick (punishment). Are you having trouble getting your child to bed on time? You can offer a stick (“Be ready for bed by 8 p.m. or else ….”) or you can find a carrot: “If you are ready for bed by 7:45 p.m., you can have 15 minutes to …”
- Buy a little bucket and stock it with “carrots.” These can be little rewards you can dole out when your child complies with a directive or behaves appropriately. Get a roll of stickers, a bag of 20 plastic army guys at a dollar store or a sack of 12 sparkly rings from the birthday party aisle.
- Get creative and add homemade coupons good for a popsicle, 10 minutes on the computer, playing a game on Mom’s phone, getting to stay up 15 minutes later, getting a bubble bath instead of taking a shower, etc.
- In time you can cut back to intermittent tangible rewards.[60] Instead, use verbal praise, hugs, and high-fives that allow you to continue a high degree of positive input[61] that will motivate your child to behave while building his or her self-esteem.
-
4Transition to a points system for rewarding good behavior. Once you’ve experienced success with the carrot bucket, wean your child from concrete rewards (toys, stickers) to praise (“Way to go!” and high-fives). Then you might consider designing a point system for positive behavior. This system acts as a bank where your child can earn points to buy privileges.[62]
- Compliance earns points and non-compliance loses points. Record these points on a sheet or poster that is accessible to the child.
- Design your schedule considering the unique aspects of the ADHD brain. Making a more successful schedule increases your child’s opportunity for praise and self-esteem. Make a checklist[63] built around the child’s schedule,[64] showing the deadlines for completing tasks. [65]
- Choose possible rewards that will motivate your child. This system also serves to externalize those motivations. [66]
Managing ADHD with Nutrition
-
1Talk to your child’s pediatrician about dietary changes. Be certain to run any major changes in diet by your child’s pediatrician. This includes changes related to vitamins and supplements.
- Ask your doctor about any conflicts that could negatively impact your ADHD medication.
- The pediatrician can also suggest recommended dosages of various supplements and warn of possible side effects. For instance, melatonin may improve sleep in persons with ADHD, but it might also induce vivid dreaming which may be unpleasant.
-
2Serve complex carbohydrates to boost serotonin levels. People with ADHD tend to have lower serotonin and dopamine levels. You can experiment with changes to your child’s diet in order to counter-effect these deficiencies to some extent.
- Experts recommend a complex-carb diet to boost serotonin for improved mood, sleep, and appetite. [67]
- Skip simple carbs (anything with added sugar, fruit juice, honey, jelly, candy, soda) [68] that cause a temporary serotonin spike. [69]
- Instead, choose complex carbohydrates such as whole grains, green vegetables, starchy vegetables, and beans. [70] These all are digested more slowly, and sugars are “time-released” into your child's bloodstream. [71]
-
3Serve protein to boost your child's focus. Serve a protein-rich diet that includes several proteins over the course of the day to keep dopamine levels high. [72] This will help your kid improve his focus.
- Proteins include meat, fish, and nuts, as well as several foods that double as complex carbs: legumes and beans. [73]
- Chicken, canned tuna, eggs, and beans are all great examples of protein sources that are usually cheap and affordable in the United States.
-
4Choose omega-3 fats. ADHD experts recommend improving the brain by avoiding “bad fats” such as those found in trans-fats and fried foods, burgers and pizzas. Instead, choose omega-3 fats from salmon, walnuts, and avocados. [74] These foods may help lower hyperactivity while improving organizational skills.
-
5Increase your child’s intake of zinc. Seafoods, poultry, fortified cereals and other foods with a high zinc content or taking zinc supplements are linked to lower levels of hyperactivity and impulsivity in some studies; however, there is limited research on this and you should speak with your child’s physician about potential benefits, if any.[75]
-
6Add spices to your child’s food. Don’t forget that some spices do more than add flavor. For example, saffron counters depression, while cinnamon helps with attention. [76]
-
7Experiment with eliminating certain foods. Some studies show that eliminating wheat and dairy, as well as processed foods, sugars, additives and dyes (especially red food coloring), can have a positive impact on behavior in children with ADHD. [77] While not everyone will be willing or able to go to that length, some experimentation may produce improvements that make a difference. [78]
Trying Medication
-
1Ask your child’s doctor mental health professional about medications. There are two basic categories of ADHD medication: stimulants (such as methylphenidate and amphetamine) and non-stimulants (such as guanfacine and atomoxetine). [79]
- Hyperactivity is treated successfully with stimulant medication because the brain circuitry being stimulated is responsible for controlling impulsivity and improving focus.[80] Stimulants (Ritalin, Concerta, and Adderall) help regulate neurotransmitters (norepinephrine and dopamine). [81] These medications can be short-acting or longer-acting. This means that the effects of the medication can last a short period of time, which can be useful for individuals who can manage their ADHD most of the time, or some medications can last throughout the day.[82]
- Non-stimulants boost norepinephrine, a chemical in the brain that seems to help with attention span.[83] These types of medications are longer-lasting as well.
-
2Monitor side effects from stimulants. Stimulants have fairly common side effects of decreased appetites and trouble sleeping. Sleep issues often can be resolved by lowering the dosage.
- Your child’s psychiatrist or pediatrician may also add a prescription to improve sleeping such as clonidine[84] or melatonin.
- For children ages 4-5, the primary treatment approach recommended is behavioral modification and parent training, with the option to use methylphenidate if behavioral techniques do not fully manage symptoms.[85]
- Combination of behavioral therapy is recommended along with medication for all age groups[86]
-
3Ask about non-stimulant medication. Non-stimulant medications may work better for some persons with ADHD. Non-stimulant anti-depression medications are often used to treat ADHD. These help regulate neurotransmitters (norepinephrine and dopamine).
-
4Find the right medication. Deciding on the right form, dosage, and specific prescription of medication is tricky because people respond uniquely to different medications. Work with your child's doctor and the most recent research to find the right form and dosage for your child.
- For example, many medications can be taken in an extended-release format, which eliminates the need to deal with dosing at school. [89]
- Some individuals decline regular usage of medication, taking it only in situations when they need the medication. In these cases, individuals want a fast-acting version.
- For older children who learn to compensate for their ADHD challenges, medication may become unnecessary or be reserved for using during special occasions, such as when taking college entrance exams or finals.
-
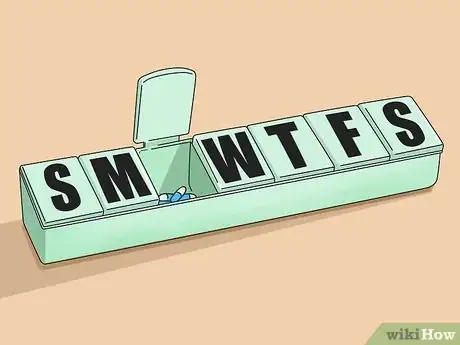
5Use a pill container. Children will probably need extra reminders and assistance in order to take their medication regularly. A weekly pill container can help parents keep track of medications.[90] If you child is taking stimulant medication, it is highly recommended that parents control medication storage and monitor its use because the DEA classifies stimulants as having a high abuse potential.
-
6Check in with your child’s pediatrician periodically to assess the prescription. The medication’s effectiveness may change depending on certain factors. The effectiveness may change depending on growth spurts, hormonal fluctuations, diet and weight changes, and how fast your child's resistance to the drug builds up. [91]
Expert Q&A
-
QuestionIs medication the only way to help kids with ADHD?
 George Sachs, PsyDGeorge Sachs is a Licensed Psychologist and the Owner of Sachs Center based in New York, New York. With over ten years of experience, Dr. Sachs specializes in treating ADD/ADHD and Autism Spectrum Disorders in children, teens, and adults. He holds a BS in Psychology from Emory University. Dr. Sachs earned his Doctorate of Psychology (PsyD) from the Illinois School of Professional Psychology, Chicago. He completed his clinical training in Chicago at Cook County Hospital, Mt. Sinai Hospital, and the Child Study Center. Dr. Sachs completed his internship and postdoctoral work at the Children’s Institute in Los Angeles, where he supervised and trained therapists in Trauma-Focused Cognitive Behavioral Therapy (TFCBT). He has been trained as a Gestalt Therapist and certified by the Gestalt Associates Training Program of Los Angeles. Dr. Sachs is the author of The Adult ADD Solution, Helping the Traumatized Child, and Helping Your Husband with Adult ADD. He has appeared on the Huffington Post, NBC Nightly News, CBS, and WPIX discussing his holistic approach to ADD/ADHD treatment.
George Sachs, PsyDGeorge Sachs is a Licensed Psychologist and the Owner of Sachs Center based in New York, New York. With over ten years of experience, Dr. Sachs specializes in treating ADD/ADHD and Autism Spectrum Disorders in children, teens, and adults. He holds a BS in Psychology from Emory University. Dr. Sachs earned his Doctorate of Psychology (PsyD) from the Illinois School of Professional Psychology, Chicago. He completed his clinical training in Chicago at Cook County Hospital, Mt. Sinai Hospital, and the Child Study Center. Dr. Sachs completed his internship and postdoctoral work at the Children’s Institute in Los Angeles, where he supervised and trained therapists in Trauma-Focused Cognitive Behavioral Therapy (TFCBT). He has been trained as a Gestalt Therapist and certified by the Gestalt Associates Training Program of Los Angeles. Dr. Sachs is the author of The Adult ADD Solution, Helping the Traumatized Child, and Helping Your Husband with Adult ADD. He has appeared on the Huffington Post, NBC Nightly News, CBS, and WPIX discussing his holistic approach to ADD/ADHD treatment.
Licensed Psychologist No, it's not the only way, although it is a fairly effective option in many cases. Coaching and therapy can also help children with ADHD when it comes to executive function issues like organizational planning and decision making.
No, it's not the only way, although it is a fairly effective option in many cases. Coaching and therapy can also help children with ADHD when it comes to executive function issues like organizational planning and decision making. -
QuestionHow do I stop yelling at my ADHD child?
 George Sachs, PsyDGeorge Sachs is a Licensed Psychologist and the Owner of Sachs Center based in New York, New York. With over ten years of experience, Dr. Sachs specializes in treating ADD/ADHD and Autism Spectrum Disorders in children, teens, and adults. He holds a BS in Psychology from Emory University. Dr. Sachs earned his Doctorate of Psychology (PsyD) from the Illinois School of Professional Psychology, Chicago. He completed his clinical training in Chicago at Cook County Hospital, Mt. Sinai Hospital, and the Child Study Center. Dr. Sachs completed his internship and postdoctoral work at the Children’s Institute in Los Angeles, where he supervised and trained therapists in Trauma-Focused Cognitive Behavioral Therapy (TFCBT). He has been trained as a Gestalt Therapist and certified by the Gestalt Associates Training Program of Los Angeles. Dr. Sachs is the author of The Adult ADD Solution, Helping the Traumatized Child, and Helping Your Husband with Adult ADD. He has appeared on the Huffington Post, NBC Nightly News, CBS, and WPIX discussing his holistic approach to ADD/ADHD treatment.
George Sachs, PsyDGeorge Sachs is a Licensed Psychologist and the Owner of Sachs Center based in New York, New York. With over ten years of experience, Dr. Sachs specializes in treating ADD/ADHD and Autism Spectrum Disorders in children, teens, and adults. He holds a BS in Psychology from Emory University. Dr. Sachs earned his Doctorate of Psychology (PsyD) from the Illinois School of Professional Psychology, Chicago. He completed his clinical training in Chicago at Cook County Hospital, Mt. Sinai Hospital, and the Child Study Center. Dr. Sachs completed his internship and postdoctoral work at the Children’s Institute in Los Angeles, where he supervised and trained therapists in Trauma-Focused Cognitive Behavioral Therapy (TFCBT). He has been trained as a Gestalt Therapist and certified by the Gestalt Associates Training Program of Los Angeles. Dr. Sachs is the author of The Adult ADD Solution, Helping the Traumatized Child, and Helping Your Husband with Adult ADD. He has appeared on the Huffington Post, NBC Nightly News, CBS, and WPIX discussing his holistic approach to ADD/ADHD treatment.
Licensed Psychologist It's important to understand the limitations of ADHD, and set realistic expectations for not only your child, but yourself. If you can pause and take a step back in the heat of the moment, you're going to have a much easier time regulating your feelings. Setting clear and consistent boundaries is also a big part of this, since your child is going to be more likely to cross the line if they don't even know where the line is. But really, when it comes to yelling it's on you to understand, be empathetic, and acknowledge the reality of living with ADHD.
It's important to understand the limitations of ADHD, and set realistic expectations for not only your child, but yourself. If you can pause and take a step back in the heat of the moment, you're going to have a much easier time regulating your feelings. Setting clear and consistent boundaries is also a big part of this, since your child is going to be more likely to cross the line if they don't even know where the line is. But really, when it comes to yelling it's on you to understand, be empathetic, and acknowledge the reality of living with ADHD. -
QuestionHow can I communicate more effectively with my child who has ADHD?
 Laura Reber, SSPLaura Reber is a school psychologist and founder of Progress Parade, an organization that provides 1:1 online tutoring with hand-picked specialists to students with academic needs, ADHD, learning disabilities, autism, and social-emotional challenges. Laura works with a team of school psychologists and specialized teachers to create personalized approaches for homework support, academic intervention, homeschooling, unschooling, and more. Laura holds a BS in Psychology from Truman State University and a Specialist in School Psychology degree (SSP) from Illinois State University.
Laura Reber, SSPLaura Reber is a school psychologist and founder of Progress Parade, an organization that provides 1:1 online tutoring with hand-picked specialists to students with academic needs, ADHD, learning disabilities, autism, and social-emotional challenges. Laura works with a team of school psychologists and specialized teachers to create personalized approaches for homework support, academic intervention, homeschooling, unschooling, and more. Laura holds a BS in Psychology from Truman State University and a Specialist in School Psychology degree (SSP) from Illinois State University.
School Psychologist Keep your message as short and specific as possible. That way, your child will be more likely to stay focused on what you're saying.
Keep your message as short and specific as possible. That way, your child will be more likely to stay focused on what you're saying.
Warnings
- Always consult a doctor before taking or being prescribed medication.⧼thumbs_response⧽
- Not every child with ADHD learns/acts the same.⧼thumbs_response⧽
- Fighting with and yelling at the child with ADHD only will lead to possible fear and sadness.⧼thumbs_response⧽
References
- ↑ Attention-Deficit / Hyperactivity Disorder (ADHD): Symptoms and Diagnosis found at http://www.cdc.gov/ncbddd/adhd/diagnosis.html
- ↑ Attention-Deficit / Hyperactivity Disorder (ADHD): Symptoms and Diagnosis found at http://www.cdc.gov/ncbddd/adhd/diagnosis.html
- ↑ Attention-Deficit / Hyperactivity Disorder (ADHD): Symptoms and Diagnosis found at http://www.cdc.gov/ncbddd/adhd/diagnosis.html
- ↑ Why Is My Child’s ADHD Not Better Yet? Recognizing The Undiagnosed Secondary Conditions That May Be Affecting Your Child’s Treatment by David Gottlieb, Thomas Shoaf, and Risa Graff (2006).
- ↑ The ADHD Update: Understanding Attention-Deficit/Hyperactivity Disorder by Alvin and Virginia Silverstein and Laura Silverstein Nunn (2008).
- ↑ ADHD and the Nature of Self-Control by Russell A. Barkley (1997).
- ↑ Organize Your ADD/ADHD Child: A Practical Guide For Parents by Cheryl R. Carter (2011).
- ↑ Putting On The Brakes: Young People’s Guide to Understanding Attention Deficit Hyperactivity Disorder (ADHD) by Patricia O. Quinn & Judith M. Stern (1991).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ ADHD and the Nature of Self-Control by Russell A. Barkley (1997).
- ↑ Organize Your ADD/ADHD Child: A Practical Guide For Parents by Cheryl R. Carter (2011).
- ↑ Putting On The Brakes: Young People’s Guide to Understanding Attention Deficit Hyperactivity Disorder (ADHD) by Patricia O. Quinn & Judith M. Stern (1991).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Putting On The Brakes: Young People’s Guide to Understanding Attention Deficit Hyperactivity Disorder (ADHD) by Patricia O. Quinn & Judith M. Stern (1991).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Putting On The Brakes: Young People’s Guide to Understanding Attention Deficit Hyperactivity Disorder (ADHD) by Patricia O. Quinn & Judith M. Stern (1991).
- ↑ George Sachs, PsyD. Licensed Psychologist. Expert Interview. 9 October 2020.
- ↑ Why Is My Child’s ADHD Not Better Yet? Recognizing The Undiagnosed Secondary Conditions That May Be Affecting Your Child’s Treatment by David Gottlieb, Thomas Shoaf, and Risa Graff (2006).
- ↑ George Sachs, PsyD. Licensed Psychologist. Expert Interview. 9 October 2020.
- ↑ George Sachs, PsyD. Licensed Psychologist. Expert Interview. 9 October 2020.
- ↑ Putting On The Brakes: Young People’s Guide to Understanding Attention Deficit Hyperactivity Disorder (ADHD) by Patricia O. Quinn & Judith M. Stern (1991).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Why Is My Child’s ADHD Not Better Yet? Recognizing The Undiagnosed Secondary Conditions That May Be Affecting Your Child’s Treatment by David Gottlieb, Thomas Shoaf, and Risa Graff (2006).
- ↑ On Their Own: Creating an Independent Future for Your Child With Learning Disabilities and ADHD by Anne Ford (2007).
- ↑ On Their Own: Creating an Independent Future for Your Child With Learning Disabilities and ADHD by Anne Ford (2007).
- ↑ George Sachs, PsyD. Licensed Psychologist. Expert Interview. 9 October 2020.
- ↑ The Everything Parent’s Guide to Children With ADD/ADHD: A Reassuring Guide to Getting The Right Diagnosis, Understanding Treatments, And Helping Your Child Focus by Linda Sonna (2005).
- ↑ The Everything Parent’s Guide to Children With ADD/ADHD: A Reassuring Guide to Getting The Right Diagnosis, Understanding Treatments, And Helping Your Child Focus by Linda Sonna (2005).
- ↑ George Sachs, PsyD. Licensed Psychologist. Expert Interview. 9 October 2020.
- ↑ Creating an IEP/504 Plan For Your ADHD Child: 11 Action Steps and 40 Great Accommodations, (2013) found at http://assets.addgz4.com/pub/free-downloads/pdf/CreatingAnIEP504forYourADHDChild.pdf
- ↑ ADD/ADHD Behavior-Change Resource Kit by Grad L. Flick (1998).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Organize Your ADD/ADHD Child: A Practical Guide For Parents by Cheryl R. Carter (2011).
- ↑ Organize Your ADD/ADHD Child: A Practical Guide For Parents by Cheryl R. Carter (2011).
- ↑ Organize Your ADD/ADHD Child: A Practical Guide For Parents by Cheryl R. Carter (2011).
- ↑ Putting On The Brakes: Young People’s Guide to Understanding Attention Deficit Hyperactivity Disorder (ADHD) by Patricia O. Quinn & Judith M. Stern (1991).
- ↑ Dr. Larry’s Silver’s Advice to Parents on ADHD by Larry N. Silver (1999).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Dr. Larry’s Silver’s Advice to Parents on ADHD by Larry N. Silver (1999).
- ↑ ADHD and the Nature of Self-Control by Russell A. Barkley (1997).
- ↑ Dr. Larry’s Silver’s Advice to Parents on ADHD by Larry N. Silver (1999).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Dr. Larry’s Silver’s Advice to Parents on ADHD by Larry N. Silver (1999).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Dr. Larry’s Silver’s Advice to Parents on ADHD by Larry N. Silver (1999).
- ↑ Dr. Larry’s Silver’s Advice to Parents on ADHD by Larry N. Silver (1999).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Organize Your ADD/ADHD Child: A Practical Guide For Parents by Cheryl R. Carter (2011).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Brainstorms: Understanding and Treating the Emotional Storms of Attention Deficit Hyperactivity Disorder from Childhood Through Adulthood by H. Joseph Horacek, Jr. (1998).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Why Is My Child’s ADHD Not Better Yet? Recognizing The Undiagnosed Secondary Conditions That May Be Affecting Your Child’s Treatment by David Gottlieb, Thomas Shoaf, and Risa Graff (2006).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Organize Your ADD/ADHD Child: A Practical Guide For Parents by Cheryl R. Carter (2011).
- ↑ Organize Your ADD/ADHD Child: A Practical Guide For Parents by Cheryl R. Carter (2011).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ Why Is My Child’s ADHD Not Better Yet? Recognizing The Undiagnosed Secondary Conditions That May Be Affecting Your Child’s Treatment by David Gottlieb, Thomas Shoaf, and Risa Graff (2006).
- ↑ Organize Your ADD/ADHD Child: A Practical Guide For Parents by Cheryl R. Carter (2011).
- ↑ Taking Charge of ADHD: The Complete, Authoritative Guide For Parents by Russell A. Barkley (2005).
- ↑ ADHD and the Nature of Self-Control by Russell A. Barkley (1997).
- ↑ Fight Back With Food by Tana Amen, R.N. in ADDitude Magazine (Winter 2014).
- ↑ Making Sense of Foods—Carbohydrates: Simple versus Complex at http://www.nutritionmd.org/nutrition_tips/nutrition_tips_understand_foods/carbs_versus.html
- ↑ Fight Back With Food by Tana Amen, R.N. in ADDitude Magazine (Winter 2014).
- ↑ Fight Back With Food by Tana Amen, R.N. in ADDitude Magazine (Winter 2014).
- ↑ Healthy Diet at http://www.cdc.gov/actagainstaids/campaigns/hivtreatmentworks/livewell/healthydiet.html
- ↑ Fight Back With Food by Tana Amen, R.N. in ADDitude Magazine (Winter 2014).
- ↑ Healthy Diet at http://www.cdc.gov/actagainstaids/campaigns/hivtreatmentworks/livewell/healthydiet.html
- ↑ Fight Back With Food by Tana Amen, R.N. in ADDitude Magazine (Winter 2014).
- ↑ Vitamins and Supplements for ADHD at http://www.nature.com/ejcn/journal/v67/n1/full/ejcn2012177a.html
- ↑ Fight Back With Food by Tana Amen, R.N. in ADDitude Magazine (Winter 2014).
- ↑ Fight Back With Food by Tana Amen, R.N. in ADDitude Magazine (Winter 2014).
- ↑ What Causes ADHD? (by National Institute of Mental Health) found at http://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder/index.shtml?rf=71264#pub3
- ↑ What Causes ADHD? (by National Institute of Mental Health) found at http://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder/index.shtml?rf=71264#pub3
- ↑ What Causes ADHD? (by National Institute of Mental Health) found at http://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder/index.shtml?rf=71264#pub3
- ↑ On Their Own: Creating an Independent Future for Your Child With Learning Disabilities and ADHD by Anne Ford (2007).
- ↑ http://www.webmd.com/add-adhd/guide/adhd-stimulant-therapy
- ↑ http://www.webmd.com/add-adhd/guide/adhd-nonstimulant-drugs-therapy
- ↑ What Medications Are Used to Treat ADHD? (by National Institute of Mental Health) found at http://www.nimh.nih.gov/health/topics/mental-health-medications/mental-health-medications.shtml#part_149868
- ↑ http://pediatrics.aappublications.org/content/early/2011/10/14/peds.2011-2654.full.pdf
- ↑ http://pediatrics.aappublications.org/content/early/2011/10/14/peds.2011-2654.full.pdf
- ↑ What Medications Are Used to Treat ADHD? (by National Institute of Mental Health) found at http://www.nimh.nih.gov/health/topics/mental-health-medications/mental-health-medications.shtml#part_149868
- ↑ http://www.nlm.nih.gov/medlineplus/druginfo/meds/a601059.html
- ↑ What Causes ADHD? (by National Institute of Mental Health) found at http://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder/index.shtml?rf=71264#pub3
- ↑ http://psychcentral.com/blog/archives/2012/06/07/12-best-tips-for-coping-with-adhd/
- ↑ What Causes ADHD? (by National Institute of Mental Health) found at http://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder/index.shtml?rf=71264#pub3
About This Article
To help your child manage their ADHD, try to maintain a structured daily routine, since consistency can help alleviate a lot of their stress. You can even write your child’s schedule on a whiteboard in the kitchen or living room, so they can clearly see what they need to do and keep on track. It’s easy for children with ADHD to feel overwhelmed by tasks, so try breaking them down into smaller steps whenever possible to help them stay motivated. For example, if you want them to unload the dishwasher, first encourage them to unload all the plates, and praise them before moving onto the glasses. It can be frustrating when you need to discipline your child, but make sure to enforce the punishment immediately, since children with ADHD often struggle with time concepts and benefit from being told right away what they’ve done wrong. For instance, if they get aggressive with you, punish their behavior right away instead of waiting until they've calmed down. For more tips from our Counselor co-author, including how to help your child with ADHD succeed at school, read on!





























































-Step-37.webp)
















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...