This article was co-authored by Trudi Griffin, LPC, MS. Trudi Griffin is a Licensed Professional Counselor in Wisconsin specializing in Addictions and Mental Health. She provides therapy to people who struggle with addictions, mental health, and trauma in community health settings and private practice. She received her MS in Clinical Mental Health Counseling from Marquette University in 2011.
There are 15 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 186,852 times.
If you've taken mind-altering or hallucinogenic drugs, you may be familiar with changes in your visual perception. If you experience these changes regularly, you may have what is known as Hallucinogen-Persistent Perception Disorder (HPPD). This condition is defined by the after effects that sometimes come from taking hallucinogenic drugs or other consciousness altering substances.[1] While there's no recognized treatment for HPPD, you can learn to manage the symptoms.
Steps
Recognizing Hallucinogen-Persistent Perception Disorder
-
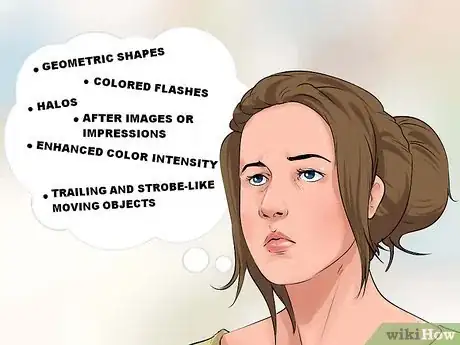
1Recognize the symptoms of Hallucinogen-Persistent Perception Disorder (HPPD). Flashbacks are the trademark symptom of HPPD. You may notice that you continue to have flashbacks beyond the few days after drug use. You may also experience persistent changes in your perception after taking hallucinogenic drugs. If you have perception changes, you may see:[2]
- Geometric shapes
- Objects in your peripheral vision (along the sides or edges of sight)
- Colored flashes
- Enhanced color intensity
- Trailing and strobe-like moving objects
- After images or impressions
- Halos
- Objects that appear small or large
-
2Learn how HPPD impacts your physical health. Changes in perception can be annoying or even frightening, but they aren't necessarily a sign of any serious physical damage that is life threatening.[3] Any alterations in brain chemistry are related to how you see things, not how your body generally functions.[4] These alterations are also distinctly different from hallucinations since they're clearly not associated with what's happening in the present moment. Changes in perception shouldn't be confused with reality.
- Any serious health consequences of HPPD aren't caused by brain damage from whatever drug was used. Instead, health problems typically come from sustained depression or anxiety associated with the persistent flashbacks.[5]
Advertisement -
3Be prepared to feel disconnected. You may feel depersonalized, or drastically disconnected from your body. For example, you may feel as though you're watching yourself from an outside perspective or from outside your body.[6] This feeling of disconnect can also be accompanied by a sense that you're in a dreamlike state or that the world isn't a real place.
- Like other HPPD symptoms, this can be frightening and last for an unknown period of time. But, it's not necessarily a sign of serious physical damage that needs immediate treatment.
-
4Consider the severity of your symptoms. Sometimes people who use hallucinogenic drugs notice visual disturbances in the weeks after use, while sometimes they last for years.[7] Since this varies by individual, there’s really no clear way of knowing how long your visual disturbances will last. You most likely won't need to treat HPPD as if it was a serious health condition. But, if you have difficulty functioning, struggle to go to work or school, or can't interact with people, you may need to consider treatment for the symptoms.
- Even people who are affected by perceptual disturbances for years can go onto live a functioning lives despite the alterations. Some people have even reported pleasurable alterations in perception, with no desire for them to dissipate.[8]
Managing Hallucinogen-Persistent Perception Disorder
-
1Know when to get professional help. If you've used hallucinogenic drugs and are affected by perceptual disturbances to the point that you can't function in your daily life, you should get help. A mental health professional can work with you to discuss lifestyle changes and behavioral therapies. Or, if you see a medical doctor, you might be prescribed medications to alleviate some of the perceptual disturbances, even though there's no cure for HPPD.[9]
- Unfortunately, there's no recognized treatment for the symptom of depersonalization. But, behavioral therapies (like Cognitive Behavioral Therapy), psychoanalysis, and basic relaxation techniques may help reduce symptom severity.[10]
-
2Consult with your doctor about medication to help with the symptoms. While there’s no known cure for HPPD, there are drugs that have been found to alleviate some of the perceptual disturbances.[11] Your doctor may prescribe clonidine, perphenazine and clonazepam.[12] These are primarily effective because they can relax you or temporarily improve the symptoms. But, these medications could have serious long-term side effects if you take them for a long period of time.[13]
- Pay attention to how your body responds to medication and let your doctor know of any harmful side effects. Also, remember that medication won't keep the perceptual alterations away permanently.
-
3Get therapy. You may want to work with a mental health professional, such as a therapist or counselor, to develop coping skills or techniques. This can help you manage the symptoms of HPPD and any anxiety or depression the symptoms may be causing. Working with a therapist can also be helpful if you specifically want help in managing the symptom of depersonalization.[14] Among therapeutic treatments, you might consider:
- Relaxation techniques, including systematic desensitization. These techniques can be useful in dealing with daily situations that may cause you anxiety. When practiced correctly and consistently, relaxation techniques can give you a greater sense of freedom in your everyday life.[15]
- Cognitive-Behavioral Therapy. This takes a typically short-term, problem based approach to the changing your beliefs and perceptions. You should notice a greater sense of well-being by changing your thought processes.
- Psychoanalysis. This focuses on understanding your unconscious desires. Psychoanalysis attempts to make you more comfortable in expressing these desires aloud, first in the therapeutic context and then outside in your everyday life.[16]
-
4Reduce or avoid using any non-prescribed drugs. Consider the effects they could be having on your perception. Any alterations in perception will probably only continue or become more noticeable with continued drug use.[17] This is especially important to consider when taking visually active drugs like LSD, cannabis and psychedelic drugs like magic mushrooms, MDMA, or mescaline.
- You may also want to avoid caffeine, alcohol, and tobacco, or limit their use, until you've figured out how your body reacts to each substance individually.
-
5Create a daily routine. Take things one day at a time and try to simplify your daily routine. Try focusing on the basics, like eating at a consistent schedule, exercising, or even just listening to music. It may be easy for you to become distracted by your flashback experiences, even to a degree that it affects your physical health. By going back to the basics, you may be able to start feeling grounded in your world again.
- Your routine doesn't have to be complicated. Even doing something as simple as going to bed or waking up at the same times every day can give you stability and focus your attention.[18]
-
6Create a support network. You should be around people that support you as often as you can. This will make dealing with HPPD symptoms easier, since these people can reinforce a sense of reality in your life. If you don't know of friends or family that you can call upon, consider joining a support group or online community where people experiencing similar symptoms can share their stories with you.
- You may also want to look for support groups that focus with managing anxiety or depression, which are associated with HPPD symptoms.[19]
Warnings
- If you are feeling depressed or suicidal, get immediate help. Be that from friends, family, trusted community leaders, psychiatrists, or through the suicide hotline.⧼thumbs_response⧽
References
- ↑ American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA, American Psychiatric Association, 2013.
- ↑ Hermle, L., Simon, M., Ruchsow, M., & Geppert, M. (2012). Hallucinogen-persisting perception disorder. Therapeutic Advances in Psychopharmacology, 2(5), 199–205. http://doi.org/10.1177/2045125312451270
- ↑ Rathus, S. (2011). Psychology: Concepts and Connections. Cengage Learning.
- ↑ http://www.newyorker.com/tech/elements/a-trip-that-doesnt-end
- ↑ Halpern, J. H., & Pope, H. G. (2003). Hallucinogen persisting perception disorder: what do we know after 50 years? Drug & Alcohol Dependence, 69(2), 109–119. http://doi.org/10.1016/S0376-8716(02)00306-X
- ↑ http://www.medicalnewstoday.com/articles/262888.php
- ↑ Halpern, J. H., & Pope, H. G. (2003). Hallucinogen persisting perception disorder: what do we know after 50 years? Drug & Alcohol Dependence, 69(2), 109–119. http://doi.org/10.1016/S0376-8716(02)00306-X
- ↑ G Lerner, A., Rudinski, D., Bor, O., & Goodman, C. (2014). Flashbacks and HPPD: A Clinical-oriented Concise Review. The Israel Journal of Psychiatry and Related Sciences, 51(4), 296–301.
- ↑ G Lerner, A., Rudinski, D., Bor, O., & Goodman, C. (2014). Flashbacks and HPPD: A Clinical-oriented Concise Review. The Israel Journal of Psychiatry and Related Sciences, 51(4), 296–301.
- ↑ Medford, N., Sierra, M., Baker, D., & David, A. S. (2005). Understanding and treating depersonalisation disorder. Advances in Psychiatric Treatment, 11(2), 92–100. http://doi.org/10.1192/apt.11.2.92
- ↑ G Lerner, A., Rudinski, D., Bor, O., & Goodman, C. (2014). Flashbacks and HPPD: A Clinical-oriented Concise Review. The Israel Journal of Psychiatry and Related Sciences, 51(4), 296–301.
- ↑ Lerner, A. G., Gelkopf, M., Skladman, I., Oyffe, I., Finkel, B., Sigal, M., & Weizman, A. (2002). Flashback and Hallucinogen Persisting Perception Disorder: clinical aspects and pharmacological treatment approach. The Israel Journal of Psychiatry and Related Sciences, 39(2), 92–99.
- ↑ Hartung, B., Sampson, S., & Leucht, S. (2015). Perphenazine for schizophrenia. The Cochrane Database of Systematic Reviews, 3, CD003443. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003443.pub3/full
- ↑ http://www.medicalnewstoday.com/articles/262888.php
- ↑ Johnson, W. R., & L, W. (1997). Gestalt empty-chair dialogue versus systematic desensitization in the treatment of a phobia. Gestalt Review, 1(2), 150–162.
- ↑ Fink, B. (1999). A Clinical Introduction to Lacanian Psychoanalysis: Theory and Technique. Harvard University Press.
- ↑ G Lerner, A., Rudinski, D., Bor, O., & Goodman, C. (2014). Flashbacks and HPPD: A Clinical-oriented Concise Review. The Israel Journal of Psychiatry and Related Sciences, 51(4), 296–301.
- ↑ https://www.psychologytoday.com/blog/may-i-have-your-attention/201103/using-little-routines-create-stability
- ↑ http://www.adaa.org/supportgroups