This article was medically reviewed by Janice Litza, MD. Dr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
There are 13 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 89% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 94,713 times.
Research shows that tuberculosis, or TB, is spread through airborne droplets from a sick person's sneeze, cough, or laugh.[1] It's an infection of the bacteria Mycobacterium tuberculosis, and while it usually starts in the lungs, it can spread to other parts of the body, like the spine or the brain. If you think you might have TB, it is important to see a doctor right away and get medications to treat it. Studies show that with a course of medication, you can recover from tuberculosis without many lasting effects.[2] Always take the full course of your medication, even after you feel better, to avoid drug-resistant strains of TB from forming.
Steps
Recognizing Tuberculosis
-
1Go to the doctor if you might have active TB. If you have active TB you are infectious. TB is usually active right after the initial infection and at points years later when it resurges. The symptoms of TB are similar to those of some other diseases, so it's important to be evaluated by a doctor to make sure you receive the correct diagnosis. Symptoms of active TB include:[3] [4] [5]
- Coughing that lasts at least three weeks
- Coughing up blood
- Chest pain
- Discomfort when breathing or coughing
- Fever
- Chills
- Night sweats where you wake up soaking wet
- Exhaustion
- Loss of appetite
- Weight loss
-
2Get screened if you are vulnerable to latent TB. People with TB often go through periods, even years, when the bacteria remain in their bodies but cause no symptoms. Latent TB can resurge into active TB. If you are vulnerable to TB and there is a possibility you were exposed to the bacteria or you are showing symptoms, then it is important you get tested. People who are at a higher risk for carrying latent TB include:[6]
- People with suppressed immune systems, such as those with HIV/AIDS
- People with diabetes, serious kidney disease, and some forms of cancer
- People undergoing chemotherapy or taking drugs to prevent their bodies from rejecting transplanted organs
- People taking certain drugs for rheumatoid arthritis, Crohn’s disease and psoriasis
- IV drug users and smokers
- Family members and people in close contact with an infected person
- Healthcare workers who treat people with a high risk
- People suffering severe malnutrition
- Children and the elderly
- People living or working in crowded residential facilities including prisons, immigration centers, nursing homes, or refugee camps
- People who have traveled or lived in Africa, Eastern Europe, Asia, Russia, Latin America, or the Caribbean Islands
Advertisement -
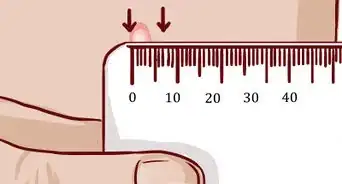
3Undergo tests if your doctor recommends it. When you go for an exam, the doctor will likely listen to your lungs and palpate your lymph nodes to for signs of infection. There are several tests that the doctor may also want you to have. These include:[7] [8]
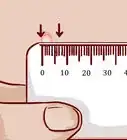
- A skin test. During this test the doctor injects PPD tuberculin under the skin of your forearm. After two to three days the doctor will look at the site to see if you have a bump. If you do, it suggests you may have TB. This test can produce both false positives and false negatives. You may produce a false positive if you have received the bacillus Calmette-Guerin vaccine against TB. You may give a false negative if you’ve been infected so recently that you have not yet mounted an immune response.
- A blood test. The blood test is more sensitive and more accurate than the skin test. The doctor will likely order the blood test if there is reason to doubt the results of the skin test.
- Imaging tests. If your skin test came out positive, the doctor will likely want to check your lungs with an X-ray, a CT scan, or an endoscopy. During an endoscopy, a small camera on a long tube is inserted into your body to allow the doctor to examine the infected area more closely. If the doctor expects that the TB has infected an area of your body beyond the lungs, the doctor may request a CT, MRI, or ultrasound scan of that area too.
- A biopsy of the infected area. The sample would then be tested for TB bacteria.
- Sputum tests. The doctor is likely to request a sputum test if the image tests show evidence of an infection. The samples can be used to determine what strains of TB you have. This helps the doctor select the right medications for you. A positive result for TB will be available in one to two days, but it can take up to one to two months for the specific strain to be identified. These results are important for refining a course of treatment for drug-resistant TB. This test is also used to monitor someone with active TB — once you return negative sputum test, then you will be removed from quarantine and no longer be considered infectious.
Treating Your Tuberculosis
-
1Take medications. Most tuberculosis treatments require taking medications for six to nine months. Which medications you are prescribed will depend on which strain of TB you have. TB medications can damage your liver, so tell your doctor if you have any liver problems. Common medications include:[9] [10]
- Isoniazid. This medication can cause nerve damage. Tell your doctor if your hands or feet feel numb or tingle. You will also be given vitamin B6 to lessen the risk.
- Rifampin (Rifadin, Rimactane, Rifampicin). This medication can interfere with some types of birth control, including the combined contraceptive pill. If you are given this medication, use condoms as a backup method of birth control.
- Ethambutol (Myambutol). This medication can be harmful to your eyes. If you receive this medication, you should have a vision test when you start taking it.
- Pyrazinamide. This will be used in conjunction with other medications and may cause mild joint or muscle pain.
-
2Ask your doctor if you have drug-resistant TB. If so, you may need to take a combination of drugs and possibly take some newer medications to which the TB is less likely to be resistant. You may also need to take medications for a year-and-a-half to two-and-a-half years. Tell your doctor before you start if you have a history of liver problems. Possible medications include:[11]
- Fluoroquinolone antibiotics
- Injectable medications such as amikacin, kanamycin, or capreomycin
- Bedaquiline
- Linezolid
-
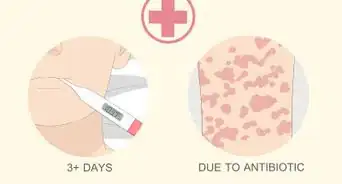
3Tell your doctor if you experience side effects. Tuberculosis medications can damage your liver, so it is very important to notify your doctor if you experience side effects. If you have side effects from the medications, do not stop taking them. This can produce a drug resistant strain. Instead, talk to your doctor to discuss what you can do to switch to another medication or alleviate the side effects. Possible side effects include:[12] [13]
- Nausea
- Vomiting
- Lack of hunger
- Jaundice
- Passing dark urine
- A fever for three or more days
- Tingling or loss of feeling in your extremities
- Blurred vision
- A rash or itchiness
-
4Avoid spreading the infection to others. You will probably not need to be quarantined during your treatment; however, you should be careful to minimize the likelihood of transmitting it. You can do this by:[14]
- Staying home from work or school until your doctor says you can return
- Not sharing a room when you sleep
- Covering your mouth when you cough, sneeze, or laugh
- Opening windows to bring in fresh air
- Throwing used tissues away in a sealed bag
-
5Complete the course of medications. After a few weeks you will probably start to feel better. This doesn’t mean that you are cured, so do not stop taking the antibiotics. Keep taking the medications exactly as prescribed.
- If you stop the medications before the TB is fully eradicated from your system, the surviving bacteria may become resistant to the drugs you took. This means that when you get sick again with it, it will be harder to treat.[15]
Preventing Tuberculosis
-
1Discuss the vaccine with your doctor. In places where TB is more common, infants are often vaccinated with the bacillus Calmette-Guerin (BCG) vaccine against TB. The vaccine is not routinely given in the US, but if you expect to be at a higher risk, then ask your doctor if it is likely to be useful for you. You may be at a higher risk if:[16]
- You will be living and working in a country where TB is more common.
- You have a lowered immune system making you more vulnerable to contracting TB if you are exposed. People who have a higher risk are those who have HIV/AIDS, who are taking immune suppressing medications, or are receiving chemotherapy.
-
2Wear a respirator around a family member with TB. TB is spread through droplets, so if you wear a respirator it lessens your chances of infection if you live with someone who has recently been diagnosed. You cannot wear just any surgical or medical mask, however. You must wear a specific respirator mask (such as N95 disposable respirators) to protect yourself from TB. The person with TB should also wear a respirator. Keep the respirator on for the first three weeks of treatment. In addition, the infected person should:
- Open windows to ventilate the room she is in.
- Sleep in a separate room to reduce the amount of time you spend breathing the same air.
- Stay home from work or school.
-
3Help a loved one with TB finish the entire course of treatment. The treatment requires a long course of medications, but it is important that they be completed without skipping any doses. This protects both the infected person and those around him, because:
- It reduces the likelihood of the bacteria developing resistance to the medications.
- Drug resistant strains are much more difficult to eradicate if they spread to others.
Expert Q&A
-
QuestionHow long is a patient with TB contagious?
 Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Board Certified Family Medicine Physician You are considered contagious only if you have been diagnosed with active tuberculosis, not latent, and will be tested through sputum regularly while taking medicine until the cultures are negative, then you are no longer considered contagious. This can take weeks to months depending on your health.
You are considered contagious only if you have been diagnosed with active tuberculosis, not latent, and will be tested through sputum regularly while taking medicine until the cultures are negative, then you are no longer considered contagious. This can take weeks to months depending on your health. -
QuestionWhen are you done with TB testing?
 Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Board Certified Family Medicine Physician This depends on the result and your job. Healthcare and other people who work in higher risk settings are tested every one to two years. If you have been positive on the screening tests, you will always be positive and need to have more detailed questions to see if you are “active” or not and might require a chest x-ray or sputum testing.
This depends on the result and your job. Healthcare and other people who work in higher risk settings are tested every one to two years. If you have been positive on the screening tests, you will always be positive and need to have more detailed questions to see if you are “active” or not and might require a chest x-ray or sputum testing. -
QuestionWhat is the first step we take if we find out we are infected?
 Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Board Certified Family Medicine Physician Contact a local health department or infectious disease specialist and they will direct you to treatment and support centers that will give you more specific information on how to protect yourself and others.
Contact a local health department or infectious disease specialist and they will direct you to treatment and support centers that will give you more specific information on how to protect yourself and others.
References
- ↑ https://www.cdc.gov/tb/topic/basics/howtbspreads.htm
- ↑ https://www.cdc.gov/tb/topic/treatment/ltbi.htm
- ↑ https://my.clevelandclinic.org/health/diseases/11301-tuberculosis
- ↑ http://www.nhs.uk/conditions/Tuberculosis/Pages/Introduction.aspx
- ↑ https://www.nlm.nih.gov/medlineplus/tuberculosis.html
- ↑ https://www.cdc.gov/tb/topic/basics/tbinfectiondisease.htm
- ↑ https://www.cdc.gov/tb/publications/factsheets/testing/tb_testing.htm
- ↑ http://www.nhs.uk/Conditions/Tuberculosis/Pages/Diagnosis.aspx
- ↑ https://my.clevelandclinic.org/health/diseases/11301-tuberculosis
- ↑ http://www.nhs.uk/Conditions/Tuberculosis/Pages/Treatment.aspx
- ↑ https://www.cdc.gov/tb/topic/drtb/default.htm
- ↑ https://www.healthywa.wa.gov.au/Articles/J_M/Medications-to-treat-tuberculosis
- ↑ http://www.nhs.uk/Conditions/Tuberculosis/Pages/Treatment.aspx
- ↑ http://www.nhs.uk/Conditions/Tuberculosis/Pages/Treatment.aspx
- ↑ https://www.healthywa.wa.gov.au/Articles/J_M/Medications-to-treat-tuberculosis
- ↑ https://www.cdc.gov/tb/topic/basics/risk.htm
- ↑ http://www.cdc.gov/tb/publications/factsheets/general/nonhealthcare_employers.htm
About This Article
To cure tuberculosis, go to your doctor if you spot the symptoms of active TB, like coughing that lasts longer than 3 weeks, coughing up blood, or chest pain. At the appointment, your doctor will listen to your lungs to check for infection, and may recommend that you take a skin test or blood test. If a diagnosis is confirmed, take the medication prescribed by your doctor for 6 to 9 months. Since some medications can damage your liver, tell your doctor if you have a history of liver problems. During your treatment, stay home from work until your doctor advises it, and don’t share a room when you sleep. Even if you start feeling better, continue to take your medication as prescribed, since it’s vital that all of the bacteria are eliminated. For tips from our Medical co-author, including how to prevent tuberculosis, keep reading!


















-Step-11.webp)















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...