Biofilms are bacteria that have formed a gated community. Biofilms are composed of an aggregate of bacterial cells and are essentially considered a multi-cellular organism. They are characterized by structural heterogeneity, genetic diversity, complex community interactions, and an extracellular matrix of polymeric substances. They live on solid surfaces (e.g., catheters, ) and the extracellular material they produce protects them from external threats, such as attacks by the body's immune cells. The property of biofilms constitute a penetration barrier for most antibiotics therefore preventing the drug from reaching the microbes. It is being widely recognized that bacterial biofilms are responsible for several chronic diseases that are difficult to treat, hence hard to eradicate (e.g., cystitis, endocarditis, urinary tract infections, gingivitis, dental plaque, and other yet to be identified conditions). They differ from free-floating or planktonic bacteria that cause acute infections and are managed by antimicrobial drugs.
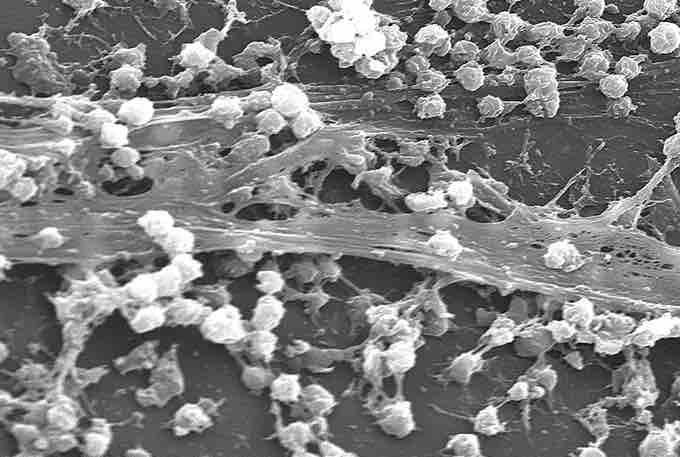
Staphylococcus aureus biofilm
Staphylococcus aureus forming a biofilm on a catheter.
Persisters are multidrug tolerant cells present in all bacterial populations. Bacterial populations that produce persister cells that neither grow nor die in the presence of microbicidal antibiotics are largely responsible for high levels of biofilm tolerance to antimicrobials. Persisters are not mutants, but rather phenotypic variants of the wild-type that upon inoculation produce a culture with similar levels of tolerance. Elimination of persisters remains an obstacle for the eradication of some tenacious and highly recurrent bacterial infections. Biofilms and persisters are the cause of multidrug tolerance. Multidrug tolerance differs from multidrug resistance in that it is not caused by mutant microbes but rather by microbial cells that exist in a transient, dormant state. These non-dividing cells often survive antibiotic exposure targeted to kill highly proliferating bacteria.