This article was medically reviewed by Wendy Powell and by wikiHow staff writer, Danielle Blinka, MA, MPA. Wendy Powell is a Maternal Health and Exercise Specialist and the Founder and CEO of MUTU System, the world's best-selling, medically recommended online fitness education program for mothers. Wendy specializes in pregnancy, post-baby recovery, postpartum exercises, fitness education, and body confidence. Wendy works to shift the conversation on women's bodies towards equality and empowerment for health, confidence, and power. She is a published author, international speaker, and award-winning entrepreneur. Wendy is on the Women's Development Board of the MicroLoan Foundation and is a frequent contributor to the BBC. MUTU System has been featured in Vogue, the Huffington Post, Fox News Health, Daily Mail, and The Guardian, and is recommended by Hollywood Trainer, Jeanette Jenkins.
There are 7 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 16,135 times.
Feeling pelvic pain while you’re pregnant can be really scary, so you likely want relief fast. Pelvic pain occurs in the lower part of your torso between your abdomen and your hipbones. This pain may be normal as your body adjusts to allow your baby to grow bigger, but sometimes it’s a cause for concern.[1] Before you try to relive your pelvic pain, determine what’s causing it so you get the right type of care. Then, there are pain treatments and lifestyle changes you can try. However, you may need to call or visit your doctor for medical treatment.
Steps
Determining the Cause of Your Pain
-
1Notice if your pain is sharp or dull with no other symptoms. While it might make you nervous, it’s totally normal to experience pelvic pain while you’re pregnant. Your hips and pelvis are spreading to accommodate a growing baby, which causes pain. Try not to worry if your pain comes and goes and you don’t have any other symptoms. It's likely that you're having normal pregnancy pains.[2]
- If you start to feel worried, call your doctor to make sure your pain is just normal pregnancy pains. They can advise you on whether or not you need to be concerned.
-
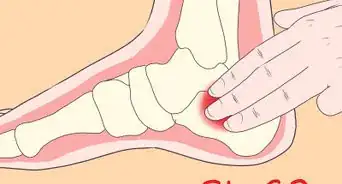
2Recognize the symptoms of pelvic girdle pain (PGP). This condition is normal and affects 1 in 5 pregnant women, but you may be at an increased risk for it if you have had damage to your pelvic region previously, your joints move unevenly, or if your baby is large or positioned in a certain way. PGP can cause you a lot of pain and may affect your mobility, but you can find relief with pain relievers and lifestyle changes. Visit your doctor if you think you have PGP so you can discuss your treatment options. To determine if you may have PGP, check if you have the following symptoms:[3]
- Pain at the center of your pubic bone
- Pain that goes across 1 or both sides of your back
- Pain in your perineum (the area between your vagina and anus)
- Widening of your thighs
- Clicking or grinding in your pelvic area
- Worsening pain while you stand, walk, go up or down stairs, stand on 1 leg, spread your legs, extend your legs, place bilateral pressure on the trochanters (where your leg connects to your hip), or turn over
Did You Know? Pelvic girdle pain can occur during any trimester and can range from mild to severe. It won’t hurt your baby, so you don’t need to worry.[4]
Advertisement -
3Look for signs of labor if you’re past 35 weeks. Sometimes pelvic pain is an early sign of labor, especially if you’re late in your third trimester. If labor is causing your pelvic pain, you’ll notice other signs of early labor, as well.[5] Go to the hospital if you have these signs of labor:[6]
- Contractions, which feel like a painful tightening and release
- Pink or reddish discharge
- Backache
- A persistent urge to use the restroom
- Your water breaking
-
4See your doctor if you’re bleeding to make sure it’s not a miscarriage. This is really scary, but try not to worry. While pelvic pain with bleeding can mean you’re having a miscarriage, this isn’t always the case. Benign spotting is possible in the first 1 to 3 months of pregnancy, but it’s important to get evaluated anyway. Go to your doctor or the emergency room immediately so you and your baby can get treatment.[7]
- Ask someone to take you to the doctor or emergency room so that you don’t have to drive.
-
5Get emergency treatment if you're lightheaded or your heart is racing. While you likely don’t need to worry, pelvic pain, lightheadedness, and a racing heartbeat are signs of an ectopic pregnancy. This isn’t very common, but go to the emergency room to be safe. They’ll check you out to make sure that everything is okay.[8]
- An ectopic pregnancy occurs when your fertilized embryo attaches to your fallopian tube instead of in your uterus. Since your fallopian tube is too narrow for the baby to grow, your health is at risk if you don’t get treatment.
Using Pain Treatments
-
1Take acetaminophen (Tylenol) for pain relief, if your doctor okays it. You’re probably worried about taking something that might hurt your baby, including pain relievers. Generally, acetaminophen is safe to take during pregnancy. However, talk to your doctor first to make sure it’s safe for you. Then, take it as directed on the bottle to relieve your pelvic pain.[9]
- You might find that acetaminophen isn’t enough to help with your pain. Talk to your doctor about your other options. They may recommend a different pain reliever, but acetaminophen is the safest during pregnancy.
-
2Apply a warm compress to your pelvic area for 15-20 minutes. Use a heating pad or a warm washcloth as a warm compress. Drape the warm compress across your pelvic area to relieve your pain. Leave the compress in place for about 15-20 minutes. Repeat as often as you like.[10]
- Ask your doctor if it’s safe to use a self-warming patch that’s designed for period cramps. These will apply warmth to your pelvic area for up to 8 hours.
-
3Take a warm bath or shower to soothe your pain. Run a bath that is comfortably warm but not hot. Alternatively, take a shower if you’re comfortable standing. Then, soak or stand in the warm water for about 15-20 minutes to soothe your pelvic pain.[11]
- If possible, place a shower chair in your shower so you can sit and relax under the water.
-
4Try a TENS unit to relieve ongoing PGP. A transcutaneous electrical nerve stimulation unit or TENS unit stimulates your muscles with a gentle electrical current. This may help to relieve pelvic girdle pain for some people.[12]
- See a physical therapist and ask about this option. A physical therapist may be able to show you how to connect the electrodes and help you use the TENS unit for the first time.
- If a TENS unit brings you relief, you might consider buying one for personal use.
-
5See an acupuncturist for a pain relief treatment. Acupuncture is really helpful for relieving pelvic pain during pregnancy, especially if it’s caused by PGP. Look for an acupuncturist who has experience in treating pregnant women. Then, tell your acupuncturist where you’re experiencing pain. During your treatment, the acupuncturist will insert thin needles into your skin to relieve your pain.[13]
- Acupuncture typically doesn’t hurt, but you might feel some discomfort.
- Talk to your doctor before you get acupuncture.
Making Lifestyle Changes
-
1Wear a maternity support belt to help reduce your pelvic pain. A pelvic support belt will take some of the pressure off your body, especially your back. This helps relieve pain in your pelvis, hips, and lower back. Choose a maternity support belt that feels comfortable to you, then wear it every day.[14]
- Some maternity support belts go under your belly to help support it. Others have a top band that goes over your belly and a bottom band that goes under your belly for added support. Both are great options, so pick what’s comfortable to you.
- You can get a maternity support belt at a maternity store, some department or drug stores, or online.
-
2Choose flat, supportive shoes to minimize the stress on your body. Pregnancy changes your posture and weight distribution, which causes pain. Wearing comfortable, supportive shoes can help minimize your pain. Pick ballet flats or comfortable sneakers that have cushioning and arch support.[15]
- Even a low heel can put more pressure on your hips, pelvis, and lower back. Avoid wearing any type of heel while you’re pregnant.
-
3Sleep on your side with a pillow between your knees and under your tummy. Turn onto the side that’s most comfortable for you. Then, place a pillow under your belly to support it. Additionally, put a pillow between your legs to support your hips, pelvis, and back.This will help you stay comfortable.[16]
- Supporting your hips and belly with pillows can help you rest better and wake up with less pain.
-
4Do Kegel exercises to strengthen your pelvic floor.[17] Use the restroom so that your bladder is empty. Then, lie or sit in a comfortable position. Tighten your pelvic floor muscles like you would to stop a stream of urine. Hold for 5 seconds, then repeat for 5 repetitions.[18]
- Do 2-3 sets of Kegels every day to see results.
- After you get used to the exercise, increase the time you hold your Kegels to 10 seconds per rep and increase your reps to 10 per session.
-
5Engage in light activity but don’t push yourself too far. Light exercise can help prevent and relieve pregnancy pain, including pelvic pain.[19] Talk to your doctor find out which exercises are safe for you. For instance, you can probably go for walks or do some gentle exercises in water.[20]
- The exercises you can do will depend on your activity level before you got pregnant. Your doctor can help you choose the right exercises for you.
Tip: Don’t sit for longer than 30 minutes at a time during the day. Too much inactivity can worsen your pain.[21]
-
6Avoid activities that trigger your pain. Keep track of the things that cause your pelvic pain, like picking up heavy objects or walking down stairs. Then, do your best to avoid these triggers so you have less pain. When you can’t avoid something, minimize how often you do it.[22]
- For example, going up the stairs is a common trigger for pelvic pain. If you have stairs in your home, you may have to go up them. However, you can minimize your trips upstairs.
Tip: Don’t stoop, bend, or lift heavy objects. These activities will likely trigger your pain.
-
7Ask for help with household chores and shopping. You might feel like you have to do everything, but right now your primary concern is your baby. Tell your family members, friends, or roommates that you need support right now. Ask them to divvy up the chores so that you’re not pushed to the point of pain.[23]
- Say, “The baby is causing me a lot of pain right now, so I need to rest more. Can you handle the cleaning and grocery shopping this week?”
- Don’t feel guilty about asking them to help. You need to put you and your baby first.
-
8Rest with your back supported when you’re feeling pain. When your pain starts, take a break and relax. Sit in a comfortable chair and place a pillow behind your back for added support. This will take the pressure off your back and pelvis so you can start to feel better.[24]
- Relax for up to 30 minutes until you feel better. It’s best to get up and walk around after 30 minutes so you don’t get stiff, which may make your pain worse.
Getting Medical Treatment
-
1Visit your doctor to get a diagnosis and discuss your treatment needs. If your pain persists, go to your doctor to find out what’s causing it. They’ll discuss your symptoms and examine you to figure out what’s causing your pain. Then, they’ll tell you if you need treatment and what kind of treatment you need.[25]
- Tell your doctor how long you’ve been experiencing pain, as well as any other symptoms you have.
-
2Call your doctor or go to the hospital if you think you’re in labor. You may not need to go to the hospital in the early stages of labor, but you should call your doctor. They’ll tell you when to go to the hospital to deliver your baby. If you’re worried, go ahead and go to the hospital.[26]
- The hospital may send you home if you’re not far progressed in labor.
-
3See a physiotherapist, osteopath, or chiropractor for an adjustment. Look for a specialist who is experienced in treating pregnant women. They can manually manipulate your muscles and joints to help you get relief. Ask your doctor for a referral or look for a specialist online.[27]
- Your appointment may be covered by your insurance, so check your benefits.
References
- ↑ https://www.merckmanuals.com/home/women-s-health-issues/symptoms-during-pregnancy/pelvic-pain-during-early-pregnancy
- ↑ https://www.merckmanuals.com/home/women-s-health-issues/symptoms-during-pregnancy/pelvic-pain-during-early-pregnancy
- ↑ https://www.nhs.uk/conditions/pregnancy-and-baby/pelvic-pain-pregnant-spd/
- ↑ https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-pelvic-girdle-pain-and-pregnancy.pdf
- ↑ https://www.merckmanuals.com/home/women-s-health-issues/symptoms-during-pregnancy/pelvic-pain-during-early-pregnancy
- ↑ https://www.nhs.uk/conditions/pregnancy-and-baby/labour-signs-what-happens/
- ↑ https://www.merckmanuals.com/home/women-s-health-issues/symptoms-during-pregnancy/pelvic-pain-during-early-pregnancy
- ↑ https://www.merckmanuals.com/home/women-s-health-issues/symptoms-during-pregnancy/pelvic-pain-during-early-pregnancy
- ↑ https://www.merckmanuals.com/home/women-s-health-issues/symptoms-during-pregnancy/pelvic-pain-during-early-pregnancy
- ↑ https://www.merckmanuals.com/home/women-s-health-issues/symptoms-during-pregnancy/pelvic-pain-during-early-pregnancy
- ↑ https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-pelvic-girdle-pain-and-pregnancy.pdf
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5367222/
- ↑ https://www.health.gov.au/resources/pregnancy-care-guidelines/part-i-common-conditions-during-pregnancy/pelvic-girdle-pain
- ↑ https://www.nhs.uk/conditions/pregnancy-and-baby/pelvic-pain-pregnant-spd/
- ↑ https://www.nhs.uk/conditions/pregnancy-and-baby/pelvic-pain-pregnant-spd/
- ↑ https://www.merckmanuals.com/home/women-s-health-issues/symptoms-during-pregnancy/pelvic-pain-during-early-pregnancy
- ↑ Wendy Powell. Maternal Health & Exercise Specialist. Expert Interview. 24 September 2020.
- ↑ https://www.merckmanuals.com/home/women-s-health-issues/symptoms-during-pregnancy/pelvic-pain-during-early-pregnancy
- ↑ Wendy Powell. Maternal Health & Exercise Specialist. Expert Interview. 24 September 2020.
- ↑ https://www.merckmanuals.com/home/women-s-health-issues/symptoms-during-pregnancy/pelvic-pain-during-early-pregnancy
- ↑ https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-pelvic-girdle-pain-and-pregnancy.pdf
- ↑ https://www.nhs.uk/conditions/pregnancy-and-baby/pelvic-pain-pregnant-spd/
- ↑ https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-pelvic-girdle-pain-and-pregnancy.pdf
- ↑ https://www.nhs.uk/conditions/pregnancy-and-baby/pelvic-pain-pregnant-spd/
- ↑ https://www.nhs.uk/conditions/pregnancy-and-baby/pelvic-pain-pregnant-spd/
- ↑ https://www.nhs.uk/conditions/pregnancy-and-baby/labour-signs-what-happens/
- ↑ https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-pelvic-girdle-pain-and-pregnancy.pdf












































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...