This article was medically reviewed by Eric Christensen, DPT. Eric Christensen is a Physical Therapist based in Chandler, Arizona. With over a decade of experience, Eric works in both orthopedic and neurological fields and specializes in custom orthotic prescription and casting, vestibular reprogramming, and manual therapy. He holds a Bachelor’s degree in Exercise Science with a focus in Sports Medicine from Colorado State University and a Doctor of Physical Therapy from Regis University. In practice, Eric takes a developmental approach to rehabilitation utilizing the Selective Functional Movement Assessment. He uses functional movement patterning and manual therapy to return patients to prior levels of function.
There are 13 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 87% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 175,626 times.
Studies show that severe osteoarthritis (the wear and tear type) is the most common cause for knee replacement surgery in the United States.[1] A total knee replacement is a type of surgery whereby a diseased knee joint is replaced with artificial material, such as titanium and plastic. Experts note that due to its exceptionally invasive nature, knee replacement surgery can generate substantial pain post-op, so learning how to manage it is very important.[2]
Steps
Managing the Pain at Home
-
1Rest and elevate your leg. Once you're discharged from the hospital, you'll be told to rest and elevate your leg for the first few days or so in order to help decrease swelling and inflammation, which also reduces pain.[3] While sitting on the sofa or a chair, prop your leg up with some pillows, but try not to hyperextend your knee and risk straining it — keep some flexion in the joint while resting. Consider putting a pillow under your knee at night while you sleep on your back to elevate the extremity.
- Total bed rest is not a good idea post-surgery because some movement (even in surrounding joints such as the hip and ankle) is needed to stimulate blood flow and healing.
- Wearing compression stockings can be another effective method for reducing achy pain and swelling, and preventing blood clot formation. Start wearing them day and night, then after a few weeks, switch to just while you sleep.
- There are two types of knee replacements: total knee replacements and partial knee replacements. Recovery from a total replacement takes longer — generally three to five days in the hospital and a recovery period lasting from one to three months.[4]
-
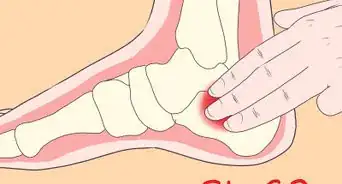
2Apply ice to your knee initially. While your knee is still in the acute phase (significant inflammation and pain), apply ice to it. The application of ice is an effective treatment for essentially all acute musculoskeletal injuries.[5] [6] Cold therapy should be applied to the area around the incision in order to reduce the swelling and pain, particularly in the muscles. Ice should be applied for 20 minutes every two to three hours for a couple of days, then reduce the frequency as the pain and swelling subside.
- Compressing the ice against your knee with a bandage or elastic support will also help control the inflammation, but don't tie it too tight because complete restriction of blood flow could cause more damage to your knee joint and lower leg.[7]
- Always wrap ice or frozen gel packs in a thin towel in order to prevent frostbite on your skin.
- If you don't have any ice or gel packs, then use a frozen bag of veggies from your freezer.
Advertisement -
3Use crutches to move around. For the first few weeks post-surgery, try to use your crutches (which are typically supplied by the hospital) while walking around so as to not inflame your knee. Some knee mobility after a few days post-op is a good idea, but total weight bearing while walking should be postponed for a week or two until the muscles surrounding the knee have started to heal and gain their back strength.[8]
- You should be able to resume most normal activities of daily living (including walking and bending) within 3-6 weeks following knee replacement surgery.
- Some pain with walking and other knee movements, particularly at night, is common for several weeks after you've had knee surgery.
- If your right knee was replaced, then don't try to drive a car until you're fully recovered, which may take a few months. Your orthopedist will clear you when it is safe for you to drive.
-
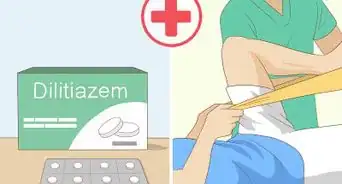
4Take your medications as advised. You'll likely receive pain medication (either orally or intravenously) while in the hospital and then given strong prescription drugs to take home.[9] These medications may include strong opioids, such as morphine, fentanyl or oxycodone, which may have to be taken for a few weeks.[10] Medication is an important part of managing your pain, so follow your doctor's instructions carefully and be aware that abuse of pain medications can lead to dependency.
- Alternatively, you may be given prescription-strength nonsteroidal anti-inflammatories (NSAIDs), such as ibuprofen or naproxen, or painkillers such as Tylenol #3. After a few weeks, you may be able to wean yourself to weaker over-the-counter offerings.
- Be careful not to take any medications on an empty stomach, as they can irritate the lining of your stomach and increase the risk of stomach ulcers.
- Pain-relieving creams containing capsaicin, menthol and/or salicylate may be of benefit also.
- Your doctor may also prescribe short-term antibiotics to reduce the risk of infection.
-
5Consider moist heat after the acute stage. After the inflammation and pain in and around your knee has largely subsided, then consider applying some moist heat. The application of heat causes mild dilatation of blood vessels and helps to alleviate any stiffness. Microwaved herbal bags work well and are often infused with aromatherapy (such as lavender) that has relaxing properties.
- With the permission of your doctor, soak your leg in a warm Epsom salt bath, which can significantly reduce pain and swelling, especially within muscles.[11] The magnesium in the salt helps the muscles relax.
- However, avoid soaking the wound in water until it has completely sealed and dried.
Seeking Medical Treatments
-
1Seek out physiotherapy. Physical therapy is an extremely important part of rehabbing after knee surgery and can begin as soon as 48 hours post-op.[12] after surgery. A physical therapist can show you specific and tailored stretches, mobilizations and strengthening exercises for your recuperating knee. Knee immobilizers are often used to stabilize the knee while undergoing physical therapy.
- Physiotherapy is usually required 2-3x per week for 6-8 weeks to positively impact a knee that's undergone surgery, although it may be longer.[13] [14] It will include a graduated walking program and knee-strengthening exercises.
- If need be, a physical therapist can stimulate, contract and strengthen your weakened leg muscles with electrotherapy, such as electronic muscle stimulation.
- For pain control, a physical therapist can use a TENS (transcutaneous electrical nerve stimulation) unit on your knee.
-
2Use a continuous passive motion machine. A device that can help speed knee recovery and reduce stiffness is the continuous passive motion (CPM) machine.[15] The CPM machine is attached to the recuperating leg and automatically moves the knee through various motions for up to an hour or so while the patient relaxes. This type of passive exercise can improve circulation and reduce the risk of scarring / contracture of the soft tissues surrounding the knee.
- CPM exercise machines also help to prevent blood clot formation in the legs.
- Some physical therapists, occupational therapists and physiotherapists (rehabilitation physicians) have CPM machines in their office, but not all of them.
-
3Consider infrared therapy. The use of low-energy light waves (infrared) is known to be able to speed up the healing of wounds, decrease pain and decrease inflammation.[16] Use of infrared radiation (either through a hand-held device or within a special sauna) is believed to penetrate deep into the body and improve circulation because it creates heat and dilates blood vessels.
- In most cases, significant pain reduction can start within hours after the first infrared treatment.
- Pain reduction is often long lasting, weeks or even months.
- Practitioners most likely to use infrared therapy include some chiropractors, osteopaths, physical therapists and massage therapists.
Using Alternative Treatments
-
1Try acupuncture treatments. Acupuncture involves sticking very thin needles into specific energy points within the skin / muscle in efforts to reduce pain and inflammation and to potentially stimulate healing.[17] Acupuncture is not commonly recommended for pain control post surgery and should only be considered as a secondary option, but anecdotal reports suggest it can be helpful for many different types of musculoskeletal injuries. It's worth a try if your budget allows for it.
- Based on the principles of traditional Chinese medicine, acupuncture reduces pain and inflammation by releasing a variety of substances including endorphins and serotonin.
- Acupuncture is practiced by a variety of health professionals including some physicians, chiropractors, naturopaths, physical therapists and massage therapists — whoever you choose should be certified by NCCAOM.
-
2Get a deep tissue massage. Knee replacement surgery involves cutting into the muscles surrounding the knee joint in order to clean it up and resurface the ends of the bones. As such, the muscles experience severe trauma, which leads to inflammation and spasm post surgery. A deep tissue massage is helpful starting a few weeks after surgery because it reduces muscle spasm, combats inflammation and promotes relaxation.[18] Start with a 30 minute leg massage, focusing on your thigh and hamstring muscles. Allow the therapist to go as deep as you can tolerate without wincing.
- Always drink lots of water immediately following a massage in order to flush out inflammatory by-products and lactic acid from your body. Failure to do so might cause a headache or mild nausea.
-
3Experiment with vibration therapy. An interesting alternative option in managing musculoskeletal pain is vibrational therapy. Vibrating frequencies seem to relax and strengthen musculature while stimulate nerves to reduce pain. In terms of knee pain, you can vibrate primarily the knee area or the entire body — both have proven effective for reducing knee pain.[19]
- Full-body vibrating machines are difficult to find in rehabilitation facilities and likely too expensive to buy for home use, so consider smaller machines that vibrate your feet and/or lower legs.
- A hand-held vibrating massage device is another option that may work well to stimulate and reduce pain in the muscles around your knee.
Expert Q&A
-
QuestionHow do you manage pain after ACL surgery?
 Eric Christensen, DPTEric Christensen is a Physical Therapist based in Chandler, Arizona. With over a decade of experience, Eric works in both orthopedic and neurological fields and specializes in custom orthotic prescription and casting, vestibular reprogramming, and manual therapy. He holds a Bachelor’s degree in Exercise Science with a focus in Sports Medicine from Colorado State University and a Doctor of Physical Therapy from Regis University. In practice, Eric takes a developmental approach to rehabilitation utilizing the Selective Functional Movement Assessment. He uses functional movement patterning and manual therapy to return patients to prior levels of function.
Eric Christensen, DPTEric Christensen is a Physical Therapist based in Chandler, Arizona. With over a decade of experience, Eric works in both orthopedic and neurological fields and specializes in custom orthotic prescription and casting, vestibular reprogramming, and manual therapy. He holds a Bachelor’s degree in Exercise Science with a focus in Sports Medicine from Colorado State University and a Doctor of Physical Therapy from Regis University. In practice, Eric takes a developmental approach to rehabilitation utilizing the Selective Functional Movement Assessment. He uses functional movement patterning and manual therapy to return patients to prior levels of function.
Physical Therapist Take your pain medication as prescribed. For a natural solution, ice and compression boots may help reduce swelling, which often is a source of pain.
Take your pain medication as prescribed. For a natural solution, ice and compression boots may help reduce swelling, which often is a source of pain. -
QuestionWhy does my knee still hurt after ACL surgery?
 Eric Christensen, DPTEric Christensen is a Physical Therapist based in Chandler, Arizona. With over a decade of experience, Eric works in both orthopedic and neurological fields and specializes in custom orthotic prescription and casting, vestibular reprogramming, and manual therapy. He holds a Bachelor’s degree in Exercise Science with a focus in Sports Medicine from Colorado State University and a Doctor of Physical Therapy from Regis University. In practice, Eric takes a developmental approach to rehabilitation utilizing the Selective Functional Movement Assessment. He uses functional movement patterning and manual therapy to return patients to prior levels of function.
Eric Christensen, DPTEric Christensen is a Physical Therapist based in Chandler, Arizona. With over a decade of experience, Eric works in both orthopedic and neurological fields and specializes in custom orthotic prescription and casting, vestibular reprogramming, and manual therapy. He holds a Bachelor’s degree in Exercise Science with a focus in Sports Medicine from Colorado State University and a Doctor of Physical Therapy from Regis University. In practice, Eric takes a developmental approach to rehabilitation utilizing the Selective Functional Movement Assessment. He uses functional movement patterning and manual therapy to return patients to prior levels of function.
Physical Therapist You may feel some pain because of the surgical incision. In this case, a bit of light motion and movement can help clear away some of that basic discomfort or nonspecific aching. Ultimately, time is going to be a huge factor, and you'll have to let the incision heal on its own.
You may feel some pain because of the surgical incision. In this case, a bit of light motion and movement can help clear away some of that basic discomfort or nonspecific aching. Ultimately, time is going to be a huge factor, and you'll have to let the incision heal on its own. -
QuestionIs it safe to cover a knee with cold cream, wrap it with a loose paper towel, and then wrap it with saran wrap to sleep for 8 hours before removing it?
 Jonas DeMuro, MDDr. DeMuro is a board certified Pediatric Critical Care Surgeon in New York. He received his MD from Stony Brook University School of Medicine in 1996. He completed his fellowship in Surgical Critical Care at North Shore-Long Island Jewish Health System and was a previous American College of Surgeons (ACS) Fellow.
Jonas DeMuro, MDDr. DeMuro is a board certified Pediatric Critical Care Surgeon in New York. He received his MD from Stony Brook University School of Medicine in 1996. He completed his fellowship in Surgical Critical Care at North Shore-Long Island Jewish Health System and was a previous American College of Surgeons (ACS) Fellow.
Board Certified Critical Care Surgeon Talk to your surgeon before applying anything to your incision after your operation. The wound should remain dry, and not covered with saran wrap unless approved by your surgeon.
Talk to your surgeon before applying anything to your incision after your operation. The wound should remain dry, and not covered with saran wrap unless approved by your surgeon.
Warning
- Contact your doctor immediately if you experience the following signs of infection: fever greater than 100°F (37.8°C), shaking chills, pus drainage from the incision, increasing redness, swelling and/or pain in the knee.[21]
References
- ↑ https://www.mayoclinic.org/tests-procedures/knee-replacement/about/pac-20385276
- ↑ https://www.mayoclinic.org/tests-procedures/knee-replacement/about/pac-20385276
- ↑ http://www.healthline.com/health/total-knee-replacement-surgery/managing-postoperative-pain#Medications3
- ↑ http://www.orthop.washington.edu/?q=patient-care/articles/knee/total-knee-replacement-a-patients-guide.html
- ↑ https://activeimplants.com/blog/6-dos-donts-knee-surgery/
- ↑ Eric Christensen, DPT. Physical Therapist. Expert Interview. 29 June 2021.
- ↑ Eric Christensen, DPT. Physical Therapist. Expert Interview. 29 June 2021.
- ↑ Eric Christensen, DPT. Physical Therapist. Expert Interview. 29 June 2021.
- ↑ Eric Christensen, DPT. Physical Therapist. Expert Interview. 29 June 2021.
- ↑ http://www.healthline.com/health/total-knee-replacement-surgery/managing-postoperative-pain#AftertheOperation2
- ↑ http://www.saltworks.us/salt_info/epsom-uses-benefits.asp
- ↑ http://www.medicinenet.com/total_knee_replacement/page4.htm#what_happens_in_the_postoperative_period_what_is_involved_in_the_recovery_from_surgery
- ↑ Eric Christensen, DPT. Physical Therapist. Expert Interview. 29 June 2021.
- ↑ http://www.orthop.washington.edu/?q=patient-care/articles/knee/total-knee-replacement-a-patients-guide.html
- ↑ http://www.medicinenet.com/total_knee_replacement/page4.htm#what_happens_in_the_postoperative_period_what_is_involved_in_the_recovery_from_surgery
- ↑ http://www.practicalpainmanagement.com/unique-use-near-infrared-light-source-treat-pain
- ↑ http://www.mayoclinic.org/tests-procedures/acupuncture/basics/definition/prc-20020778
- ↑ https://curearthritis.org/total-knee-replacement-good-bad-ugly/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3764345/
- ↑ http://www.orthop.washington.edu/?q=patient-care/articles/knee/total-knee-replacement-a-patients-guide.html
- ↑ http://www.mayoclinic.org/tests-procedures/knee-replacement/basics/risks/prc-20019202
About This Article
If you’ve just had knee replacement surgery, you can reduce pain and inflammation by resting and elevating your knee. It might also help to wear a compression stocking. During the first couple of days after the surgery, apply an ice pack to your knee every 2 to 3 hours for 20 minutes at a time. If you have to walk around, use crutches to minimize the weight on your knee. You can also keep pain in check by taking prescription or over-the-counter painkillers as recommended by your doctor. Once your doctor says it’s safe, try soaking in an Epsom salt bath. For more advice from our Medical co-author, including how to get medical treatments for your pain, read on!






































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...