This article was medically reviewed by Erik Kramer, DO, MPH. Dr. Erik Kramer is a Board-Certified Primary Care Physician at the University of Colorado. With over 15 years of experience, his clinical interests include obesity and weight management, diabetes care, and preventive care, as well as embracing a holistic approach to primary care. He received his Doctorate in Osteopathic Medicine (D.O.) from the Touro University Nevada College of Osteopathic Medicine and completed his residency at Central Maine Medical Center. Dr. Kramer is a Diplomate of the American Board of Obesity Medicine.
There are 12 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 7,963 times.
Osteopenia is when you have a bone density, also known as a T-score, of -1 to -2.5. Osteopenia may be a precursor of osteoporosis, which is when your bone density dips below -2.5. It’s important to treat osteopenia before it progresses since it puts you at an increased risk of breaking a hip, femur, or vertebra. Get a diagnosis from your doctor and discuss your treatment options. You can also try making lifestyle changes to reverse osteopenia.
Steps
Seeking Medical Treatment Options
-
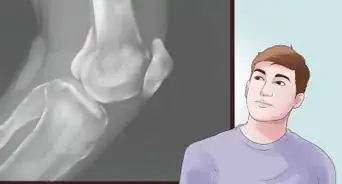
1Get a DXA test done to determine your risk of breaking a bone. Also known as dual-energy x-ray absorptiometry or DEXA, a DXA test measures the density of your bones. The test is painless and noninvasive. A machine scans your body while you lie still on a table.[1] The result of this type of test is called a T-score, and if you have osteopenia, the score will be between -1 and -2.5.[2]
- Your risk of bone fractures rises with a lower DXA score. For example, if you score a -1 on a DXA test, you have a 16% chance of fracturing a hip, or a 27% chance with a score of -2, or a 33% chance with a score of -2.5.
-
2Tell your doctor about any medications you currently take. Some medications are known to increase the risk of osteopenia, so it’s important to tell your doctor about any medications you are currently taking. They may recommend switching if the risk of worsening bone density outweighs the potential benefits of a medication. Some medications that may increase the risk of osteopenia include:[3]Advertisement
-
3Get checked for any underlying conditions that may cause osteopenia. Osteopenia may present as a side effect of another condition, so it’s important to rule out any underlying causes. If you have an underlying condition, treating it may help to reverse your osteopenia or at least prevent it from getting worse. Some conditions that may contribute to osteopenia include:[6]
- Cushing’s disease
- Diabetes mellitus
- Hypogonadism
- Acromegaly
- Chronic kidney disease
- Hyperparathyroidism
Tip: Be aware that your risk of osteopenia also rises during pregnancy, after menopause, and after the age of 65.
-
4Ask your doctor about medications if you are at a high risk of fracture. Your doctor may recommend starting medication if your risk of fracturing a hip over the next 10 years is greater than 3% or if your risk of fracturing another major bone is greater than 20%. You can determine your risk using the World Health Organization’s FRAX calculator: https://www.sheffield.ac.uk/FRAX/tool.aspx?country=9 Also, if you have a T-score of -2.5 or lower, then your doctor will likely suggest starting a medication to treat osteoporosis.[7]
- The most commonly prescribed medications for improving bone density are biophosphonates, such as alendronate, risedronate, ibandronate, and zoledronic acid.[8]
- If you are a post-menopausal woman, your doctor may also recommend estrogen replacement therapy to help treat osteopenia. However, this is no longer a first-line therapy since it may increase the risk of breast cancer, stroke, coronary heart disease, and venous thromboembolism.[9]
- Medications can help to get your T-score back up above -1 and avoid letting it fall further into the osteoporosis category, which includes anything below -2.5. Once it falls below -2.5, medication will likely be necessary to improve your bone density.
Making Lifestyle Changes
-
1Do weight-bearing exercises on most days of the week. Bearing weight by walking, jogging, doing aerobics, dancing, and doing other activities that require standing can help to boost your bone density. Go for a 30 minute walk on 5 days of the week for an easy way to get some weight bearing exercise, or do another activity that you enjoy. Adjust the amount of exercise that you do according to your fitness level.[10]
- For example, if walking for 30 minutes at a time is difficult for you, start by walking 10 minutes, and then increase the amount you walk each week by 5 minutes until you are walking for 30 minutes at a time.
- You can also break up your daily exercise into smaller sessions, such as by doing two 15-minute walks or three 10-minute walks.
-
2Get the recommended daily amount of calcium and vitamin D. Calcium and vitamin D deficiency are major causes of osteopenia, so it’s important to work these into your diet or take a supplement if you have trouble getting the recommended amount each day. [11] Most people need about 1,000 mg of calcium each day and 600 iu (15 micrograms) of vitamin D, but talk with your doctor before starting any supplements to find out what amount is right for you.[12]
- Good sources of calcium include milk, cheese, yogurt, leafy green vegetables, fish with soft, edible bones like sardines, and calcium fortified foods, such as orange juice and cereal.
- Good sources of vitamin D include cod liver oil, canned tuna, fortified orange juice, milk, yogurt, and eggs.[13]
-
3Quit smoking if you’re a smoker. Smoking increases your risk of developing osteopenia, so if you’re a smoker, quitting might help to improve your condition. Talk to your doctor about medications and nicotine replacement products that might help you quit. There may also be other resources in your area for people who want to stop smoking.[14]
- Buproprion and varenicline tartrate are prescription medications that may help you quit by reducing your cravings. You can also try nicotine replacement products, such as gum, lozenges, and patches to help with cravings.
- Many people also benefit from using counseling, support groups, and smart phone apps to help them quit.[15]
-
4Cut back or quit drinking if you drink alcohol regularly. Alcoholism is another common risk factor for osteopenia. If you drink alcohol heavily or on a daily basis, then cutting back or quitting may help to reverse your osteopenia. Talk to your doctor if you are having trouble cutting back or quitting. There are medications and programs that can help.[16]
- Moderate drinking is defined as no more than 1 drink per day for women or no more than 2 drinks per day for men. If you exceed this amount, then you may want to cut back or quit drinking.
-
5Gain weight if you’re underweight. Being underweight also predisposes you to osteopenia. If you have a body mass index of 18.5 or lower, then you’re considered underweight.[17] Talk to your doctor to determine a healthy weight for you.[18]
- Aim to gain weight slowly over time by adding more nutritious foods into your diet. For example, base your meals on starches, such as pasta, rice, or bread, and include a serving of vegetables, fruit, lean protein, and healthy fats with every meal.[19]
Tip: Being malnourished is a risk factor for developing osteopenia, so eat a wide variety of healthy foods every day.[20]
References
- ↑ https://www.nhs.uk/conditions/dexa-scan/what-happens/
- ↑ https://my.clevelandclinic.org/health/diseases/21855-osteopenia
- ↑ https://my.clevelandclinic.org/health/diseases/21855-osteopenia
- ↑ https://rad.washington.edu/about-us/academic-sections/musculoskeletal-radiology/teaching-materials/online-musculoskeletal-radiology-book/osteopenia/
- ↑ https://medlineplus.gov/ency/article/007231.htm
- ↑ https://rad.washington.edu/about-us/academic-sections/musculoskeletal-radiology/teaching-materials/online-musculoskeletal-radiology-book/osteopenia/
- ↑ https://www.health.harvard.edu/womens-health/osteopenia-when-you-have-weak-bones-but-not-osteoporosis
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK499878/
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/12117397
- ↑ https://familydoctor.org/condition/osteopenia/
- ↑ https://www.health.harvard.edu/womens-health/osteopenia-when-you-have-weak-bones-but-not-osteoporosis
- ↑ https://familydoctor.org/condition/osteopenia/
- ↑ https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK499878/
- ↑ https://www.cdc.gov/tobacco/data_statistics/fact_sheets/cessation/quitting/index.htm#ways
- ↑ https://www.health.harvard.edu/womens-health/osteopenia-when-you-have-weak-bones-but-not-osteoporosis
- ↑ https://www.cdc.gov/healthyweight/assessing/index.html
- ↑ https://www.health.harvard.edu/womens-health/osteopenia-when-you-have-weak-bones-but-not-osteoporosis
- ↑ https://www.nhs.uk/live-well/healthy-weight/advice-for-underweight-adults/
- ↑ https://rad.washington.edu/about-us/academic-sections/musculoskeletal-radiology/teaching-materials/online-musculoskeletal-radiology-book/osteopenia/





























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...