This article was co-authored by Padam Bhatia, MD. Dr. Padam Bhatia is a board certified Psychiatrist who runs Elevate Psychiatry, based in Miami, Florida. He specializes in treating patients with a combination of traditional medicine and evidence-based holistic therapies. He also specializes in electroconvulsive therapy (ECT), Transcranial Magnetic Stimulation (TMS), compassionate use, and complementary and alternative medicine (CAM). Dr. Bhatia is a diplomat of the American Board of Psychiatry and Neurology and a Fellow of the American Psychiatric Association (FAPA). He received an MD from Sidney Kimmel Medical College and has served as the chief resident in adult psychiatry at Zucker Hillside Hospital in New York.
There are 11 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 39,903 times.
You may feel like you’ve completed treatment and are successfully dealing with OCD. Then, you get triggered by something and everything falls apart, and you’re back to square one. You may feel like it’s impossible to recover from a relapse. However, there is hope to get back on track. While obsessive thoughts may not go away, it’s important to have a plan for dealing with them for when they do come up.
Steps
Dealing with Lapses and Relapse
-
1Address feelings of doubt and guilt. Doubt and guilt are considered the hallmarks of OCD. Doubts can arise about every situation, topic, event, or person and these doubts are often futile in resolving. Guilt can also play a major role in OCD. You may feel personally responsible for things that had nothing to do with you and constantly find yourself thinking, “If only….” Remind yourself that you are responsible for yourself, and you generally do the best you can. Especially after a relapse, you may feel many negative emotions. Don’t ignore the emotions, but don’t dwell on the feelings either, as they can contribute to OCD.[1]
- If you find yourself feeling doubtful (“Did I do everything I could? Am I really sane? Will I become a criminal? Can I really get to the other side of OCD?”), address these feelings. Say to yourself, “I have doubts about this situation. Is this coming from me or from OCD?” The same is true for guilt.
-
2Understand the difference between a lapse and a relapse. You may experience a period of time with no OCD triggers, then suddenly experience obsessions once again. After the obsessions re-emerge, you may feel a need to complete compulsive behaviors, and this is considered a lapse. A relapse, however, involves absolute or rigid thinking following the re-emergence of obsessions, such as, “All my therapy is wasted, I must now engage my obsessions and compulsions.” This type of rigid thinking is associated with a relapse.[2]
- For example, a person with contamination fears may be triggered by using a dirty public restroom and begin washing compulsions as a result of the distress. This is a lapse.
Advertisement -
3Plan for lapses. Anticipate what situations will trigger lapses or setbacks into obsessive thoughts or fears. If you know you will experience heightened distress (like you will be around many people and may begin to have a contamination fear), plan for intrusive thoughts. Recognize that the thoughts are a result of the stress and a part of OCD. Having intrusive thoughts is not a failure.
- Say to yourself, “I know this is a stressful situation, and that obsessive thoughts or fears may happen. Even if they do, it does not mean that I am failing.”
-
4Manage lapses. After you’ve identified a lapse, assess what made you lapse and how you can prevent future lapses. You may feel triggered at a number of situations, yet having a plan to deal with these triggers is most important. Think about what worked during treatment and try that on your own. When triggered, expose yourself to the fear, stop yourself from engaging in rituals, get through the anxiety, and repeat the process.[3]
- Say to yourself, “This is stressful, but I know I can handle this. This fear exposure can help me work past my anxieties and not need to perform a ritual.”[4]
-
5Expect recovery to be imperfect. Remind yourself that nobody is perfect and to not set too high a bar for yourself. You may forget medication here or there, or begin to give into obsessive thinking. Instead of beating yourself up or putting yourself down for getting off track, refocus your efforts to start again.[5]
- There’s no need to guilt or shame yourself. Forgive yourself and get back on track.
- If you have a rigid approach to treatment and success, it can backfire. Recognize that obsessions won’t go entirely away and you may experience triggers and fears.
Managing Symptoms Effectively
-
1Confront obsessions immediately. Typically, obsessions occur because you want to avoid a feared situation. Out of that avoidance comes compulsions. Relapse can happen as a result of avoiding an obsessive fear that got out of control and turned into performing compulsions to continue resisting the fear. It’s important to confront fears as they occur and deal with them appropriately as soon as possible.[6]
- For example, a fear of germs may occur. If not dealt with immediately, you may turn to hand washing or excessively cleaning the house as a way to deal with the fear. Confronting the fear may include you thinking, “I recognize that I’m having a fear of germs come up. I know that germs exist and that sometimes they make people sick. I do a good job of cleaning myself and my house, which makes me at a lower risk of contracting anything.”
-
2Expose yourself to anxiety triggers. The more exposure you have to the things that cause you anxiety, the better you will be able to handle those triggers. Resist or delay the compulsions that these triggers create.[7] More exposure means that your anxiety will decrease and fade. Then you will realize that you have less fear and more control than you did before.[8]
- For example, if you need your items to be symmetrical, begin to purposefully leave one thing out of row, then place it back 30 seconds later. Continue to do this over time and recognize that it causes less and less distress to be exposed to non-symmetry.
-
3Anticipate urges and thoughts. If you have specific compulsions or obsessions that occur frequently, begin to anticipate them and combat the urges they cause. If you continuously check that tasks have been performed (such as the doors are locked, the windows are shut, and the stove is turned off), make a mental picture of the task being completed. You can also say aloud, “I have closed the windows.”[9]
- If fears or obsessive thoughts begin to arise, take note and say to yourself, “This is an obsessive thought. I know I completed this task.”
-
4Distract yourself from obsessive thoughts. Obsessions are normal and can be expected when dealing with OCD.[10] Don’t fret about having obsessive thoughts and instead, devise a plan to push against them when they do come. For example, find a distracting activity you can do until the thought or urge passes. This can include taking a walk, reading a book, or listening to music.
- Recognize that having obsessive thoughts is nothing to be ashamed of, but it is important to plan for them and be prepared to deal with them.
-
5Live a balanced life. Focus on getting enough sleep, eating healthy foods, and exercising regularly. Spend time with friends and social relationships and try to balance your life in a way that does not cause excess stress. Balancing the basic aspects of your life can help you in your recovery and can minimize stress.[11]
- Having your external life balanced can help your internal life be more balanced and make each day more predictable.
Recovering Through Therapy and Social Support
-
1Talk with a therapist. If you’ve stopped seeing your therapist or you’ve never seen one, now is a good time to get into therapy. Tell your therapist that you struggle with OCD and relapsed recently. Work toward preventing future relapses by learning skills to manage and cope with OCD symptoms. Work with the therapist to identify specific triggers so that you can avoid additional problems in the future. [12]
- The best type of therapy is Cognitive Behaviour Therapy, which is also known as “Talk Therapy”. Other types of therapy to help out with your relapse of OCD include Exposure and Response Prevention (ERP), which is a type of CBT. ERP involves progressive exposure of the object or situation that is leading to the relapse, and how to best cope with your anxiety about the obsession.
-
2Reach out for social support. It’s okay to ask friends and family for help and support. Share your experience with someone who cares about you and is willing to listen and support you. Even when you would rather isolate yourself, make an effort to make plans with friends, spend time with family, and maintain an active social life.[13]
- By isolating yourself, you increase your risk of experiencing anxiety and OCD. Surround yourself with people who care about you.
-
3Join a support group. A support group is a great place to meet other people who struggle with anxiety and OCD symptoms. You can share your experiences, give and receive advice, share recommendations, gain a sense of community, and make new friends.[14] Consider joining a self-help group, support group, or group therapy for individuals struggling with anxiety and OCD.
- If you do not have a group near you in your community, join an online support group.
- For more information, check out How to Join an Anxiety Disorder Support Group.
-
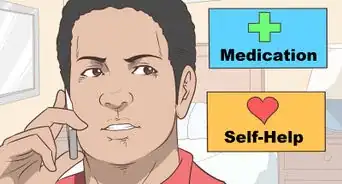
4Continue with treatment. You may relapse with OCD if you feel better and decide to stop taking your medications. You feel like you are “cured” or that your OCD was just a “phase.” Unfortunately, OCD is a chronic condition that must be treated and prevented. It is possible to manage OCD effectively, yet there is no “cure” for OCD.[15] OCD is often treated with a combination of therapy and medication.[16] Keep up with all treatment to stay on top of your symptoms and stay in control of your life.
- Medication approved by the FDA for the treatment of OCD are antidepressants.[17] These include the following medications: Clomipramine, Fluoxetine, Fluvoxamine, Paroxetine, and Sertraline.[18]
- Never stop antidepressant medication without the approval of your doctor because there are serious side effects that can result, which is sometimes called discontinuation syndrome.
- Medication is rarely effective by itself. It is most effective when combined with therapy.[19]
References
- ↑ http://beyondocd.org/expert-perspectives/articles/ten-things-you-need-to-know-to-overcome-ocd
- ↑ https://iocdf.org/expert-opinions/expert-opinion-relapse-prevention/
- ↑ https://iocdf.org/expert-opinions/expert-opinion-relapse-prevention/
- ↑ Padam Bhatia, MD. Board Certified Psychiatrist. Expert Interview. 3 April 2020.
- ↑ http://beyondocd.org/expert-perspectives/articles/ten-things-you-need-to-know-to-overcome-ocd
- ↑ http://beyondocd.org/expert-perspectives/articles/ten-things-you-need-to-know-to-overcome-ocd
- ↑ Padam Bhatia, MD. Board Certified Psychiatrist. Expert Interview. 3 April 2020.
- ↑ http://www.helpguide.org/articles/anxiety/obssessive-compulsive-disorder-ocd.htm
- ↑ http://www.helpguide.org/articles/anxiety/obssessive-compulsive-disorder-ocd.htm
- ↑ https://adaa.org/learn-from-us/from-the-experts/blog-posts/consumer/how-take-power-back-intrusive-thought-ocd
- ↑ http://beyondocd.org/expert-perspectives/articles/ten-things-you-need-to-know-to-overcome-ocd
- ↑ http://www.helpguide.org/articles/anxiety/anxiety-attacks-and-anxiety-disorders.htm#therapy
- ↑ https://www.mentalhealthfirstaid.org/2020/08/the-importance-of-having-a-support-system/
- ↑ https://iocdf.org/supportgroups/
- ↑ http://beyondocd.org/expert-perspectives/articles/ten-things-you-need-to-know-to-overcome-ocd
- ↑ http://www.camh.ca/en/hospital/health_information/a_z_mental_health_and_addiction_information/obsessive_compulsive_disorder/obsessive_compulsive_disorder_information_guide/Pages/ocd_medications.aspx
- ↑ Padam Bhatia, MD. Board Certified Psychiatrist. Expert Interview. 3 April 2020.
- ↑ http://www.mayoclinic.org/diseases-conditions/obsessive-compulsive-disorder/diagnosis-treatment/treatment/txc-20245962
- ↑ http://www.helpguide.org/articles/anxiety/obssessive-compulsive-disorder-ocd.htm#treatment


































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...