This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 10 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 88% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 272,690 times.
The development of a blood clot in your leg is also known as deep vein thrombosis (DVT). It is a serious condition that needs medical attention because the clot can break loose and travel to your lungs causing a pulmonary embolism (PE), which can be fatal. Pulmonary embolism can kill quickly if the embolus is large enough, with up to 90% of those affected dying within the first few hours. The presence of a small emboli is much more common and is successfully treated in the majority of cases. Although DVT may not exhibit any signs, by identifying the symptoms and getting proper medical attention, you can detect a blood clot in your leg.[1]
Steps
Identifying Symptoms of DVT
-
1Watch your leg for swelling. Because a clot can block blood flow in your leg, it may cause a backup of blood. Any lack of proper blood flow due to a clot may result in swelling in the affected leg.[2] Sometimes swelling alone may be the only presenting symptom of DVT.
- Be aware that the swelling will only generally be in one leg, though it can also be in an arm.
- Feel your leg with your hand gently and compare it to the other unaffected leg. The swelling may only be slight and not palpable by touch, but you may notice it when putting on articles of clothing such as pants, workout gear, or high boots.
- Make sure to look and feel along the veins of your leg for swelling as well.[3]
-
2Notice leg pain or tenderness. Many people with DVT also experience leg pain and tenderness. In many cases, they describe this as a feeling like a cramp or Charley horse in your leg.[4]
- Keep a log of when you notice leg pain or tenderness to rule out things like injury. Write down if the cramping or Charley horse comes on during or after exercise or if it happens when you’re just easily walking or sitting down. You may only feel the tenderness when you are standing or walking.[5] In many cases, pain will start in your calf and may radiate from there.[6]
Advertisement -
3Feel if your leg is warm. In some cases, your leg or arm may feel warm to the touch. When checking for other symptoms, may sure to lay your hands on each part of your leg to see if one section feels warmer than the others.[7]
- Be aware that the increased warmth may only be in the area that is swollen or causes pain; however, it’s a good idea to feel your entire leg so that you can more easily detect a section that is warm versus one without a temperature difference.[8]
-
4Look for discolored skin. The skin on a leg suffering from DVT may also exhibit discoloration. Looking for skin patches that are reddish or bluish in color may indicate that you have a blood clot in your leg.[9]
- Be aware that discoloration may look like bruising that doesn’t go away. Make sure to watch any discolored spots on your leg to see if they change colors or stay reddish or bluish. If they don’t change, it could signal a clot.
-
5Determine symptoms of PE. A blood clot in your leg may not have any visible or palpable signs;[10] however, if a whole or partial clot breaks off and enters your lung, you may have symptoms related to your breathing. If you have any of the following symptoms, seek immediate medical attention:[11]
- Sudden shortness of breath
- Sharp or stabbing pain when breathing that worsens with deep breaths
- Rapid heart rate
- Sudden bouts of coughing, which may have some blood or mucus
- Feeling lightheaded or dizzy[12]
- Fainting
- Feelings of dizziness or fainting
-
6Recognize your risk factors for developing DVT. Almost any person can develop a blood clot in his or her leg. There is a wide range of risk factors that may contribute to having DVT. You may be at higher risk for developing a blood clot in your leg if you have one or more of any of the following risk factors:[13] [14]
- Having surgery of any kind, but especially on the pelvis, abdomen, hip or knee
- Smoking
- Taking birth control pills
- A femoral (thigh) fracture
- Undergoing hormone replacement therapy
- Being on prolonged bed rest
- Being injured
- Being overweight or obese
- Being pregnant or giving birth
- Having cancer
- Suffering from inflammatory bowel disease
- Having heart failure or a heart attack
- Having a personal or family history
- You have had a stroke in the past
- Being over the age of 60
- Sitting for long periods of time, especially driving or flying
Getting a Medical Diagnosis
-
1Consult with your doctor. The only definitive way to know if you have a blood clot in your leg is to get a medical diagnosis. If you have any symptoms of a blood clot in your leg without the signs of PE, schedule an appointment with your healthcare provider as soon as possible. Make sure to let the office know why you’re calling so that they can schedule you without delay. Your health care provider will perform a full examination, run diagnostic tests, and prescribe or recommend the proper course of treatment based on your condition.[15]
- Answer any questions your doctor may have about your symptoms and when they started as well as what makes them better or worse. Make sure to let your doctor know about any medication you’re taking, if you’ve ever been treated for cancer, or if you’ve had any recent surgeries or injuries.[16]
-
2Undergo a physical exam. Before your doctor orders more involved tests, they will perform a physical exam to check for signs of DVT you may have overlooked. Your doctor will check your legs for the signs of DVT. In addition, your healthcare provider will measure your blood pressure and listen to your heart and lungs.[17]
- Let your doctor know if there is any part of the exam that causes you pain, such as if you experience pain when taking a deep breath while the doctor listens to your heart and lungs with a stethoscope.
-
3Get diagnostic tests. Your doctor may order additional tests to determine whether or not you have DVT or how serious your condition is. The most common diagnostic tests for DVT are:[18]
- Ultrasound, which is the most common test for DVT. It makes a picture of the veins and arteries in your leg so your doctor can better assess any clot.
- D-dimer test, which measures a substance in your blood that is released when a clot breaks up. High levels can indicate a deep vein blood clot.
- Spiral CT of chest or ventilation/perfusion (VQ) scan to rule out pulmonary embolism.
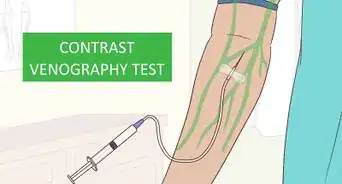
- Venography, which is done when an ultrasound doesn’t give your doctor a clear diagnosis. This procedure requires injecting a dye and then getting an x-ray that illuminates the vein. The x-ray can indicate if blood flow is slow, which may mean you have a deep vein clot.
- Magnetic resonance imaging (MRI) or computer tomography (CT) scans, which make pictures of the organs. These tests are not common for DVT, but more generally used for diagnosing PE.
Treating a Blood Clot in the Leg
-
1Take anticoagulants. If your doctor diagnoses you with DVT, they will aim to stop your blood clot from getting bigger, prevent it from breaking off and moving to the lungs, and reduce your chances of another clot. The most common way your doctor will do this is by prescribing anticoagulants, or blood thinners. These medications can be taken either as a pill, injection under the skin, or intravenously.[19] Patients with acute DVT require hospitalization for anticoagulation therapy.
- Make sure to ask any questions about the blood thinners you are taking. The two most common are warfarin and heparin. Initially you may be started with heparin then transition to warfarin. Warfarin is given in pill form and may have side effects such as headache, rash, and hair loss. Heparin comes in different forms — your doctor will discuss the best option for you. Heparin can also come with side effects such as bleeding, skin rash, headache, and upset stomach.[20]
- Be aware that your doctor may prescribe you Heparin and warfarin at the same time. They may also prescribe other injectable blood thinners such as enoxaparin (Lovenox), dalteparin (Fragmin) or fondaparinux (Arixtra).[21]
- Follow your doctor’s instructions for taking the medication exactly. Taking too much or too little of your medicine can have serious side effects. Follow up weekly for blood work or as recommended by your doctor.
-
2Have a filter inserted. Some people may not be able to take blood thinners or anticoagulants may not be effective at treating the clot. In these cases, your doctor may suggest inserting a filter into the vena cava, which is a large vein in your abdomen. The filter can prevent clots that have broken loose in your leg from lodging in your lungs.[22]
-
3Bust clots with thrombolytics. Severe cases of DVT may require medication called thrombolytics, which are also called clot busters. These medications dissolve the clot, which your body would otherwise do naturally in conjunction with other medications.[23]
- Recognize that thrombolytics run a high risk of causing bleeding, which is why they are reserved for severe or life-threatening cases.[24]
- Be aware that because of the severity, thrombolytics are only given in an intensive care unit of a hospital. A doctor will administer the drugs through an IV line or through a catheter that has been placed directly into the clot.
-
4Wear compression stockings. As a complement to any treatment for DVT, your doctor may prescribe wearing compression stockings. These can prevent swelling as well as blood from pooling and clotting in your legs.[25]
- Have your compression stocking fitted by your doctor or medical supply professional. Doing this can help ensure you get enough compression to be effective against clots. Buying a generic pair fitted for different body types may not be as effective as a pair specifically made for you.
- Wear your stockings for two to three years if possible.
-
5Have surgery. Thrombectomy is a type of surgery used to remove the clot from your leg. This procedure is used in rare cases, such as if your clot is especially severe, getting worse, or not responding to medication.[26]
Warnings
- Do not ignore blood clots, DVT, or PE symptoms, or delay meeting with your healthcare provider. You may need immediate treatment even if you don’t think your symptoms are severe. Failing to seek proper medical attention for a blood clot could result in worsened health or death.[27]⧼thumbs_response⧽
References
- ↑ http://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/basics/symptoms/con-20031922
- ↑ https://www.stoptheclot.org/learn_more/blood_clot_symptoms__dvt.htm
- ↑ https://www.nlm.nih.gov/medlineplus/magazine/issues/spring11/articles/spring11pg20-21.html
- ↑ https://www.stoptheclot.org/learn_more/blood_clot_symptoms__dvt.htm
- ↑ https://www.nlm.nih.gov/medlineplus/magazine/issues/spring11/articles/spring11pg20-21.html
- ↑ http://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/basics/symptoms/con-20031922
- ↑ https://www.stoptheclot.org/learn_more/blood_clot_symptoms__dvt.htm
- ↑ https://www.nlm.nih.gov/medlineplus/magazine/issues/spring11/articles/spring11pg20-21.html
- ↑ https://www.stoptheclot.org/learn_more/blood_clot_symptoms__dvt.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/basics/symptoms/con-20031922
- ↑ https://www.stoptheclot.org/learn_more/blood_clot_symptoms__dvt.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/basics/symptoms/con-20031922
- ↑ http://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/basics/risk-factors/con-20031922
- ↑ https://www.stoptheclot.org/know-your-risk.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/basics/symptoms/con-20031922
- ↑ https://www.nlm.nih.gov/medlineplus/magazine/issues/spring11/articles/spring11pg20-21.html
- ↑ https://www.nlm.nih.gov/medlineplus/magazine/issues/spring11/articles/spring11pg20-21.html
- ↑ https://www.nlm.nih.gov/medlineplus/magazine/issues/spring11/articles/spring11pg20-21.html
- ↑ https://www.nlm.nih.gov/medlineplus/magazine/issues/spring11/articles/spring11pg20-21.html
- ↑ https://www.stoptheclot.org/learn_more/blood_clot_treatment.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/basics/treatment/con-20031922
- ↑ http://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/basics/treatment/con-20031922
- ↑ http://www.cdc.gov/ncbddd/dvt/diagnosis-treatment.html
- ↑ http://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/basics/treatment/con-20031922
- ↑ http://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/basics/treatment/con-20031922
- ↑ http://www.cdc.gov/ncbddd/dvt/diagnosis-treatment.html
- ↑ https://www.stoptheclot.org/learn_more/blood_clot_symptoms__dvt.htm
About This Article
To detect a blood clot in your leg, watch out for swelling, which is caused by a blockage of blood flow. Additionally, pay attention to pain or tenderness in your leg, which may feel like a cramp. In some cases, one section of your leg may feel warmer than the others. You may also have discolored patches of skin, including reddish or blue patches. If you experience a sudden sharpness of breath, a sharp stabbing pain, or a rapid heart rate, seek medical attention immediately, since the clot may be impacting your lungs. For tips from our Medical co-author on how to get rid of a blood clot by taking anticoagulants, read on!
















-Step-13.webp)


-Step-16.webp)



















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...