This article was medically reviewed by Janice Litza, MD. Dr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
There are 13 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. This article has 23 testimonials from our readers, earning it our reader-approved status.
This article has been viewed 418,626 times.
Research suggests that for many patients, methadone -- a drug frequently used to wean patients off of opiates like heroin -- may need to be continued indefinitely in order to prevent relapses.[1] In this sense, it's helpful to think of methadone for heroin addicts as the equivalent of insulin for diabetics. Nevertheless, many patients do want or need to withdraw from methadone. If you're in that group, experts emphasize that it's absolutely crucial to consult your health care provider first and to wean yourself off the drug gradually to minimize any unpleasant side effects.[2]
Note: Any withdrawal program should be supervised by a suitably qualified professional. This article offers general guidance and is not a substitute for professional treatment.
Steps
Deciding to Quit Methadone
-
1Consider why you are quitting methadone. If you are taking methadone as a maintenance drug to aid in recovering from an opiate addiction, you are probably better off sticking with it. Methadone maintenance has no significant negative health effects, and patients who remain on methadone show gradual but steady improvements in health and functioning, while those who quit worsen in both aspects and have a much higher tendency to relapse into opiate use.[3]
-
2Speak with an addiction specialist. You will need both medical and psychological support to get off of methadone. It is important to note that not all doctors are able to prescribe withdrawal drugs like suboxone, because it requires a special training and approval from the government, such as the Drug Enforcement Administration (DEA) in the Unites States. Physicians with the proper training can tailor a withdrawal program to suit your needs and prescribe appropriate withdrawal drugs.Advertisement
-
3Set up a support network of friends and family. Quitting methadone is not easy. You will suffer withdrawal symptoms, and you will need to either carefully reduce your methadone intake over time or take medications regularly to substitute for methadone. Especially if you are quitting in an out-patient setting, it is extremely helpful to have friends and family who can hold you accountable and remind you to stay on course.
Getting off Methadone
-
1Do not try to quit “cold turkey.” The symptoms of methadone withdrawal are painful enough that quitting suddenly is simply not realistic. They typically begin within 30 hours of last methadone exposure and include:[4] [5]
- Early symptoms: agitation, anxiety, muscle aches, insomnia, runny nose, sweating, and yawning
- Late symptoms: abdominal cramping, diarrhea, dilated pupils, goose bumps, nausea, vomiting
-
2Be aware that quitting is a long-term process. Methadone withdrawal symptoms typically begin between 24 – 36 hours after the last dose and peak between 96 and 144 hours. While the detox process is usually considered over after five to seven days, milder symptoms may last for weeks, and “abstinence syndrome” — including unease, fatigue, insomnia, and irritability — can last for up to eight months.[6]
-
3
-
4Reduce methadone use gradually. There are two methods typically used: tapering the amount of methadone used or substituting buprenorphine and tapering or maintaining. Long-term maintenance with buprenorphine, accompanied by counseling and support groups, has been shown to produce the best rate of success.[8]
- Rapid detox programs using naltrexone to induce withdrawal can shorten peak withdrawal symptoms to two to three days, but there is no evidence regarding the rates of long-term abstinence for such programs.[9]
- Rapid detox under anesthesia should be avoided. It does not improve long-term results and carries a significant risk of death due to pulmonary edema (fluid in the lungs).[10]
- Maintenance on naltrexone is another option. It blocks the nerve receptors that opiates use, meaning that users of naltrexone will be unable to get high on opiates; however, relapse rates are very high for naltrexone treatments.
-
5Taper with methadone. There are two methods of tapering: a relatively quick method and a more recently prescribed long term method. In both cases, clonidine is often given to help reduce the symptoms of withdrawal.
- The more traditional tapering method usually takes five to seven weeks. Patients first rapidly reduce their use to 30 mg per day before beginning tapering at a typical rate of 5 mg per week.[11]
- Some clinics now recommend a more drawn-out tapering over six months to a year. The dose is reduced by 5 mg every three to 14 days, and then even more slowly after reaching 20 mg.[12]
-
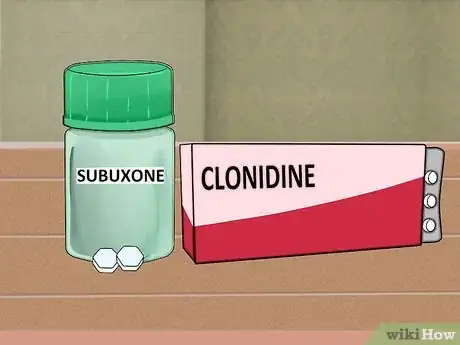
6Maintain or taper with buprenorphine-naxolone (Subuxone). Buprenorphine maintenance has been shown to be more effective than simply quitting methadone, while tapering with buprenoprhine is just as effective as tapering with methadone, and helps withdrawal symptoms to fade more quickly.[13] Patients must first reduce their methadone use to 40 mg/day for a week before beginning to substitute buprenorphine for methadone. Starting 36 hours after the last dose of methadone, the oral drug buprenorphine can be used to reduce symptoms of withdrawal.[14]
- Initial dose is 2 – 4 mg of buprenorphine. If that is tolerated, a second 2 – 4 mg does is given an hour later, and then 4 mg six to eight hours later, for a total day one dose of 8 –12 mg.
- A dose of 12 – 16 mg is reached by day two or three and should suppress most symptoms of withdrawal from methadone, with additional symptoms treated by clonidine.
- Once the patient's withdrawal symptoms are stabilized, buprenorphine can be continued as a long-term maintenance drug, or can be tapered off over two to three weeks.
- Once you have been weaned off methadone, your primary care provider may also be able to prescribe another form of buprenorphine (Butrans) which is available in patch or oral form.
Staying Off Methadone
-
1Get counseling. Your doctor or the clinic you are visiting will be able to put you in touch with an experienced opiate-withdrawal counselor. Whether it is one-on-one, group, or in a family setting, counseling in conjunction with buprenorphine maintenance or detox has been shown to be much more effective than maintenance or detox alone.[15]
-
2Join a support group. Support groups like Narcotics Anonymous or SMART Recovery can be extremely helpful for the recovering patient. One study found that recovering patients attending NA and AA programs had an 81% abstinence rate, compared to a 26% abstinence rate among non-attendees.[16]
- Don't force yourself to go through the pain of methadone withdrawal alone. There are thousands of other recovering patients just like you, who can not only give you advice and support, but who draw inspiration from you.
-
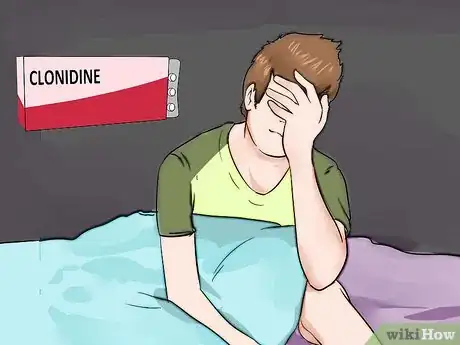
3Use clonidine or lofexidine to treat lingering withdrawal symptoms.[17] While clonidine is not as effective as buprenorphine during detox, it is useful in reducing lingering flu-like symptoms such as anxiety, agitation, muscle aches, sweating, runny nose, and cramping, all of which may last up to eight months. Lofexidine is a drug with a similar pathway, recently approved in the UK, which can reduce symptoms with fewer side effects.[18]
-
4Ask your doctor about using trazodone, zaleplon or zolpidem to treat insomnia. Insomnia is a common symptom of withdrawal from methadone. Zaleplon and zolpidem work like benzodiazepines such as clonazepam, but without the same withdrawal symptoms.[19] Trazodone is an antidepressant that regulates serotonin levels, thereby aiding sleep.[20]
-
5Treat the other lingering symptoms of withdrawal. Muscle cramps, diarrhea, nausea, and flu-like symptoms are most likely during detox, but such symptoms can linger for weeks. Aches and diarrhea can be treated with over-the-counter medications such as ibuprofen (Advil) and bismuth subsalicylate (Pepto-Bismol). Your doctor may prescribe prochlorperazine (Compazine) or ondansetron (Zofran) for nausea.[21]
Expert Q&A
-
QuestionWhat is the best way to wean myself off of Methadone?
 Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Board Certified Family Medicine Physician Work very closely with the prescribing clinic or physician and develop a plan and timeline so you know what to expect in the process.
Work very closely with the prescribing clinic or physician and develop a plan and timeline so you know what to expect in the process. -
QuestionWill temazepam help me to sleep? (I have not slept in 3 days now.)
 Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Board Certified Family Medicine Physician Yes. Temazepam is actually a benzodiazepine specifically prescribed for sleep. If you are having severe problems sleeping, I recommend talking to your doctor.
Yes. Temazepam is actually a benzodiazepine specifically prescribed for sleep. If you are having severe problems sleeping, I recommend talking to your doctor.
References
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1070723/
- ↑ https://www.nami.org/Learn-More/Treatment/Mental-Health-Medications/Types-of-Medication/Methadone%C2%AE
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202507/
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000949.htm
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1862300/?page=1
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202507/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1340840/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202507/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202507/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202507/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202507/
- ↑ http://www.camh.ca/en/hospital/health_information/a_z_mental_health_and_addiction_information/methadone/client_handbook/Pages/mmt_clienthndbk_ch8.aspx
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/12821205
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202507/
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/8385230
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1574294/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202507/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202507/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC181172/
- ↑ http://www.nlm.nih.gov/medlineplus/druginfo/meds/a681038.html
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202507/