This article was co-authored by Lydia Shedlofsky, DO. Dr. Lydia Shedlofsky is a Resident Dermatologist who joined Affiliated Dermatology in July of 2019 after completing a traditional rotating internship at Larkin Community Hospital in Miami, Florida. She earned a Bachelor of Science in Biology at Guilford College in Greensboro, North Carolina. After graduation, she moved to Beira, Mozambique, and worked as a research assistant and intern at a free clinic. She completed a Post-Baccalaureate program and subsequently earned a Master's Degree in Medical Education and a Doctorate of Osteopathic Medicine (DO) from the Lake Erie College of Osteopathic Medicine.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 41,416 times.
Ocular rosacea is a form of skin disease in and around the eye area that results in eye redness, swelling, burning, and itching.[1] It can sometimes even cause the sensation of having sand in your eyes. Ocular rosacea can be treated by a combination of prescription antibiotics and home eye care. There are several steps you can take in the midst of an ocular rosacea flare up to ease your symptoms and help it to pass, as well as some things you do to prevent flare-ups in the future. Ocular rosacea is a chronic, non-contagious condition that has no cure, but there are numerous ways to find relief.[2] Always consult your ophthalmologist or dermatologist to make sure any new treatment is right for you.
Steps
Treating Ocular Rosacea During a Flare Up
-
1Visit your doctor. If you believe you are experiencing ocular rosacea, it is best to consult your doctor.[3] Your eye doctor or general practitioner is the best person to diagnose and treat ocular rosacea. Severe or untreated problems can lead to scarring on the eyelid or corneal abrasions, both of which can impact your vision. That is why it is best to talk to a doctor when you first notice early symptoms. Common symptoms include:[4]
- Dry eyes
- Eye itchiness
- Feeling something gritty in your eyes
- Burning in the eyes
- Sensitivity to light
- Blurred vision
- Eye redness
- Swollen eyelids
- Watery eyes
-
2Use prescription oral antibiotics. Most of the time your doctor will prescribe antibiotics to help clear up and treat ocular rosacea.[5] You may be asked to take oral antibiotics for up to 1 month. Common medications include tetracycline, doxycycline, erythromycin, minocycline.[6]
- Your doctor may choose a particular drug based on your medical history and specific symptoms.
Advertisement -
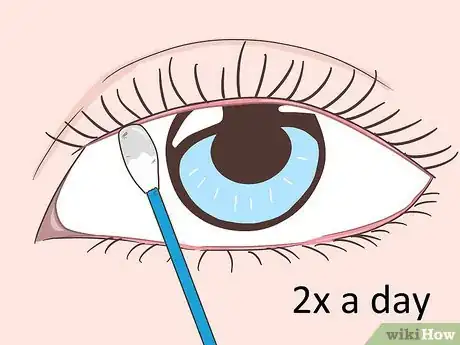
3Clean your eyelids twice a day. Dip a cotton swab in warm water and move it across your eyelid. Use it to remove any debris and/or oil from your eyelid. Repeat on the other eye, and complete this practice twice a day.[7]
- Your doctor may advise you to use very diluted baby shampoo to cleanse your eyelids instead of plain water.[8]
-
4Apply a warm compress to dilate blocked glands. Soak a clean washcloth in hot water. Wring out the washcloth, lie back, and place the washcloth over your closed eyes. Leave it there for 5-10 minutes. This should both loosen your blocked glands and help to soften any remaining debris.[9]
- You may want to clean your eyelids again if the warm compress loosens any excess oil or debris.
-
5Avoid makeup. In the midst of a flare up, it is best to avoid make up completely. Also avoid using facial care products that contain fragrances or other skin irritants. In most cases, you can resume using non-comedogenic makeup after your flare up is over.[10]
-
6Opt for glasses over contact lenses. While your eyes are irritated, it is best not to use contact lenses. Wear glasses instead, and give your eyes the opportunity to heal. In most cases, you will be able to resume the use of contact lenses after your flare up has passed.[11]
-
7
Preventing Future Flare Ups
-
1Recognize that this condition is chronic. Although ocular rosacea can usually be controlled with medication and other remedies, these actions don't actually cure the condition. Ocular rosacea is considered chronic and recurring, although many people experience periods of remission.[14]
-
2Continue to practice eyelid hygiene. You can help to prevent flare ups of ocular rosacea by continuing to wash your eyelids 1-2 times per day, even when you are not exhibiting rosacea symptoms. Try making this a regular part of your grooming routine.[15]
-
3Avoid hot, spicy foods. Ocular rosacea can be brought on by different triggers for different people. For some people, eating hot, spicy foods can signal a flare up. If this is true for you, avoid eating these foods.[16]
-
4Limit alcoholic beverages. Another potential rosacea trigger is alcohol. If you find that you are prone to rosacea flare-ups after consuming alcohol, you should probably avoid it. Try limiting yourself to 1-2 drinks per week.[17]
-
5Use only non-comedogenic and fragrance-free products. When you are not experiencing a flare up, it is probably safe to use makeup and other cosmetics. However, it is important to make sure that the products you use are fragrance-free and non-comedogenic.[18]
- Look for labels on cosmetic products that read fragrance-free and non-comedogenic.
- Shop at health foods store and specialty cosmetic stores to find special products.
-
6Limit your sun exposure. Sun exposure is another common rosacea trigger. Use a sunhat, wear sunglasses, and apply sunscreen any time you'll be out in the sun. Limit the amount of time you spend in direct sunlight. Never use tanning beds.[19]
-
7Consume flaxseed oil regularly. Some research indicates that consuming flaxseed oil, which is rich in omega-3 fatty acids, can help reduce flare-ups of rosacea. Look for flaxseed oil, flaxseed supplement capsules, or whole flaxseed at grocery stores and health food stores.[20]
- Try to consume about 2–3 teaspoons (9.9–14.8 ml) of flaxseed oil or 0.125 cups (30 ml) of ground flaxseed each day.
Expert Q&A
Did you know you can get expert answers for this article?
Unlock expert answers by supporting wikiHow
-
QuestionHow can I get relief from ocular rosacea?
 Lydia Shedlofsky, DODr. Lydia Shedlofsky is a Resident Dermatologist who joined Affiliated Dermatology in July of 2019 after completing a traditional rotating internship at Larkin Community Hospital in Miami, Florida. She earned a Bachelor of Science in Biology at Guilford College in Greensboro, North Carolina. After graduation, she moved to Beira, Mozambique, and worked as a research assistant and intern at a free clinic. She completed a Post-Baccalaureate program and subsequently earned a Master's Degree in Medical Education and a Doctorate of Osteopathic Medicine (DO) from the Lake Erie College of Osteopathic Medicine.
Lydia Shedlofsky, DODr. Lydia Shedlofsky is a Resident Dermatologist who joined Affiliated Dermatology in July of 2019 after completing a traditional rotating internship at Larkin Community Hospital in Miami, Florida. She earned a Bachelor of Science in Biology at Guilford College in Greensboro, North Carolina. After graduation, she moved to Beira, Mozambique, and worked as a research assistant and intern at a free clinic. She completed a Post-Baccalaureate program and subsequently earned a Master's Degree in Medical Education and a Doctorate of Osteopathic Medicine (DO) from the Lake Erie College of Osteopathic Medicine.
Dermatologist
References
- ↑ Lydia Shedlofsky, DO. Dermatologist. Expert Interview. 11 November 2020.
- ↑ https://my.clevelandclinic.org/health/diseases/22265-ocular-rosacea
- ↑ Lydia Shedlofsky, DO. Dermatologist. Expert Interview. 11 November 2020.
- ↑ https://www.aao.org/eye-health/diseases/ocular-rosacea-facts
- ↑ Lydia Shedlofsky, DO. Dermatologist. Expert Interview. 11 November 2020.
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4458660/
- ↑ https://dermnetnz.org/topics/ocular-rosacea
- ↑ Lydia Shedlofsky, DO. Dermatologist. Expert Interview. 11 November 2020.
- ↑ https://dermnetnz.org/topics/ocular-rosacea
- ↑ https://www.aad.org/public/diseases/rosacea/triggers/prevent
- ↑ https://emedicine.medscape.com/article/1197341-treatment
- ↑ Lydia Shedlofsky, DO. Dermatologist. Expert Interview. 11 November 2020.
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5096126/
- ↑ https://my.clevelandclinic.org/health/diseases/22265-ocular-rosacea
- ↑ https://www.rdehospital.nhs.uk/media/5uqizssz/patient-information-leaflet-eyelid-hygiene-rde-18-243-001.pdf
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5096126/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5096126/
- ↑ https://www.aad.org/public/diseases/rosacea/triggers/prevent
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5096126/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2646454/






































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...