This article was co-authored by Shervin Eshaghian, MD. Dr. Shervin Eshaghian is a Board Certified cardiologist and the owner of Beverly Hills Cardiology based in the Los Angeles, California metro area. Dr. Eshaghian has over 13 years of cardiology experience, including serving on the medical staff at Cedars-Sinai Medical Center. He holds a BS in Psycho-Biology from the University of California, Los Angeles (UCLA) and an MD from the Albert Einstein College of Medicine. Furthermore, Dr. Eshaghian completed an internship, residency, and fellowship at Cedars Sinai Medical Center, where he was awarded the Leo Rigler Outstanding Academic Achievement Award and the Elliot Corday Fellow of the Year Award.
There are 21 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 22,306 times.
Myocarditis, or inflammation of the heart muscle, is uncommon, but can be life-threatening if left untreated. While it’s usually caused by an infection, it also can occur in people who suffer from autoimmune disorders.[1] Getting an accurate diagnosis is vital, as treatments for autoimmune-related myocarditis can interfere with the body’s ability to fight an infection. In addition to treating the underlying cause, your doctor will give you medication to help your heart function normally. You’ll likely need to take medications, avoid strenuous activity, and limit your salt intake for at least 6 months.
Steps
Diagnosing the Cause of Myocarditis
-
1See your doctor if you experience shortness of breath or chest pain. While many people don’t experience symptoms, signs of myocarditis may include unexplained shortness of breath, chest pain or pressure, joint pain, fatigue, and rapid or irregular heartbeat. These symptoms could be related to a variety of conditions, so see a doctor for an accurate diagnosis.[2]
- You can see your primary doctor for an initial exam, and they'll most likely refer you to a cardiologist if they find signs of a heart problem. If they determine your condition is urgent, they'll instruct you to go to the emergency room.
- Call emergency services if you can’t breathe or experience severe chest pain with pain or tingling in your arms, neck, or jaw.
- Myocarditis is more likely if you’ve had an infection such as the flu or if you have an autoimmune disorder, such as rheumatoid arthritis or lupus.[3]
-
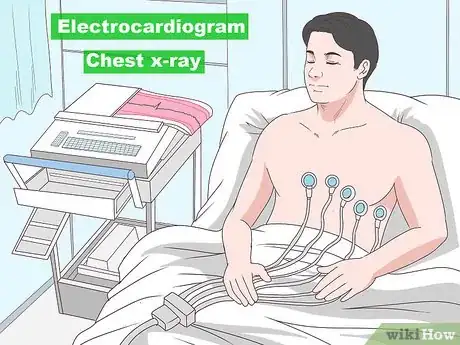
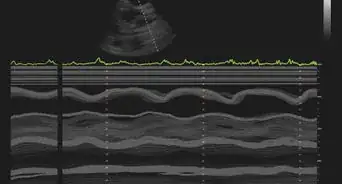
2Get an electrocardiogram (EKG or ECG) and chest x-ray. First, your doctor will perform a physical exam and listen to your heart with a stethoscope. If they suspect something’s wrong, they’ll take an ECG to check for abnormal heart rhythms. They may also order an x-ray to examine the size and shape of your heart.[4]
- If your doctor has the necessary equipment in their office, you might undergo these screenings and get results the day of your initial visit. If not, they might have you schedule appointments with another facility. If your condition is urgent, they'll advise you visit the emergency room.
- Your doctor might also order other imaging tests, such as a cardiac MRI, which can show the size, shape, and structure of your heart. An MRI can reveal signs of inflammation in the heart muscle.
- An echocardiogram is a graph of the sound waves produced by your heartbeat. An ECG can reveal heart valve problems, pumping irregularities, or other issues, such as clots or excessive fluid in the heart.
Advertisement -
3Have your blood tested for signs of an infection. If your doctor suspects something's wrong, they'll test your blood for viral antibodies, bacteria, and fungi. They’ll also check your blood for substances related to an autoimmune response.[5]
- The most common cause of myocarditis is a viral infection.
- An autoimmune response is when the body attacks itself in order to fight an infection or because of an autoimmune disorder.
-
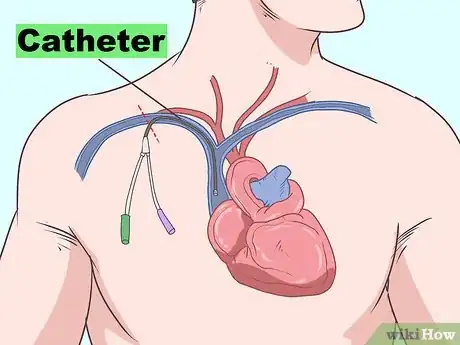
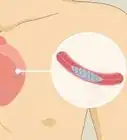
4Get an endomyocardial biopsy, if your doctor recommends it. Your doctor may wish to perform an endomyocardial biopsy to check for infection or inflammation in your heart. The doctor will insert a thin tube (catheter) through a vein in your leg or neck and into your heart. They will then thread a tiny surgical tool through the tube to collect a small sample of tissue from your heart for lab analysis.[6]
- This type of biopsy can help establish an accurate diagnosis, which is required to avoid administering potentially dangerous treatments. For example, steroids are used to treat autoimmune responses, but they weaken the immune system. This could be dangerous if you have a viral infection.
- An endomyocardial biopsy is performed at a hospital. You’ll receive a sedative and local anesthetic, but you need to be awake during the procedure. You might experience some pressure and discomfort at the incision site.[7]
Treating the Underlying Cause
-
1Consult your doctor about treatments for a viral infection. Your doctor may only recommend medications to support your immune system and heart function if you have an acute, or short-term, infection. If you’ve had a viral infection for more than 6 months, they might recommend antiviral drugs, such as interferon or ribavirin.[8]
- You’ll likely inject your medication every other day. Use any medication according to your doctor’s instructions. You might need to continue antiviral treatments for up to 6 months. Common side effects include flu-like symptoms, muscle tightness, and weakness.
- Seek medical attention if you experience serious side effects, such as bruising or discoloration at the injection site, nausea, vomiting, confusion, trouble speaking, swelling, increased aggression, or yellowing of the skin or eyes.[9]
-
2Take antibiotics as directed if you have a bacterial infection. If you have a bacterial infection, your doctor will prescribe an antibiotic, which you’ll most likely take orally. Take antibiotics as prescribed, and don’t stop taking your medication without your doctor’s approval.[10]
- If you stop taking antibiotics prematurely, the infection could return or worsen.
- You might also receive antibiotics intravenously (IV).
-
3Treat myocarditis related to an autoimmune disorder with steroids. Steroids, such as methylprednisone, reduce inflammation caused by an autoimmune response. If necessary, you’ll most likely take a steroid orally for 6 months. Your doctor will prescribe a dosage amount and schedule. Take your medication as directed, and don’t stop taking it without their approval.[11]
- Common side effects include upset stomach, vomiting, headache, dizziness, restlessness, acne, and insomnia. Seek medical attention if you experience a rash, swelling, vision problems, or muscle weakness.
- These medications are immunosuppressants, which means they can interfere with your body’s ability to fight an infection. In cases of myocarditis related to viral infection, using an immunosuppressant without first controlling the infection can be fatal.[12]
- Avoid contact with sick people, wash your hands frequently, and don’t get any vaccines while taking an immunosuppressant. Call your doctor if you experience signs of an illness, such as coughing or sneezing, or suffer an injury.[13]
Supporting Normal Heart Function
-
1Take an ACE inhibitor as directed to promote blood flow. An ACE inhibitor is an oral medication that relaxes the blood vessels in your heart, which makes it easier for your heart to pump blood. Take your medication as directed, and don’t stop taking it without talking to your doctor. For most ACE inhibitors, take your dose at the same time every day an hour before a meal.[14]
- Many people who experience myocarditis take an ACE inhibitor or other heart medication for at least 3 months. You might need to continue taking an ACE inhibitor indefinitely if your heart sustained irreversible damage.[15]
- Side effects may include dizziness, headache, fatigue, loss of appetite, diarrhea, numbness, and joint pain. Call your doctor if you experience these side effects, and seek emergency care if you experience swelling of the tongue or lips.
-
2Take medications for an abnormal heart rhythm, if necessary. If you’re hospitalized for myocarditis and have an abnormal heart rhythm, your healthcare providers will likely administer an antiarrhythmic drug via IV. You might also need to take a long-term oral medication to manage an abnormal heartbeat.[16]
- There are a variety of drugs used to treat arrhythmia, or an abnormal heart rhythm. Your doctor will prescribe a specific drug, dosage amount, and schedule for your needs. Take your medication as instructed, and don’t stop taking it without consulting your doctor.
- You might also be prescribed a beta blocker, which lowers blood pressure, slows the heart’s rhythm, and is sometimes used to manage an irregular heartbeat.[17]
- Antiarrhythmic drugs and beta blockers can cause dizziness, headache, fatigue, and cold hands and feet.
-
3Relieve fluid retention with a diuretic. Diuretics, or fluid pills, remove excess water and sodium from your body, which build up due to heart failure and can cause widespread swelling. Take a diuretic orally 1 to 2 times per day according to your doctor’s instructions.[18]
- Avoid taking a diuretic right before going to bed, or you will need to get up repeatedly during the night to urinate. If you need to take a dose late in the day, try to take it in the early evening.
- Side effects may include increased urination, diarrhea, loss of appetite, and headache.
- Your doctor will tell you to reduce your salt intake. If you are taking a potassium sparing diuretic, you will also need avoid potassium-rich foods such as potatoes, apricots, peaches, tomatoes, brussels sprouts, nuts, dried beans, peas, spinach, bananas, prunes, raisins, oranges, and orange juice.[19]
-
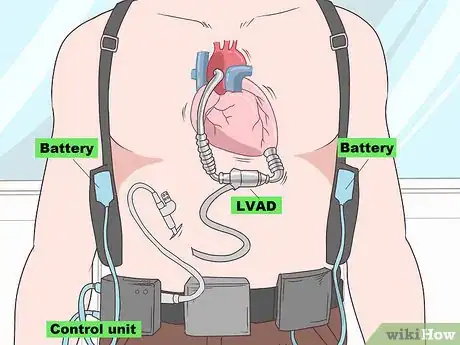
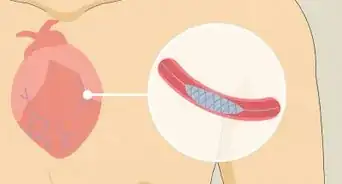
4Support blood flow with a mechanical pump in extreme cases. In severe cases of myocarditis, the heart becomes too weak to pump blood. Aggressive treatments, such as a ventricular assist device (VAD), an aortic balloon pump, or an oxygenation machine, might be needed to take over the heart’s function. In the most extreme cases of myocarditis, a heart transplant might be necessary.[20]
- Machines that pump or oxygenate blood are used until the heart recovers or until a new heart becomes available for transplantation.
Recovering from Myocarditis
-
1Avoid strenuous activity for 3 to 6 months. While your heart recovers, avoid intense aerobic exercise, heavy lifting, and other activities that cause your heart to beat faster. Consult your doctor about when you should begin resuming aerobic or strenuous activities.[21]
- The amount of time depends on the severity of your condition.
-
2Eat a heart-healthy, low-salt diet. The key elements of a heart-healthy diet are vegetables, fruits, whole grains, fat-free dairy products, and lean protein sources. Avoid foods that contain saturated and trans fats, salt, and added sugars. Limit your daily salt intake to 1500 to 2000 mg, or to the amount recommended by your doctor.[22]
- Foods to avoid include processed meats (such as bacon or deli meats), chips, fries, pastries, ice cream, and sweetened beverages, such as soft drinks. Processed foods tend to be high in sodium, calories, and refined sugars.
- Try to limit your intake of red meat, as well.[23]
- When you cook, use herbs and citrus instead of salt, and don’t add extra salt when you eat your meals. Try special salt-free spice blends, such as Mrs. Dash, to add flavor to your meals.
-
3Quit smoking and limit your alcohol consumption, if necessary. Alcohol can interfere with medications you take to treat myocarditis or cause undesirable side effects, such as dizziness or nausea. It also raises your blood pressure and can worsen heart failure. Smoking damages your heart and circulatory system and is harmful for your overall health, so ask your doctor for advice about quitting, if necessary.[24]
- You should also quit using any other tobacco products, as well.[25]
- Your doctor may tell you to stop drinking while your heart recovers or indefinitely if you’ve sustained permanent heart damage. At a minimum, you should drink no more than the recommended amounts, which are 2 drinks per day for men and 1 drink per day for women.[26]
-
4Take medications for chronic heart failure, if necessary. Many people who experience myocarditis recover fully without complications. However, if you’ve sustained irreversible heart damage, you might need to take long-term medications, such as an ACE inhibitor, a beta blocker, an antiarrhythmic drug, or a diuretic. Take any medication as prescribed and never stop taking medication for your heart without consulting your doctor.[27]
- See your doctor for routine check-ups and call them if you experience new or worsening side effects, such as chest pain, shortness of breath, or fainting.
References
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/myocarditis
- ↑ https://medlineplus.gov/ency/article/000149.htm
- ↑ https://my.clevelandclinic.org/health/diseases/22129-myocarditis
- ↑ https://www.myocarditisfoundation.org/about-myocarditis/
- ↑ https://rarediseases.org/rare-diseases/myocarditis/
- ↑ https://www.thecardiologyadvisor.com/cardiology/endomyocardial-biopsy/article/583479/
- ↑ https://medlineplus.gov/ency/article/003873.htm
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3370379/
- ↑ https://medlineplus.gov/druginfo/meds/a601151.html
- ↑ https://medlineplus.gov/ency/article/000149.htm
- ↑ http://circ.ahajournals.org/content/107/6/857.long
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3370379/
- ↑ https://medlineplus.gov/druginfo/meds/a682795.html
- ↑ https://medlineplus.gov/ency/patientinstructions/000087.htm
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3370379/
- ↑ http://www.heart.org/HEARTORG/Conditions/Arrhythmia/PreventionTreatmentofArrhythmia/Medications-for-Arrhythmia_UCM_301990_Article.jsp#.WqvedOjwaCg
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4042333/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3370379/
- ↑ https://medlineplus.gov/druginfo/meds/a682571.html
- ↑ https://medlineplus.gov/ency/article/007307.htm
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2770911
- ↑ https://www.nhlbi.nih.gov/node/24044
- ↑ Shervin Eshaghian, MD. Board Certified Cardiologist. Expert Interview. 26 June 2020.
- ↑ https://www.myocarditisfoundation.org/about-myocarditis/
- ↑ Shervin Eshaghian, MD. Board Certified Cardiologist. Expert Interview. 26 June 2020.
- ↑ https://www.cdc.gov/alcohol/fact-sheets/moderate-drinking.htm
- ↑ https://www.heart.org/en/health-topics/heart-failure/treatment-options-for-heart-failure/medications-used-to-treat-heart-failure

































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...