This article was co-authored by Asmi Sanghvi, DO and by wikiHow staff writer, Jennifer Mueller, JD. Dr. Asmi Sanghvi is a Board Certified Dermatologist based in New York, New York. She specializes in general and cosmetic dermatology and has a passion for educating others. Dr. Sanghvi has been published in several peer-reviewed journals, including the Journal of the American Academy of Dermatology and Cutis. She holds a BS in Human Communication Sciences from Northwestern University and a DO from Lake Erie College of Osteopathic Medicine.
There are 9 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 11,178 times.
An acne breakout on your back can be cause for insecurity and embarrassment. If it's fungal acne, you won't get any results if you treat it like regular acne. In fact, fungal acne can persist for years unless you use an antifungal medication to kill the fungus that's causing the acne. Luckily, most breakouts clear up simply by using creams that you can get online or at your local pharmacy or supermarket. Lifestyle changes, primarily focused on keeping the affected area clean and dry, improve the effectiveness of treatments. If your condition doesn't improve after treating it at home, a dermatologist can help you.[1]
Steps
Using Topical Treatments
-
1Try a shampoo with selenium sulfide as a body wash. Dandruff shampoos with selenium sulfide, such as Selsun Blue, can help clear up fungal acne. Instead of using the shampoo as you would a normal body wash, smear a thin layer of the shampoo over the affected area and leave it there for 5 to 10 minutes, then wash it off. Do this once a day until your skin is clear, then continue to do it once or twice a week to keep the fungal acne from returning.[2]
- Other dandruff shampoos, such as Head and Shoulders, with the active ingredient pyrithione zinc, might also work when used in the same way.
-
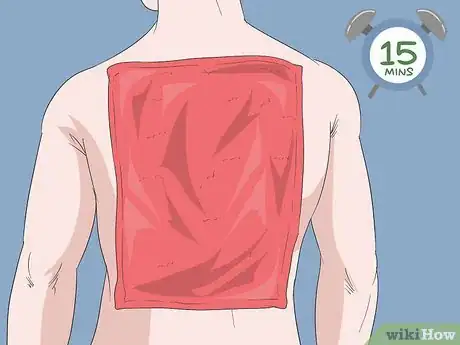
2Use a warm compress to calm itching and inflammation. It's not uncommon for fungal acne to itch, but you shouldn't scratch the bumps. A warm compress can help this so you don't feel the need to scratch. Simply soak a washcloth or hand towel in warm water, wring out the excess, and place it on the affected area.[3]
- Leave the warm compress on your skin for no more than 10-15 minutes at a time. Make sure you thoroughly dry your skin when you're done using the compress.
Advertisement -
3Add an over-the-counter antifungal cream. Antifungal creams with clotrimazole, such as Lotrimin, gradually kill the fungus that causes your fungal acne.[4] Read the instructions on the box carefully before applying the cream. Generally, you should see results if you apply the cream twice a day for a couple of weeks.[5]
- You can buy antifungal creams online or in your local pharmacy or supermarket. Since these creams are primarily marketed for treatment of athlete's foot, you'll likely find them with foot care products.
- Wash and dry the affected area with mild soap and warm water before applying antifungal cream with clotrimazole. Wash your hands both before and after applying it.[6]
Adjusting Your Lifestyle
-
1Shower immediately after exercising. Any time you work up a sweat, whether out on a run, at the gym, or just doing some work in your garden, take off your sweaty clothes and shower. Wash your skin thoroughly with a mild soap and warm water.[7]
- Bathe or shower at least once a day regardless of your activity level.
-
2Use your own towels and washcloths. Don't share towels or washcloths with anyone else if you have fungal acne. Not only can you spread the fungus to others but it's also possible that they can spread it to you.[8]
- Also avoid re-using towels and washcloths, even if they've completely dried between uses. Use a fresh, clean towel to dry off every time you take a shower.
-
3Wear looser clothes that don't rub against your skin. Tight-fitting clothes that rub against your skin trap heat and sweat, which can encourage fungal acne to spread. Wear light, breathable layers, especially when in you're going to be active or in a hot and humid environment.[9]
- If you have a dress code that requires a top that irritates the fungal acne on your back, try wearing a soft t-shirt underneath to help protect it.
- If you anticipate that you're going to get sweaty and won't have the opportunity to shower, bring a clean, dry shirt that you can change into.
- If you wear a bra and the straps rub against the inflamed area, try going without a bra or look for a bra in a different style that won't irritate your skin as much — at least until the fungal acne has cleared.
-
4Avoid using a public hot tub or spa. Hot tubs and spas can cause fungal acne on your back, as well as on your chest, arms, and legs. If you already have fungal acne, hot tubs can encourage it to spread.[10]
- If you have your own hot tub at home, thoroughly clean it according to the manufacturer's instructions. Don't use it while you have an outbreak of fungal acne to avoid contaminating it.
-
5Keep oils and oil-based products off your skin. While you certainly don't want to get sunburned, make sure any sunscreen you put on your back isn't oil-based. The oil will clog your pores and make it more difficult for you to eliminate the fungal acne.[11]
- Check the ingredients on any lotions or moisturizers you use regularly to make sure they don't include oils. If you feel the need to moisturize your skin, stick to natural, water-based moisturizers while you're treating the fungal acne.
Seeing a Dermatologist
-
1Schedule an appointment if symptoms persist over 3 weeks. With topical treatments for fungal acne, you'll likely see results in 2 to 3 weeks. However, if your acne isn't responding to the treatment or seems to be getting worse, have a dermatologist look at it.[12]
- Be prepared to tell the dermatologist how long you've had fungal acne, if you've ever had it before, and what you've done to treat and care for it.
- If there are any products or treatments you might be allergic to, be sure to let the dermatologist know. You'll also need to tell them about all medications and supplements you're taking so they can make sure they don't prescribe anything that would cause a bad interaction.
-
2Take prescribed antifungal medication as instructed. Most fungal acne clears up with over-the-counter topical treatment. However, if yours is resistant, your dermatologist might prescribe an oral antifungal medication.[13] These medications destroy the fungus that a topical cream might not be able to reach.[14]
- Always take the full round of medication, even if your skin starts to clear up before you've finished it. Completing the full round makes it less likely that the fungus will return.
- Make sure you understand the possible side effects of oral antifungal medication before you start. If you have troubling side effects, including nausea, vomiting, diarrhea, or abdominal pain, let your dermatologist know. They might discontinue treatment.[15]
-
3Try photodynamic therapy if oral medication doesn't work. With photodynamic therapy, the dermatologist applies a cream to your fungal acne, then shines a special light on your skin to help eradicate it. You'll likely have several sessions over the course of a couple of months with 2 weeks between sessions.[16]
- In between sessions, follow your dermatologist's instructions for treating the area and keeping it clean.
-
4Use an antifungal product at least once a week. After you've treated fungal acne and your skin has cleared, there's still a possibility that the fungus could return.[17] Using a topical treatment at least once a week can help ensure this doesn't happen.[18]
- For example, if you found that dandruff shampoo worked for you to eliminate the fungal acne, you might include that treatment as part of your self-care routine once a week.
- Your dermatologist might also prescribe a specific antifungal wash for you to use, at least until your next followup appointment.
- Be mindful of your skin so when you see signs of a possible return you can treat it quickly before it spreads.
Expert Q&A
-
QuestionHow do I know if I have fungal acne or regular acne?
 Asmi Sanghvi, DODr. Asmi Sanghvi is a Board Certified Dermatologist based in New York, New York. She specializes in general and cosmetic dermatology and has a passion for educating others. Dr. Sanghvi has been published in several peer-reviewed journals, including the Journal of the American Academy of Dermatology and Cutis. She holds a BS in Human Communication Sciences from Northwestern University and a DO from Lake Erie College of Osteopathic Medicine.
Asmi Sanghvi, DODr. Asmi Sanghvi is a Board Certified Dermatologist based in New York, New York. She specializes in general and cosmetic dermatology and has a passion for educating others. Dr. Sanghvi has been published in several peer-reviewed journals, including the Journal of the American Academy of Dermatology and Cutis. She holds a BS in Human Communication Sciences from Northwestern University and a DO from Lake Erie College of Osteopathic Medicine.
Board Certified Dermatologist Fungal acne can actually look very similar to regular (bacterial) acne. To differentiate, them, remember that regular acne usually occurs in different sizes and forms, while fungal acne are all the same size. Also, fungal acne appears in clusters, while bacterial acne is more spread out.
Fungal acne can actually look very similar to regular (bacterial) acne. To differentiate, them, remember that regular acne usually occurs in different sizes and forms, while fungal acne are all the same size. Also, fungal acne appears in clusters, while bacterial acne is more spread out. -
QuestionWhat products are best for fungal acne?
 Asmi Sanghvi, DODr. Asmi Sanghvi is a Board Certified Dermatologist based in New York, New York. She specializes in general and cosmetic dermatology and has a passion for educating others. Dr. Sanghvi has been published in several peer-reviewed journals, including the Journal of the American Academy of Dermatology and Cutis. She holds a BS in Human Communication Sciences from Northwestern University and a DO from Lake Erie College of Osteopathic Medicine.
Asmi Sanghvi, DODr. Asmi Sanghvi is a Board Certified Dermatologist based in New York, New York. She specializes in general and cosmetic dermatology and has a passion for educating others. Dr. Sanghvi has been published in several peer-reviewed journals, including the Journal of the American Academy of Dermatology and Cutis. She holds a BS in Human Communication Sciences from Northwestern University and a DO from Lake Erie College of Osteopathic Medicine.
Board Certified Dermatologist You should use a combination of oral and topical antifungals. Try using creams twice a day for a few weeks. Also, use a ketoconazole shampoo twice a week as a body wash for a few weeks. Oral therapies include 2-3 weeks of daily antifungals, prescribed by a dermatologist.
You should use a combination of oral and topical antifungals. Try using creams twice a day for a few weeks. Also, use a ketoconazole shampoo twice a week as a body wash for a few weeks. Oral therapies include 2-3 weeks of daily antifungals, prescribed by a dermatologist. -
QuestionAre all back acnes fungal?
 Asmi Sanghvi, DODr. Asmi Sanghvi is a Board Certified Dermatologist based in New York, New York. She specializes in general and cosmetic dermatology and has a passion for educating others. Dr. Sanghvi has been published in several peer-reviewed journals, including the Journal of the American Academy of Dermatology and Cutis. She holds a BS in Human Communication Sciences from Northwestern University and a DO from Lake Erie College of Osteopathic Medicine.
Asmi Sanghvi, DODr. Asmi Sanghvi is a Board Certified Dermatologist based in New York, New York. She specializes in general and cosmetic dermatology and has a passion for educating others. Dr. Sanghvi has been published in several peer-reviewed journals, including the Journal of the American Academy of Dermatology and Cutis. She holds a BS in Human Communication Sciences from Northwestern University and a DO from Lake Erie College of Osteopathic Medicine.
Board Certified Dermatologist Not necessarily, but since fungal acne is more common on the arms, chest, and back, it could be the case. Bacterial acne, on the other hand, is more common on the face.
Not necessarily, but since fungal acne is more common on the arms, chest, and back, it could be the case. Bacterial acne, on the other hand, is more common on the face.
Warnings
- If you have a fever over 101 °F (38 °C), contact your doctor immediately. You may have a more serious infection.[19]⧼thumbs_response⧽
References
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3970831/
- ↑ https://dermnetnz.org/topics/malassezia-folliculitis/
- ↑ https://www.uofmhealth.org/health-library/hw171614
- ↑ Asmi Sanghvi, DO. Board Certified Dermatologist. Expert Interview. 16 August 2021.
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3970831/
- ↑ https://www.uofmhealth.org/health-library/d04395t1
- ↑ https://www.uofmhealth.org/health-library/hw171614
- ↑ https://www.uofmhealth.org/health-library/hw171614
- ↑ https://www.mayoclinic.org/diseases-conditions/folliculitis/symptoms-causes/syc-20361634
- ↑ https://www.uofmhealth.org/health-library/hw171614
- ↑ https://www.uofmhealth.org/health-library/hw171614
- ↑ https://www.uofmhealth.org/health-library/hw171614
- ↑ Asmi Sanghvi, DO. Board Certified Dermatologist. Expert Interview. 16 August 2021.
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3970831/
- ↑ https://jamanetwork.com/journals/jamapediatrics/fullarticle/485898
- ↑ https://pubmed.ncbi.nlm.nih.gov/20166153/
- ↑ Asmi Sanghvi, DO. Board Certified Dermatologist. Expert Interview. 16 August 2021.
- ↑ https://www.dermatologytimes.com/view/it-acne-or-pityrosporum-folliculitis
- ↑ https://www.uofmhealth.org/health-library/hw171614