This article was medically reviewed by Erik Kramer, DO, MPH. Dr. Erik Kramer is a Board-Certified Primary Care Physician at the University of Colorado. With over 15 years of experience, his clinical interests include obesity and weight management, diabetes care, and preventive care, as well as embracing a holistic approach to primary care. He received his Doctorate in Osteopathic Medicine (D.O.) from the Touro University Nevada College of Osteopathic Medicine and completed his residency at Central Maine Medical Center. Dr. Kramer is a Diplomate of the American Board of Obesity Medicine.
There are 9 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 51,687 times.
Parkinson’s Disease (PD) is a progressive neurodegenerative disorder affecting both motor and non-motor abilities. It afflicts 1% of those over 60 years of age.[1] It is a progressive disorder of the central nervous system. PD is caused by a lack of dopamine, a chemical that helps the parts of your brain responsible for motor function (or body movement) communicate with each other. This condition often causes tremors, muscle stiffness, slowness, and poor balance. If you suspect that you, or someone you love, has Parkinson’s, it is important to know how you can diagnose this condition. Begin by trying to identify symptoms of the disease at home, and then see your doctor for an appropriate medical diagnosis.[2]
Steps
Recognizing Symptoms of Parkinson’s Disease
-
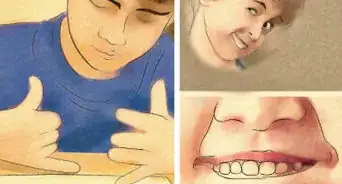
1Watch for tremors in your hands and/or fingers. One of the first complaints presented to doctors by many people later diagnosed with Parkinson’s Disease is an involuntary tremor or shaking of the hands, fingers, arms, legs, jaw, and face.[3] [4] You’re most likely to notice this tremor when your hands are at rest rather than when you’re using them, although you may see more tremors while your hands and arms are in use as the disease progresses.
- There are many causes of tremors. Parkinson's Disease is one of the most common causes, and tremors are often the first sign of the disease.
- The tremor and other symptoms may initially appear only on one side of the body, or they may appear worse on one side than the other.
- A repetitive “pill-rolling" movement between the thumb and finger—named because it looks as though the person is rolling a pill between their fingers—is characteristic of a Parkinsonian tremor.[5]
-
2Check for slowed or distorted movements. Some symptoms of Parkinson's are caused by the larger symptom of slowed movements (also known as bradykinesia).[6] This primarily affects motor functions from walking and balance to writing and even motor functions that are often considered reflexive or spontaneous.
- These slowed movements are a very common early sign of Parkinson’s, and may show up at the onset of the disease in 80% of patients.
- Some people might have a hard time describing what they are feeling and use words like “weakness,” “tiredness,” or “incoordination” when talking about these symptoms.
- Look for distortions in voluntary movements. In addition to involuntary movements, those with Parkinson’s may experience disturbances in their voluntary movements beyond just slowness. Some of the treatments used for Parkinson's disease may cause abnormal involuntary movements, or an increase in movement, referred to as dyskinesia. These distortions (dyskinesias) can be similar to a “tic” in appearance and worsen with psychological stress.
- Advanced dyskinesia is most often seen in patients who have been on the medication Levodopa for some time.
Advertisement -
3Look out for a shuffling gait. A common symptom of Parkinson’s is a shuffling gait with short steps and a tendency to lean forward. People with Parkinson's often have difficulty with their balance, and there is sometimes a tendency to fall forward, causing the person to walk faster and faster to keep from falling over. This pattern is called a "festinating gait," and it is very common in Parkinson's disease.[7]
- This symptom typically shows up in the later stages of the disease.
-
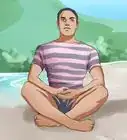
4Examine your posture. Those with Parkinson’s Disease often lean forward at the waist when standing or walking. This is because Parkinson's can cause posture and balance problems, including rigidity. There is a tendency to flex the arms and the head so that the person appears bent over with the elbows flexed and the head down.[8]
- Rigidity can affect the whole body, and might you feel stiff or sore.
- Check for postural rigidity. Also referred to as “cog-wheeling,” this symptom presents as a hallmark, rigid motion when an examiner moves the arm of a patient through basic flexion and extension motions. The rigidity and resistance to movement is most obvious with passive movement of the wrists and elbow.
- Cog-wheeling may happen when the increased muscle tone related to rigidity is combined with a tremor.
-
5Examine for cognitive impairment. Some cognitive impairment is common, but usually not until late in the course of the disease.[9]
-
6Check for speech disturbances. Around 90% of those with PD will show signs of speech disturbances at some point. These can present as quieter speech, breathy or hoarse qualities to the voice, and reduced precision with language.[10]
- The voice often becomes soft or whispery because the vocal muscles lack mobility.
-
7Watch for signs of depression or anxiety. Up to 60% of those with PD may show signs or anxiety or depression. PD affects some of the mood-stabilizing portions of the brain, which leads to this increased chance for depression, especially paired with the quality of life for patients in late stages of the disease.[11]
-
8Check for gastrointestinal issues. The muscles used to push food through the digestive system are also affected by PD. This can lead to a variety of gastrointestinal issues from incontinence to constipation.
- These same symptoms often present along with difficulty swallowing food as well.
-
9Watch for difficulty sleeping. Many of the involuntary movements associated with Parkinson’s make it increasingly difficult for those with the disease to get a full night of sleep. Other symptoms—such as muscle rigidity making it difficult to roll over at night or bladder issues leading to getting up at night to urinate frequently—compound the sleep disruptions experienced by those with PD.[12]
Testing for Parkinson’s Disease
-
1Test symptoms at home. While symptoms alone cannot provide an accurate diagnosis, you can test for the symptoms elsewhere in this article in order to provide your doctor a complete case of your symptoms. The first thing your doctor would do if you came in asking about PD is perform a physical exam, and you can look for some of the same signs they would look for.
- Rest your hand in your lap and look for tremor. Unlike most other forms of tremor, the tremor associated with Parkinson's is worse when you are at rest.
- Note your posture. Most people with Parkinson's usually stand slightly bent forward, with the head down and the elbows flexed.
-
2See your doctor. Ultimately a diagnosis can only come from your doctor. Make an appointment and tell them your case history and concerns. If your physician thinks PD is among the potential causes, then they will likely run a few tests to help determine the diagnosis.[13]
- Note that Parkinson’s Disease is not difficult to diagnose, except in the very early stages. There is no single test your doctor will perform. Instead, your doctor may run other tests to eliminate other conditions that lead to similar symptoms as Parkinson’s (such as stroke, hydrocephalus, or benign essential tremor). The condition that most often mimics PD is essential tremor, which often runs in families and is most marked with the hands outstretched.
- Your doctor may also refer you to a neurologist, which is a doctor who specializes in conditions of the nervous system.
-
3Have a physical examination. The first thing your doctor will do is give you a physical exam looking for a variety of different indicators:
- Is your expression animated?
- Do you show signs of a tremor with your arms at rest?
- Do you exhibit rigidity in your neck or limbs?
- How easily can you stand up from a sitting position?
- Do you have a normal gait, and do your arms swing symmetrically as you walk?
- When given a small push, are you quickly able to resume your balance?
-
4Agree to further tests if necessary. Imaging tests, such as MRI, ultrasound, SPECT, and PET scans, are not usually very helpful in diagnosing Parkinson's.[14] However, in some cases your doctor may recommend one of these tests to help them distinguish between Parkinson's and diseases that present similar symptoms. Due to the expense of such scans, the invasive nature of the procedures, and the plain lack of availability of the machines, it is unlikely that your doctor will recommend these scans as a diagnostic tool in most cases.
- An MRI may help your physician distinguish between PD and conditions that display similar symptoms, such as progressive supranuclear palsy and multi-system atrophy.
-
5Measure your response to treatment. Treatment involves increasing the effect of dopamine (the neurotransmitter affected by PD) in the brain. Treatment may consist of administering levodopa, the most commonly prescribed and most effective drug for PD, on its own (usually as a levodopa/carbidopa combination). In some cases, your doctor may also prescribe a dopamine agonist, such as pramipexole, that stimulates the dopamine receptors.[15]
- If your symptoms are advanced enough to warrant use of medication, then your doctor may prescribe it to see if it curbs any of the symptoms you experience. Diseases that mimic PD tend to respond to treatment less well than PD does. A good response to medication makes PD more likely.
Treating Parkinson’s Disease
-
1Try medications. Unfortunately, there aren't any cures for Parkinson’s Disease yet. However, a wide array of medications are available to treat different symptoms. Some of the medications for treating PD include:[16]
- Levodopa/Carbidopa (Sinemet, Parcopa, Stalevo, etc.), which treats the various motor symptoms seen in both early and advanced PD
- Dopamine agonists (Apokyn, Parlodel, Neupro, etc.), which stimulate dopamine receptors to trick the brain into believing it is receiving dopamine
- Anticholinergics (Artane, Cogentin, etc.), which are primarily used to help treat tremors
- MAO-B inhibitors (Eldepryl, Carbex, Zelapar, etc.), which help enhance the effects of levodopa
- COMT inhibitors (Comtan, Tasmar), which block the body’s metabolism of levodopa, prolonging the effects
-
2Exercise to slow the progression of the disease. Though exercise is by no means a permanent solution to the effects of PD, it has been shown to reduce stiffness and improve mobility, gait, posture, and balance Aerobic exercises that require good biomechanics, posture, rotation, and rhythmic movements have proven especially beneficial. Types of exercise that can help include:[17]
-
3See a physical therapist. To find the best fitness regimen based on your specific progression of PD, consult a physical therapist. A physical therapist can tailor a routine to target the areas where you have started experiencing stiffness or decreased mobility.[18]
- You should also consult your physical therapist for periodic reevaluation of your routine both to ensure maximum effectiveness of the regimen and to keep up with the progression of the disease.
-
4Ask about surgical options for treating PD. Deep brain stimulation (DBS) is a surgical procedure that has revolutionized the treatment of PD in its later stages. The procedure involves implanting electrodes into the targeted region of the brain, which are then connected to an impulse generator inserted beneath the collarbone. The patient is then given a controller to turn the device on or off at necessary times.[19]
- The effects of DBS are often dramatic and doctors may recommend this route for those who experience disabling tremors, those with adverse side effects to medication, or if medications begin losing their efficacy.
References
- ↑ JOHN D. GAZEWOOD, MD, MSPH,D. ROXANNE RICHARDS, MD,KARL CLEBAK, MD, Parkinson’s An Update, The American Family Physician, 2013 Feb 15;87(4):267-273
- ↑ https://www.parkinson.org/understanding-parkinsons/what-is-parkinsons
- ↑ JOHN D. GAZEWOOD, MD, MSPH,D. ROXANNE RICHARDS, MD,KARL CLEBAK, MD, Parkinson’s An Update, The American Family Physician, 2013 Feb 15;87(4):267-273
- ↑ Reuter, I., Engelhardt, M., Freiwaldt, J., & Baas, H. (1999). Exercise test in Parkinson's disease. Clinical Autonomic Research, 9(3), 129-134.
- ↑ JOHN D. GAZEWOOD, MD, MSPH,D. ROXANNE RICHARDS, MD,KARL CLEBAK, MD, Parkinson’s An Update, The American Family Physician, 2013 Feb 15;87(4):267-273
- ↑ JOHN D. GAZEWOOD, MD, MSPH,D. ROXANNE RICHARDS, MD,KARL CLEBAK, MD, Parkinson’s An Update, The American Family Physician, 2013 Feb 15;87(4):267-273
- ↑ JOHN D. GAZEWOOD, MD, MSPH,D. ROXANNE RICHARDS, MD,KARL CLEBAK, MD, Parkinson’s An Update, The American Family Physician, 2013 Feb 15;87(4):267-273
- ↑ JOHN D. GAZEWOOD, MD, MSPH,D. ROXANNE RICHARDS, MD,KARL CLEBAK, MD, Parkinson’s An Update, The American Family Physician, 2013 Feb 15;87(4):267-273
- ↑ Natalie C Palavra, Sharon L Naismith, Simon J Lewis Mild Cognitive Impairment in Parkinson’s Disease: A Review of Current Concepts Neurology Research International June 2013 Article ID 576091 doi 10.1155/2013/576091
- ↑ https://medlineplus.gov/parkinsonsdisease.html
- ↑ JOHN D. GAZEWOOD, MD, MSPH,D. ROXANNE RICHARDS, MD,KARL CLEBAK, MD, Parkinson’s An Update, The American Family Physician, 2013 Feb 15;87(4):267-273
- ↑ https://medlineplus.gov/parkinsonsdisease.html
- ↑ https://my.clevelandclinic.org/health/diseases/8525-parkinsons-disease-an-overview
- ↑ https://my.clevelandclinic.org/health/diseases/8525-parkinsons-disease-an-overview
- ↑ https://www.nhs.uk/conditions/parkinsons-disease/treatment/
- ↑ https://www.nhs.uk/conditions/parkinsons-disease/treatment/
- ↑ https://www.nia.nih.gov/health/parkinsons-disease
- ↑ https://www.nhs.uk/conditions/parkinsons-disease/treatment/
- ↑ https://www.ninds.nih.gov/health-information/patient-caregiver-education/hope-through-research/parkinsons-disease-hope-through-research#therapies




































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...