This article was medically reviewed by Danielle Jacks, MD and by wikiHow staff writer, Jennifer Mueller, JD. Danielle Jacks, MD is a Surgical Resident at Ochsner Clinic Foundation in New Orleans, Louisiana. She has over six years of experience in general surgery. She received her MD from Oregon Health and Science University in 2016.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 18,846 times.
Being told you have uterine (or endometrial) polyps may sound scary, but they're usually not cause for any alarm. Uterine polyps, also called endometrial polyps, are small growths on the endometrium, which is the lining of the uterus. Smaller polyps may not cause any symptoms and often go away on their own. However, larger polyps may cause troubling symptoms, such as irregular menstrual periods or excessively heavy bleeding during periods. If these symptoms become more than you can manage, your gynecologist may recommend surgical removal. Once removed, polyps seldom return, but your doctor will still want to continue to monitor your condition.[1]
Steps
Having Uterine Polyps Removed
-
1Get the polyps removed during the hysteroscopy procedure. If your gynecologist conducted a hysteroscopy to confirm their diagnosis of uterine polyps, they may go ahead and remove them using the same procedure. They remove the polyps by inserting a small surgical device or laser through the scope.[2]
- This is a minimally invasive procedure that typically doesn't require general anesthesia. You'll likely be able to go home within a few hours after the procedure.
- Full recovery typically takes about 2 weeks. Your gynecologist may ask you not to engage in penetrative intercourse during that time. You may also experience cramping and vaginal bleeding, similar to a period.
Tip: Removed polyps will likely be sent to a lab for microscopic analysis to determine if they are cancerous. Your gynecologist will contact you when they get results back from the lab. Uterine polyps are usually not cancerous.
-
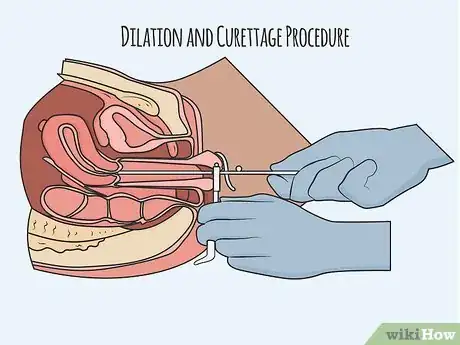
2Submit to a dilation and curettage procedure if necessary. In this procedure, your gynecologist dilates your cervix with the assistance of surgical instruments or medication, then scrapes the inner walls of your uterus with a curette to remove uterine tissue.[3]
- Some curettes are sharp, while others use suction. Recovery is generally the same regardless of which type of curette your gynecologist uses.
- Your gynecologist may use twilight sedation or general anesthesia to put you under during the procedure. Depending on the anesthesia used, you may have to wait in a recovery room for anywhere from a few minutes to a few hours for the effects to wear off.
- After the procedure, cramping and bleeding are to be expected, similar to having a normal period.
Tip: A dilation and curettage procedure can also be used to confirm a diagnosis of uterine polyps. However, gynecologists can typically use less invasive means to confirm a diagnosis.
Advertisement -
3Return for additional treatment if necessary. Occasionally uterine polyps return after you've had them removed. Your doctor will monitor your condition to see if they return. At the first signs of re-growth, your doctor may offer treatment or medication to get rid of them before they start to cause you problems again.[4]
- Your gynecologist may ask you to keep a record of your menstrual cycle and average flow during your period so they can monitor for any irregularities.
- If you have symptoms return after removal of uterine polyps, contact your gynecologist. Keep in mind that those symptoms may indicate a different condition, rather than the return of the polyps.
-
4Undergo a hysterectomy as a last resort. If the polyps are cancerous, or if they can't be removed using any other surgical method, your gynecologist may recommend a hysterectomy. With this surgical procedure, your entire uterus is removed.[5]
- A hysterectomy is a surgery that requires general anesthesia, but it’s often performed as an outpatient procedure. However, this may vary depending on the reason for the hysterectomy.
- Your gynecologist typically would only recommend a hysterectomy if other methods to remove the polyps had been unsuccessful, or if the polyps keep coming back after they're removed.
- You may experience weight gain and other side effects after a hysterectomy. However, you can lose this added weight with a few changes to your diet and lifestyle.
Recognizing the Symptoms of Uterine Polyps
-
1Track your menstrual cycle. An irregular menstrual cycle is the most common symptom of uterine polyps. A normal menstrual cycle is 21 to 35 days long, with a period that lasts 4 to 7 days. If your menstrual cycle is irregular and unpredictable, or if your period lasts longer than 7 days, you might have uterine polyps.[6]
- There are many other things that can also cause an irregular menstrual cycle. Visit your gynecologist for a pelvic exam and they will evaluate the possibilities.
- If you're trying to get pregnant and are unable to get pregnant, or unable to carry a pregnancy to term, this could also be a sign of uterine polyps. However, keep in mind that there are many other reasons you may be having trouble conceiving.
-
2Keep records of your flow during and between periods. If your flow during your period is unusually heavy are unpredictable, this can also be a sign of uterine polyps. Bleeding or spotting between periods, or bleeding after penetrative intercourse, may also occur.[7]
- For example, suppose the first day of your period is normally your heaviest day, followed by a couple of days of regular flow, and then a couple of days of light flow. However, in the past few months, you've had heavier flow sporadically throughout your period. This might be a symptom of uterine polyps.
- It’s also important to see your doctor if you have any post-menopausal bleeding. This may indicate uterine fibroids or polyps, or it may signal something more serious, such as a malignancy.
- Schedule an appointment with your gynecologist and let them know that you suspect you might have uterine polyps. Provide them a copy of your records of your menstrual cycle and your flow. They will examine you and rule out any other possible causes of these symptoms.
Tip: There are smartphone apps that you can use to track your menstrual cycle and flow, many of which are free. You can also keep a regular journal with pen and paper if you choose.
-
3Evaluate your vaginal discharge. Vaginal discharge varies throughout your menstrual cycle. However, if you have unusual or abnormal vaginal discharge, this may be a sign that you have uterine polyps.[8]
- There are many factors that can also cause a change in the consistency, color, and odor of your vaginal discharge, including your diet, activity level, and certain STIs. For example, a yeast infection causes abnormal discharge. If you notice unusual discharge, try to eliminate other possible causes first.
-
4Consider whether or not you have any of the risk factors. There's no real way to prevent uterine polyps from growing. However, some things may increase your chance of developing polyps. Risk factors for uterine polyps include:[9]
Tip: Uterine polyps often have no symptoms whatsoever. This is just one of the many reasons why regular gynecological exams are important. Make an appointment for a wellness checkup at least once a year.
Diagnosing and Treating Uterine Polyps
-
1Visit your gynecologist for a pelvic exam and pap smear. If uterine polyps extend beyond the cervix, your gynecologist may be able to identify and diagnose them during a basic pelvic exam. A pap smear can also reveal the existence of uterine polyps.[13]
- While your gynecologist may be able to diagnose uterine polyps right away, further testing is typically required to confirm the diagnosis.
- At your appointment, your gynecologist will also ask you questions to eliminate other possible causes of your symptoms.
-
2Return for further testing to confirm the diagnosis. If your gynecologist isn't able to confirm their initial diagnosis of uterine polyps, they may want to do additional procedures that will allow them to see inside your uterus. Some tests your gynecologist may recommend include:[14]
- Transvaginal ultrasound: a wand-like device placed in your vagina emits sound waves that create an image of the inside of your uterus, allowing your gynecologist to see any polyps or other abnormalities
- Hysterosonography: similar to an ultrasound, except that saline is injected into your uterus. The saline expands your uterine cavity so your gynecologist can see the inside of your uterus.
- Hysteroscopy: a thin, flexible, lighted telescope is inserted through your vagina and cervix into your uterus, allowing your gynecologist to examine it
- Endometrial biopsy: your gynecologist uses a suction catheter inside your uterus to remove a sample of uterine tissue for testing
-
3Go with the "watch and wait" approach if the polyps are small. Small polyps that cause mild symptoms (if any) often go away on their own without needing any further treatment. Depending on the severity of your symptoms, your gynecologist may recommend this approach.[15]
- Maintain detailed records of your menstrual cycle and other possible symptoms during this time. If any new symptoms appear or existing symptoms increase in severity, contact your gynecologist as soon as possible.
Tip: If there is a history of uterine cancer in your family, make sure your gynecologist knows. That history and other risk factors may affect your treatment options.
-
4Take medication to lessen your symptoms. Hormonal medications, such as progestins and gonadotropin-releasing hormone agonists, can lessen the symptoms of uterine polyps. At times they can even shrink the polyps. However, taking medication typically doesn't eliminate the polyps entirely.[16]
- The benefits of medication are typically relatively short-lived. If you stop taking the medications, your symptoms will return and might be more severe than they were when you started the medications.
- Hormonal medications may also have side effects that may be more uncomfortable for you than your uterine polyp symptoms. Discuss possible side effects with your gynecologist before committing to a hormonal medication.
References
- ↑ https://www.bcm.edu/healthcare/care-centers/obstetrics-gynecology/conditions/endometrial-polyps
- ↑ https://my.clevelandclinic.org/health/diseases/14683-uterine-polyps
- ↑ https://medlineplus.gov/ency/article/007636.htm
- ↑ https://my.clevelandclinic.org/health/diseases/14683-uterine-polyps/prevention
- ↑ https://www.nhs.uk/conditions/hysterectomy/why-its-done/
- ↑ https://www.acog.org/womens-health/faqs/abnormal-uterine-bleeding#
- ↑ https://my.clevelandclinic.org/health/diseases/14683-uterine-polyps
- ↑ https://www.womens-health-concern.org/help-and-advice/factsheets/uterine-polyps/
- ↑ https://medlineplus.gov/ency/article/007636.htm
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/27116465
- ↑ https://my.clevelandclinic.org/health/diseases/14683-uterine-polyps
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/23344409
- ↑ https://www.bcm.edu/healthcare/care-centers/obstetrics-gynecology/conditions/endometrial-polyps
- ↑ https://medlineplus.gov/ency/article/007636.htm
- ↑ https://www.bcm.edu/healthcare/care-centers/obstetrics-gynecology/conditions/endometrial-polyps
- ↑ https://journals.sagepub.com/doi/full/10.1177/2050312119848247











-Step-3.webp)















-Step-3.webp)






































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...