This article was medically reviewed by Janice Litza, MD. Dr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
There are 18 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 56,451 times.
TSH (thyroid-stimulating hormone) is produced by your pituitary gland, and it helps regulate your thyroid. When TSH levels are low, it usually means your thyroid is overactive and producing more thyroid hormone than necessary, which is a condition that requires medical evaluation. The quickest solution is to get a diagnosis and undergo treatment as soon as you suspect there's a problem. While hyperthyroidism, or an overactive thyroid, is the most common cause, other medical conditions and some medications can also suppress TSH levels. Your doctor can provide an accurate diagnosis and recommend the right solution.
Steps
Identifying the Underlying Cause
-
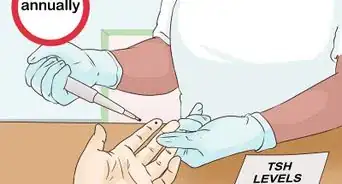
1Have your T3 and T4 levels tested, if you haven’t already. TSH tells your thyroid to produce hormones called T3 and T4. If your TSH levels are low and your T3 and T4 levels are high, your thyroid is overactive. If your TSH, T3, and T4 levels are all low, you might have a pituitary gland disorder.[1]
- Your doctor will order a blood test to measure your hormone levels. They might also test for antibodies, which would indicate an infection, or perform a radioactive iodine uptake scan to see if your thyroid is overactive.[2]
- When the pituitary gland produces higher levels of TSH, it usually means the thyroid isn’t making enough hormones. Low TSH levels usually mean the thyroid is producing too many hormones.
- It usually takes 24 to 48 hours to get results for TSH and thyroid hormone tests.
-
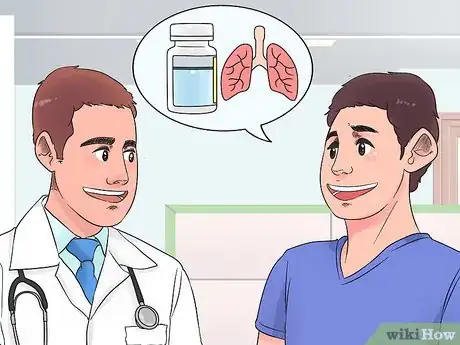
2Ask your doctor if you take any medications that suppress TSH levels. Some medications for asthma, inflammation, Parkinson’s disease, and cancer can cause low TSH levels. Tell your doctor about all medications you take, and ask if they recommend any changes to your regimen.[3]
- You might not be able to stop taking certain medications, so your doctor might just monitor your condition.
- If you experience unusual symptoms, such as rapid heartbeat or unexplained weight loss, your doctor might recommend thyroid medication.
Advertisement -
3Adjust your dosage if you take medication for hypothyroidism. High T3 and T4 counts along with low TSH levels are signs that you’re taking too much medication for an underactive thyroid. Your doctor will decrease your dose, then they’ll check your levels at a follow-up appointment to make sure the adjustment worked.[4]
- You'll likely see your doctor again within 6 weeks of changing your dose. They'll check your levels and, if necessary, make further adjustments.
- High or low hormone levels are common during treatment for hypothyroidism, and finding the right balance can take time. If you take thyroid medication, you'll most likely have your hormone levels tested every 6 to 12 months once the levels are stable and every 6 to 8 weeks after a dose change.
-
4Get tested for a pituitary gland disorder if your T4 levels are low. If your test results show that your thyroid hormone levels are also low, there might be something preventing your pituitary gland from producing TSH. If necessary, your doctor will order blood work and imaging scans to check for a pituitary gland disorder.[5]
- Low TSH levels can be caused by pituitary gland tumors, which are almost always benign (not cancerous). If a tumor is detected, you’ll receive hormone or radiation therapy, or have it surgically removed.[6]
- Cases of low TSH levels due to a pituitary gland disorder are rare. Most of the time, an overactive thyroid gland is the issue.
Managing an Overactive Thyroid
-
1Take a prescription antithyroid medication for short-term management. Antithyroid medications are usually only taken for a few weeks, or until a patient undergoes radioactive iodine therapy, which is the most common treatment. Take your medication as directed, and don’t stop taking it without your doctor’s approval.[7]
- Antithyroid medications, such as methimazole, are usually taken with food every 8 hours.[8]
- Tell your doctor if you experience any side effects, such as upset stomach, skin rash, joint or muscle pain, and unusual numbness, tingling, or burning.
- Women who are pregnant or breastfeeding can’t undergo radioactive iodine therapy. If you’re pregnant or breastfeeding and need to manage hyperthyroidism, you’ll need to take antithyroid medications until it’s safe to undergo radioactive iodine therapy.
-
2Control an overactive thyroid with radioactive iodine therapy. Most people with hyperthyroidism receive radioactive iodine therapy. Typically, you’ll take a single capsule or liquid dose of a substance that permanently destroys thyroid tissue. As a result of treatment, your thyroid will be underactive, and you’ll likely need to take medication to replace thyroid hormones.[9]
- You might experience a sore throat for a few days after taking radioactive iodine.
- Most of the radioactive material will be absorbed by your thyroid within 2 days, but your bodily fluids will also temporarily contain small amounts after treatment. You’ll need to take precautions to prevent exposing others to these traces of radioactive iodine.
- Your doctor will most likely instruct you to avoid contact with small children and pregnant women for several days. You should also avoid prolonged periods of intimate contact with other people for 3 to 4 days.
-
3Ask your doctor if they recommend a beta-blocker. A beta-blocker doesn’t treat hyperthyroidism, but it can help manage symptoms such as rapid heartbeat, shaking, and nervousness. Take any medication as prescribed, and don’t stop taking your medicine without consulting your doctor.[10]
- Side effects can include dizziness, fatigue, diarrhea, and constipation. Call your doctor if any side effects are severe or persistent.[11]
-
4Undergo surgery if other treatment options aren't possible. Usually, thyroid surgery is only recommended for people who have a large goiter, an abnormal enlargement of the thyroid, or who have nodules on their thyroid that may be cancerous. You might also need surgery if you can’t take antithyroid medication or undergo radioactive iodine therapy.[12]
- Thyroid surgery usually takes around 2 hours, and many people are able to go home the same day as the operation.
- After undergoing surgery, you’ll need to avoid strenuous activity for at least 2 weeks. Follow your doctor’s postoperative instructions, and attend all scheduled follow-up appointments.[13]
-
5Take medication for hypothyroidism as directed. Almost all people develop hypothyroidism, or an underactive thyroid, after receiving treatment for hyperthyroidism. Your doctor will prescribe a hormone replacement medication and monitor your TSH, T3, and T4 levels. You’ll need to remain on medication for hypothyroidism permanently and have your levels tested every 6 to 12 months when your levels are stable and 6 to 8 weeks after a dosage change to ensure that these counts are balanced. Make sure to take the medication without food or other medications to ensure that your body absorbs it properly.[14]
- After starting medication for hypothyroidism, you'll need to have your hormone levels checked within 6 weeks. If necessary, your doctor will adjust your dosage. You might have additional follow-up appointments every 2 to 3 months until your thyroid is regulated.
- It might seem strange that treatment for an overactive thyroid leads to an underactive thyroid. Hypothyroidism is easily managed with medication, but hyperthyroidism is a potentially life-threatening condition. Treatment for hyperthyroidism is necessary, even if it results in hypothyroidism.
Making Lifestyle Changes
-
1Follow a low-iodine diet while undergoing treatment. Avoid iodized salt, seafood, seaweed, dairy products, and egg yolks, and limit the amounts of grain, meat, and poultry you eat. Try not to eat more than 1⁄2 cup (120 mL) of pasta and 6 ounces (170 g) of meat or poultry per day.[15]
- Stick to a low-iodine diet as directed by your doctor. After treating hyperthyroidism, you might need to switch to a normal, iodine-rich diet to promote healthy thyroid function.
- High amounts of iodine can aggravate hyperthyroidism. Additionally, during radioactive iodine therapy, you'll need to limit your iodine intake to ensure your thyroid absorbs the radioactive substance instead of non-radioactive iodine.[16]
-
2Keep your stress levels in check. When you feel overwhelmed or anxious, take deep, slow breaths. Visualize calming scenery, such as a relaxing vacation spot or a safe place from your childhood. Try to set aside time every day to relax, such as by listening to soothing music, taking a bubble bath, or reading a good book.[17]
- Stress can worsen hyperthyroidism and trigger related symptoms, such as rapid heartbeat and shaking. Do your best to manage your stress levels, especially before and during treatment.
-
3Ask your doctor to recommend calcium and vitamin D supplements. High amounts of thyroid hormones can prevent your body from absorbing calcium and vitamin D, which can lead to brittle bones. While a supplement can help, it’s important to consult your doctor before taking any vitamin or supplement.[18]
- Some supplements contain iodine, which could aggravate hyperthyroidism or interfere with radioactive iodine therapy.
- Additionally, calcium can prevent your body from absorbing medication for an underactive thyroid. If your doctor recommends a calcium supplement, avoid taking it within 6 to 8 hours of your medication.
-
4Consume more calories and protein if you’ve experienced weight loss. If you've experienced weight loss and muscle wasting due to hyperthyroidism, you might need to consume more calories and nutrients. If you’re on a low-iodine diet, ask your doctor for advice about consuming more calories and protein from low-iodine sources, such as legumes.[19]
- If you’re not on a low-iodine diet, add calories by eating more pastas, grains, and lean protein sources, such as poultry and seafood.
- Avoid strenuous exercise while managing hyperthyroidism. You need to burn fewer calories and, since hyperthyroidism makes your heart work harder, excessive exercise can be dangerous.[20]
-
5Eat fewer calories once your thyroid becomes underactive. If you develop hypothyroidism after undergoing treatment, you might gain weight and have a harder time losing weight. To manage weight gain, keep track of your caloric intake, and avoid eating more calories than your recommended daily amount.[21]
- Your daily recommended calorie and nutrient values depend on your age, sex, and activity level. Learn more about your specific needs at https://www.choosemyplate.gov.
- Check labels and look up the nutritional contents for any item you eat or drink. Log your caloric intake in a journal or use a fitness tracking app.
- Cutting soft drinks and other high-calorie beverages is a simple way to cut your caloric intake.
- Eat more fruits and vegetables, and cut down on fatty cuts of red meat, sweets, and unhealthy snacks.
-
6Consult your doctor about exercising if you have thyroid issues. Exercise is usually great for your health, but it can be dangerous if your thyroid hormone levels are uncontrolled. Whether you have hyperthyroidism or hypothyroidism, ask your doctor to recommend an exercise regimen that's right for you.[22]
- If you have hyperthyroidism, your body is under constant stress, as if you were running on a treadmill 24 hours a day. Excessive exercise can cause heart problems and other medical issues.
- If you have hypothyroidism, your heart rate is slow, and excessive exercise is like a sudden, stressful jolt.
- Once you've regulated your hormone levels, moderately intense exercise, like walking briskly for 30 minutes a day, can boost your energy and control weight.
Warnings
- Always take any medication according to your doctor's instructions, and follow their recommendations regarding diet, exercise, and other lifestyle choices.⧼thumbs_response⧽
- Don't try to increase TSH levels quickly with supplements, non-prescribed medication, or by increasing your thyroid medication dosage without consulting your doctor.⧼thumbs_response⧽
References
- ↑ https://medlineplus.gov/ency/article/003684.htm
- ↑ https://www.thyroid.org/thyroid-function-tests/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2784889/
- ↑ https://medlineplus.gov/ency/article/000309.htm
- ↑ https://www.pituitary.org.uk/news/2017/03/problems-with-the-assessment-of-thyroid-function-in-pituitary-disease/
- ↑ https://www.pituitary.org.uk/information/symptoms,-diagnosis-and-tests/diagnosis/
- ↑ https://www.thyroid.org/hyperthyroidism/
- ↑ https://medlineplus.gov/druginfo/meds/a682464.html
- ↑ https://www.radiologyinfo.org/en/info.cfm?PG=radioiodine
- ↑ https://www.thyroid.org/hyperthyroidism/
- ↑ https://medlineplus.gov/druginfo/meds/a682607.html
- ↑ https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease
- ↑ https://www.thyroid.org/thyroid-surgery/
- ↑ https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease
- ↑ https://www.thyroid.org/low-iodine-diet/
- ↑ https://www.thyca.org/download/document/408/LIDSlides.pdf
- ↑ https://www.cancercenter.com/community/blog/2020/05/covid-ways-to-help-relax
- ↑ https://familydoctor.org/condition/hyperthyroidism/
- ↑ https://www.thyroid.org/wp-content/uploads/patients/brochures/Thyroid_and_Weight.pdf
- ↑ https://health.clevelandclinic.org/uncontrolled-thyroid-exercise-diet-risks/
- ↑ https://www.thyroid.org/wp-content/uploads/patients/brochures/Thyroid_and_Weight.pdf
- ↑ https://health.clevelandclinic.org/uncontrolled-thyroid-exercise-diet-risks/
- ↑ https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease
























-Step-12-Version-2.webp)
















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...