This article was co-authored by Neal Blitz, DPM, FACFAS. Dr. Neal Blitz is a Podiatrist and Foot & Ankle Surgeon who runs private practices in New York City and in Beverly Hills, California. Dr. Blitz is “The Bunion King®” and is the creator of the Bunionplasty® Procedure (plastic surgery for bunions) which has revolutionized bunion surgery. He has over 17 years of podiatric experience and specializes in minimally invasive foot and ankle surgery. Dr. Blitz received his DPM from the New York College of Podiatric Medicine, then completed a residency focused on Elective & Reconstructive Foot & Ankle Surgery at the Swedish Medical Center, and was awarded an AO Trauma fellowship in Dresden, Germany, focused on trauma and reconstructive techniques. He is board certified in Foot Surgery and Reconstructive Rearfoot & Ankle Surgery and is also a Diplomate of the American Board of Foot & Ankle Surgery and a fellow of the American College of Foot & Ankle Surgeons (FACFAS).
There are 19 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, several readers have written to tell us that this article was helpful to them, earning it our reader-approved status.
This article has been viewed 380,946 times.
If you've ever gotten a yeast infection or athlete's foot, you may not have realized that you actually had a skin fungus. A fungus is a group of organisms that make spores. Fungi, the word for more than one fungus, live most everywhere and usually don't cause infections or skin growths. But, you may occasionally get fungal growths on your skin, like ringworm, athlete's foot, jock itch, or vaginal yeast infection. Don't worry. Fungal infections on the skin are not life-threatening and don't usually cause significant harm or damage. And, there are things you can do to reduce your risk of getting a skin fungus.
Steps
Reducing Your Risk
-
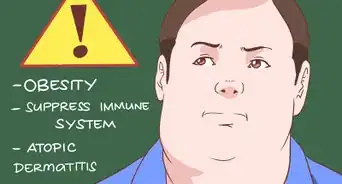
1Learn who is at risk of getting a fungal infection. There are some things that may increase your risk of a fungal infection, like sharing clothing or personal care products (brushes/combs) with an infected person.[1] But, some people are also more likely to get an infection, based on risk factors. Individuals at risk include:
- People who have depressed immune systems from medications, steroids, other infections or illnesses[2]
- People taking long-term antibiotics or immunosuppressant drugs
- People or babies who are incontinent or unable to hold their urine (this creates a moist genital environment)
- People who perspire heavily
- Individuals who work or spend time in an environment where they come in contact with people who are at high risk, such as nurses, school teachers, hospitalized patients, students and coaches.
-
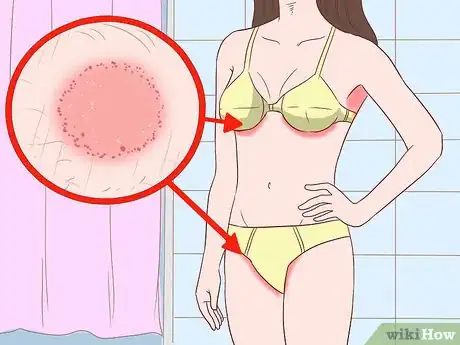
2Recognize what areas of your skin are at risk of a fungal infection. Parts of your skin that are moist are more at risk for fungal infections since the fungus needs moisture to thrive.[3] These parts include the areas between your toes, under the breast tissue, in the genital region (including the vaginal area), and between folds of skin.Advertisement
-
3Take care in public places. Since fungal infections are contagious, you can get them from exposure to skin cells that have the infection. Try to reduce your exposure to public areas where other people with fungal infections may have been.[4] If you use public locker rooms, showers, or pools, wear flip flops. You shouldn't ever share towels or combs in the locker room either.[5]
- Never touch other people's infections or share shoes.
-
4Keep your skin clean and dry. Fungi live in warm, moist areas, like between the toes or in the groin.[6] By keeping your skin clean and dry you reduce the potential for infection. There are several things you can do to keep dry:
- Change your socks once daily or twice daily if you sweat a lot. Let your bath towels air dry completely before using them a second time.[7]
- Clean and dry any skinfold areas such as under the breast or under the stomach. Apply a drying or medicated powder to the skin folds when you are exercising or are going to be in a hot environment.
- You should also alternate your shoes so they can dry completely between wearings, especially if they get sweaty. Also, wash your athletic supporter after each use.
-
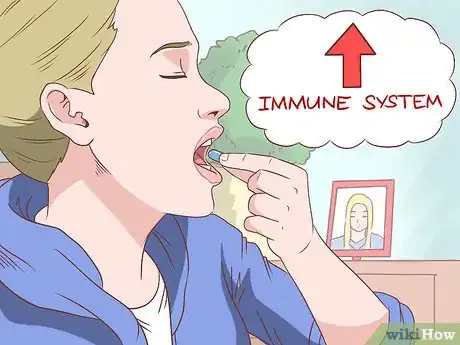
5Boost your immune system. You're more likely to get a fungal infection if you have a depressed immune system. To improve your immune system, take a daily vitamin supplement[8] and consider taking a probiotic.[9] Try to eat a balanced diet high in healthy fats and reduce your carbohydrate intake. You should also stay hydrated by drinking water. Your urine should be very light yellow in color.[10] Your immune system may also benefit from 8 hours of sleep a night.[11]
- Your immune system may not be in the best shape, even if you don't have a medical condition or are taking medications that might depress it. This makes it important to strengthen your immune system.
-
6Prevent current infections from spreading. If you already have a fungal infection, prevent it from spreading to more parts of your body or to your family members. Other family members should be examined and treated, if infection is suspected. Since fungal infections are contagious, take the following precautions to prevent spreading the infection:[12]
- Avoid scratching your infection. Wash your hands frequently and keep them dry.
- Use flip flops in the shower if you have athlete's foot.
- Wash all towels in warm, soapy water and dry in the dryer. Use a clean towel every time your shower or clean up.
- Clean your bathroom sink, tub, and floor well after using.[13]
- Wear clean, dry clothes every day and avoid sharing clothes or socks.
- Treat all infected pets.
- Children and adults may want to use medicated shampoo 2 to 3 times a week for 6 weeks to prevent tinea capitis (itching/ringworm of the scalp).
- Soak combs and brushes for 1 hour a day in a mixture of half bleach and half water for 3 days if you have tinea capitis. Don't share combs, brushes, hats, pillows, helmets, or towels with other people.
Recognizing Symptoms
-
1Determine if you have ringworm. Although it goes by several different names depending upon the location on the body, all are caused by the same fungus (not a parasitic worm, despite the name). If you have athlete's foot, jock itch or ringworm the fungus is the same, the location is different. The symptoms may be slightly different depending on the location of the fungal infection.
-
2Recognize the symptoms for athlete's foot. Athlete's foot, also called tinea pedis, causes red or itchy skin around and between the toes, and less often on the soles of the feet. You may experience burning or stinging pain and the skin will blister and crust.[14] You may also find red, scaly bumps between your toes.[15]
-
3Learn the symptoms of Jock Itch. Jock Itch, also called tinea cruris, is common mostly in teen boys and adult men. Symptoms include red, raised scaly patches with defined borders that blister in the groin. They are redder on the outside and more flesh colored on the inside, giving them a classic ring appearance of ringworm. They can also cause abnormally dark or light pigmentation on the skin which can be permanent.[16]
- This infection is more common in boys who play athletics and spend time in a public locker room.[17] They may also have athlete's foot from the same fungus with which they reinfect themselves in the groin.
-
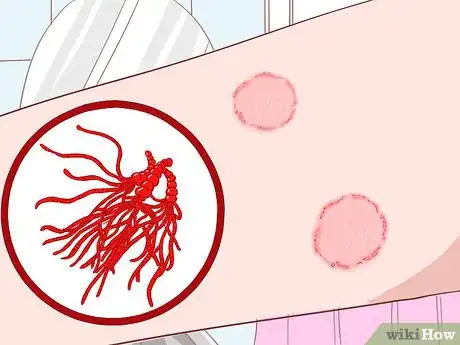
4Check your body for ringworm. Tinea corporis is a ringworm infection which appears on the body, but not the scalp, inside a beard, on the feet or in the groin area. It begins as a small raised red area that looks like small pimples. It is itchy and quickly becomes scaly. The rash will slowly take on a ring shape classic to ringworm with a redder exterior border and a flesh colored middle.[18]
- You should also look for dermatophytids (a rash). This rash affects another part of your body and can accompany body ringworm. You may experience an itchy bumpy rash on your fingers which is related to an allergic reaction to the fungus. This does not result from touching an infected area.[19]
-
5Look at facial hair for ringworm. Tinea barbae is ringworm found in a man's facial hair. It can cause a deeper infection in the follicles of a man's beard and may result in permanent hair loss from scarring with follicular infection. Symptoms include a reddened area on the skin that is itchy and can become scaly. Depending upon the location you can see the classic ring characteristic with redder border and more flesh colored interior. The man will also lose hair growth with an active fungal infection.
- You should also look for dermatophytids (a rash). This rash affects another part of your body and can accompany facial ringworm. You may experience an itchy bumpy rash on your fingers which is related to an allergic reaction to the fungus. This does not result from touching an infected area.[20]
-
6Watch for symptoms of ringworm on your scalp. Tinea capitis is ringworm found on the scalp and may involve a small portion or the whole head. Areas that are infected will be itchy and red, often inflamed and can have pus filled sores. It also may cause a lot of scaling of the scalp, either in one area, or of a large part of the scalp. You can also look for 'black dots', which are the broken hairs that occur with scalp ringworm. Individuals with tinea capitis will lose their hair during an active infection and the infection can cause lasting scar tissue and permanent hair loss if not treated properly. Individuals may also experience a low grade fever below 101 degrees Fahrenheit or swollen lymph nodes in the neck area as your body is fighting the infection.[21]
- You should also look for dermatophytids (a rash). This rash affects another part of your body and can accompany tinea capitis, or ringworm on your scalp. You may experience an itchy bumpy rash on your fingers which is related to an allergic reaction to the fungus. This does not result from touching an infected area.[22]
-
7Recognize if you have a vaginal yeast infection. Yeast are actually fungus and can cause vaginal infections for women. The vagina, labia, and vulva can all be affected by a yeast infection. You shouldn't try to treat symptoms at home if you've had more than 4 infections in the last year, are pregnant, have uncontrolled diabetes, have a depressed immune system, or have tears, cracks, fissures, or sores in the vaginal area. Most yeast infection symptoms range from mild to moderate and include:[23]
- Itching and irritation in the vagina or at the entrance to the vagina
- Redness or swelling at the entrance to the vagina
- Vaginal pain and soreness
- Burning sensation with urination or intercourse
- Vaginal discharge that has a cottage cheese appearance and is white, thick and odorless
Treating Skin Fungus
-
1Treat athlete's foot. Over-the-counter antifungal powders or creams are effective in controlling or eliminating the infection. Look for products that contain miconazole, clotrimazole, terbinafine, or tolnaftate. Follow the packaged instructions and apply the medication for at least 2 weeks and an additional 1-2 weeks after the infection is cleared to prevent it from returning.[24] Wash your feet twice a day with soap and water. Be sure to dry your feet and between the toes, then put on a clean pair of socks after each washing.
- Wear shoes that are well ventilated and made of natural materials. You should also alternate your shoes everyday to give them time to dry out thoroughly.
- If you have athlete's foot that isn't responding to home treatment, your doctor may prescribe oral medications after testing your infection by taking a culture.
-
2Treat Jock Itch. Use over-the-counter antifungal products to help control the infection. These medications should contain miconazole, tolnaftate, terbinafine or clotrimazole. You should notice the infection start to clear up within a few weeks. If it lasts longer than 2 weeks, is severe, or returns frequently (more than 4 times a year), you should see your doctor.[25] If it doesn't respond to home treatment, your doctor may prescribe oral medications after testing your infection by taking a culture.
- Avoid wearing tight clothing or anything that rubs or irritates the skin.
- Wash all undergarments and athletic supporters after one use.
-
3Treat ringworm on the body. Use over-the-counter creams that contain oxiconazole, miconazole, clotrimazole, ketoconazole or terbinafine. Follow packaged instructions for 10 days. In general, you should wash and dry the area, then apply the cream from the outside to the center of the infection. Wash and dry your hands after applying the cream. Don't put a bandage over ringworm because it will keep the moisture in your skin.[26]
- If you have ringworm on your scalp or beard you must see your doctor for treatments. If you have ringworm on the body that isn't responding to home treatment, your doctor may prescribe oral medications after testing your infection by taking a culture.
- If you're treating school-aged children for ringworm, they can return to classes once treatment has started.
-
4Treat vaginal infections. Uncomplicated vaginal yeast infections can be treated with over-the-counter preparations. Use antifungal vaginal suppository creams, foams, tablets, or ointments from a class of azoles. These include butoconazole, miconazole, clotrimazole, and terconazole. You may notice some slight burning or irritation to the area when you apply the medication. Always follow the packaged instructions.[27]
- The oil-based nature of these creams can weaken a latex condom or diaphragm. If these are your forms of birth control, realize that they may not be as effective while using the medication.
-
5Treat complications from vaginal infections. You may need long-course vaginal therapy that includes using a prescription vaginal cream in the “azole” family which is stronger than what can be purchased over-the-counter. You'll use the cream for 10 to 14 days. If you have complications from vaginal yeast infections, your doctor may prescribe fluconazole (Diflucan) to be taken 1 time by mouth.[28] Or, you may be given 2 to 3 doses of fluconazole by mouth, instead of a cream. This is not recommended for pregnant women.
- If you have repeated infections, you may take a maintenance dose of fluconazole once a week for 6 months or a vaginal suppository of clotrimazole.
-
6See your doctor if you have diabetes or a depressed immune system. Your doctor will need to help you treat fungal infections because diabetes or a depressed immune system can increase your risk of experiencing more severe symptoms from a fungal infection.
- See your doctor for early treatment to reduce potential health problems or significant secondary infections from scratching.
-
7See your doctor if a fungal infection is on your scalp or your beard. Your doctor will give you an oral medication that will include griseofulvin, terbinafine or itraconazole. Take the medication according to your doctor's instructions, usually for a minimum of 4 weeks and up to 8 weeks. You can improve your chance for successful treatment by:[29]
- Keeping the area clean and dry
- Washing the hair and beard with medicated shampoo that contains selenium sulfide or ketoconazole. This will help stop the spread but will not get rid of the current infection.
Expert Q&A
-
QuestionHow can you prevent fungal infections from spreading?
 Neal Blitz, DPM, FACFASDr. Neal Blitz is a Podiatrist and Foot & Ankle Surgeon who runs private practices in New York City and in Beverly Hills, California. Dr. Blitz is “The Bunion King®” and is the creator of the Bunionplasty® Procedure (plastic surgery for bunions) which has revolutionized bunion surgery. He has over 17 years of podiatric experience and specializes in minimally invasive foot and ankle surgery. Dr. Blitz received his DPM from the New York College of Podiatric Medicine, then completed a residency focused on Elective & Reconstructive Foot & Ankle Surgery at the Swedish Medical Center, and was awarded an AO Trauma fellowship in Dresden, Germany, focused on trauma and reconstructive techniques. He is board certified in Foot Surgery and Reconstructive Rearfoot & Ankle Surgery and is also a Diplomate of the American Board of Foot & Ankle Surgery and a fellow of the American College of Foot & Ankle Surgeons (FACFAS).
Neal Blitz, DPM, FACFASDr. Neal Blitz is a Podiatrist and Foot & Ankle Surgeon who runs private practices in New York City and in Beverly Hills, California. Dr. Blitz is “The Bunion King®” and is the creator of the Bunionplasty® Procedure (plastic surgery for bunions) which has revolutionized bunion surgery. He has over 17 years of podiatric experience and specializes in minimally invasive foot and ankle surgery. Dr. Blitz received his DPM from the New York College of Podiatric Medicine, then completed a residency focused on Elective & Reconstructive Foot & Ankle Surgery at the Swedish Medical Center, and was awarded an AO Trauma fellowship in Dresden, Germany, focused on trauma and reconstructive techniques. He is board certified in Foot Surgery and Reconstructive Rearfoot & Ankle Surgery and is also a Diplomate of the American Board of Foot & Ankle Surgery and a fellow of the American College of Foot & Ankle Surgeons (FACFAS).
Board Certified Podiatrist Always clean and bleach your shower thoroughly so the fungus doesn't spread to other people in your household.
Always clean and bleach your shower thoroughly so the fungus doesn't spread to other people in your household.
Warnings
- See your doctor for treatment if you have a depressed immune system from medications or illness. You should also see your doctor for fungal treatment if you have diabetes.⧼thumbs_response⧽
References
- ↑ https://www.cdc.gov/fungal/diseases/ringworm/risk-prevention.html
- ↑ http://www.cdc.gov/fungal/infections/
- ↑ http://my.clevelandclinic.org/health/diseases_conditions/hic_Contact_Dermatitis/hic_How_to_Care_for_a_Fungal_Rash
- ↑ Neal Blitz, DPM, FACFAS. Board Certified Podiatrist. Expert Interview. 22 April 2020.
- ↑ https://www.cedars-sinai.org/health-library/diseases-and-conditions/t/tinea-infection.html
- ↑ Neal Blitz, DPM, FACFAS. Board Certified Podiatrist. Expert Interview. 22 April 2020.
- ↑ https://www.footcare.net/blog/153750-is-there-fungus-growing-in-your-socks_4
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3166406/
- ↑ http://www.health.harvard.edu/staying-healthy/how-to-boost-your-immune-system
- ↑ http://ajl.sagepub.com/content/5/4/304.abstract
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3258559/
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000877.htm
- ↑ Neal Blitz, DPM, FACFAS. Board Certified Podiatrist. Expert Interview. 22 April 2020.
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000875.htm
- ↑ https://my.clevelandclinic.org/health/diseases/4276-skin-fungus
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000876.htm
- ↑ https://kidshealth.org/en/parents/jock-itch.html
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000877.htm
- ↑ https://www.merckmanuals.com/home/skin-disorders/fungal-skin-infections/overview-of-fungal-skin-infections
- ↑ https://www.merckmanuals.com/home/skin-disorders/fungal-skin-infections/overview-of-fungal-skin-infections
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000878.htm
- ↑ https://www.merckmanuals.com/home/skin-disorders/fungal-skin-infections/overview-of-fungal-skin-infections
- ↑ http://www.mayoclinic.org/diseases-conditions/yeast-infection/basics/symptoms/con-20035129
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000875.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000876.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000877.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/yeast-infection/basics/treatment/con-20035129
- ↑ http://www.mayoclinic.org/diseases-conditions/yeast-infection/basics/treatment/con-20035129
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000878.htm
About This Article
To prevent skin fungus, one of the best things you can do is keep your skin clean and dry since fungal infections thrive in moist, dirty environments. If you sweat a lot, change your socks once or twice a day, alternate which shoes you wear so they have time to dry out, and apply drying powder to skin folds where you tend to get sweaty. You can also prevent skin fungus by boosting your immune system with a daily vitamin supplement and probiotic. Make sure you eat a balanced diet, drink plenty of water, and get enough sleep every night since that can affect your immune system as well. Additionally, always wear flip flops in public locker rooms, pools, and showers since fungal infections are contagious. For advice from our Medical co-author, like how to recognize the symptoms of skin fungus, scroll down.












































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...