This article was medically reviewed by Lacy Windham, MD. Lacy Windham, MD, is a Board-Certified Obstetrician & Gynecologist in Cleveland, Tennessee. Dr. Windham attended medical school at the University of Tennessee Health Science Center in Memphis. Her residency was completed at Eastern Virginia Medical School in Norfolk, Virginia. She was the recipient of multiple awards during her residency training, including Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, Most Outstanding Resident Overall, and Special Award in Minimally Invasive Surgery.
There are 15 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 63,367 times.
Studies show that ovarian cancer is very rarely detected in early stages, as symptoms often don't appear until later stages.[1] Ovarian cancer is cancer that starts in the ovaries, the organs that produce and release the eggs. If you aren’t sure whether you have symptoms, it is best to err on the side of caution and get checked by a doctor. Research suggests that if you do have ovarian cancer, the outcome is generally better when it is detected earlier.[2]
Steps
Recognizing the Symptoms
-
1Identify possible symptoms. It is important to recognize that at the early stages, the symptoms are not very distinctive. Other conditions like pre-menstrual syndrome (PMS) or irritable bowel syndrome (IBS) have symptoms that are very similar. So if you do have these symptoms, it does not mean that you definitely have cancer. But it does mean that you should get checked. Symptoms include:[3] [4]
- A distended or bloated abdomen that doesn’t go away
- Pain in your pelvis or abdomen that doesn’t go away
- Loss of appetite, feeling full quickly, or nausea associated with eating
- Weight loss
- Constipation
- Urinating more frequently
-
2Consider whether you may have a higher risk. Some things may increase a person’s risk of developing ovarian cancer. These risk factors don’t mean that you will develop it, but just that your chances may be somewhat higher. If you think you are at a higher risk, ask your doctor if you should be checked regularly.[5] [6]
- Ovarian cancer is most likely to occur over the age of 50.
- Some people may have a genetic predisposition to developing ovarian cancer. This may be true for those with the breast cancer gene 1 (BRCA 1), breast cancer gene 2 (BRCA 2), or mutations that are related to Lynch syndrome and colon cancer. Having these mutations does not mean you will develop cancer, but it means your risk is higher. If you have a family history of these cancers, you should tell your doctor.
- Using estrogen hormone replacement therapy over a long period of time with a high dosage may increase your risk.[7]
- Menstruating for a long period of time may increase the risk. For example, this would include people who started their periods before age 12, people who menstruated until they were over 50, people who have not been on hormonal contraception, or not been pregnant. This occurs because during each ovulation, the ovaries rupture to release and egg. The tissue then heals, with a small risk of abnormal cell growth occurring during the process.
- Fertility treatments may increase the risk.
- Smoking increases your risk of ovarian cancer and other cancers.
- Medical conditions such as polycystic ovary syndrome and endometriosis may make you more vulnerable to ovarian cancer.
Advertisement -
3Learn about the different types of ovarian cancers. Ovarian cancers are categorized based on where the cancer cells begin.[8] [9]
- Epithelial tumors are the most frequent kind of ovarian cancer. In this type of cancer, the tumor starts in the outside layer of the ovaries. Roughly 90 percent of ovarian cancers are epithelial tumors.
- Stromal tumors start in the parts of the ovaries that produce hormones. These types of ovarian cancers make up about 7 percent of the total.
- Germ cell tumors are very rare, making up only about 1 or 2 percent of the total number of ovarian cancers. In this type, the tumors start where the eggs are produced.
Going to the Doctor
-
1Get a pelvic exam. During a pelvic exam your doctor is likely to do several things which will help evaluate whether you have ovarian cancer. These include:[10]
- Inspecting your abdomen and genitals.
- Feeling your uterus and ovaries by putting gloved fingers in your vagina and simultaneously using the other hand to press your uterus and ovaries against the fingers in your body. This may be slightly uncomfortable, but should not cause pain.
- Looking inside your vagina with a speculum
-
2Discuss imaging tests with your doctor. Depending upon what your doctor found during the pelvic exam, it may be advisable to get more information through additional tests. These tests can help the doctor evaluate the size and shape of your ovaries:[11] [12]
- An ultrasound
- An X-ray
- A CT scan
- An MRI scan
-
3Consider a blood test. Some types of ovarian cancer cells make a protein referred to as CA125. This means that high levels of it may signal cancer. This is, however, not a screening test – it is used when there is already a concern for cancer. Other conditions can also raise the level of this protein, so it must be done in connection with other tests. Some other conditions that elevate the level of this protein are:[13]
- Endometriosis
- Pelvic Inflammatory Disease
- Fibroids
- Pregnancy
-
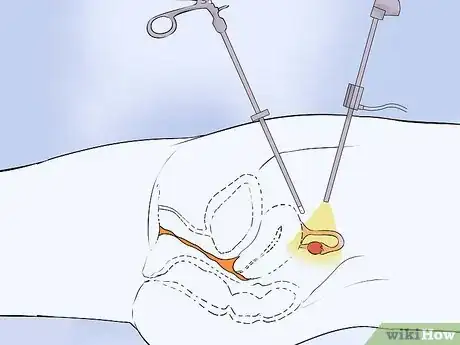
4Use invasive tests to get more definite information. These tests will let the doctor test directly for cancerous cells:[14]
- Laparoscopy. During this procedure the doctor inserts an tiny camera through a little cut in your abdomen and looks at the ovaries directly.
- A biopsy. The doctor may take a small sample of tissue from your ovaries and test it to see if it is cancerous.
- Abdominal fluid aspiration. During this procedure the doctor uses a long needle to extract some fluid from your abdomen. That fluid will then be examined to see if it has abnormal cells in it.
Understanding your Diagnosis
-
1Ask your doctor at what stage the cancer is. This will help you to understand how far along it is. There are four commonly used categories:[15] [16]
- Stage 1: The cancer is only in the ovaries. It may be in one or both ovaries.
- Stage 2: The cancer is also in the pelvis or uterus.
- Stage 3: The cancer has spread to the abdomen. It may be in the lining of the abdomen, bowels, or lymph nodes in the pelvis.
- Stage 4: The cancer has spread beyond the abdomen. It may be in other organs such as the liver, spleen, or lungs.
-
2Inquire about what grade your cancer is. This will help you to understand how aggressively your doctor expects the cancer to grow.[17]
- Low grade cells are cancerous, but grow slowly.
- Moderate grade cells are more abnormal and grow faster than low grade cells.
- High grade cells are highly abnormal and grow aggressively.
-
3Discuss treatment options with your doctor. The best course of action will depend on your particular situation including your overall health, the stage, and the grade of the cancer. Most treatment plans incorporate:[18] [19]
- Surgery to remove as much of the cancerous tissue as possible
- Chemotherapy to kill cancerous cells
-
4Get emotional support. Cancer is both physically and emotionally exhausting. You will be more physically and psychologically resilient if you have emotional support.[20]
- Talk with trusted friends and family members
- Seek out a support group where you can talk with people who are also experiencing similar things
- Reduce your stress by giving yourself time to rest and to sleep. You may need more than the usual 8 hours of sleep per night.
References
- ↑ https://www.mayoclinic.org/diseases-conditions/ovarian-cancer/symptoms-causes/syc-20375941
- ↑ http://www.mayoclinic.org/diseases-conditions/ovarian-cancer/basics/definition/con-20028096
- ↑ http://www.nhs.uk/Conditions/Cancer-of-the-ovary/Pages/Symptoms.aspx
- ↑ http://www.mayoclinic.org/diseases-conditions/ovarian-cancer/basics/symptoms/con-20028096
- ↑ http://www.mayoclinic.org/diseases-conditions/ovarian-cancer/basics/risk-factors/con-20028096
- ↑ http://www.nhs.uk/Conditions/Cancer-of-the-ovary/Pages/Causes.aspx
- ↑ http://www.cancer.org/cancer/cancercauses/othercarcinogens/medicaltreatments/menopausal-hormone-replacement-therapy-and-cancer-risk
- ↑ http://www.mayoclinic.org/diseases-conditions/ovarian-cancer/basics/causes/con-20028096
- ↑ http://www.cancerresearchuk.org/about-cancer/type/ovarian-cancer/about/types-of-ovarian-cancer
- ↑ http://www.mayoclinic.org/diseases-conditions/ovarian-cancer/basics/tests-diagnosis/con-20028096
- ↑ http://www.mayoclinic.org/diseases-conditions/ovarian-cancer/basics/tests-diagnosis/con-20028096
- ↑ http://www.nhs.uk/Conditions/Cancer-of-the-ovary/Pages/Diagnosis.aspx
- ↑ http://www.nhs.uk/Conditions/Cancer-of-the-ovary/Pages/Diagnosis.aspx
- ↑ http://www.nhs.uk/Conditions/Cancer-of-the-ovary/Pages/Diagnosis.aspx
- ↑ http://www.nhs.uk/Conditions/Cancer-of-the-ovary/Pages/Diagnosis.aspx
- ↑ http://www.mayoclinic.org/diseases-conditions/ovarian-cancer/basics/tests-diagnosis/con-20028096
- ↑ www.nhs.uk/Conditions/Cancer-of-the-ovary/Pages/Diagnosis.aspx. It
- ↑ http://www.mayoclinic.org/diseases-conditions/ovarian-cancer/basics/treatment/con-20028096
- ↑ http://www.nhs.uk/Conditions/Cancer-of-the-ovary/Pages/Treatment.aspx
- ↑ http://www.mayoclinic.org/diseases-conditions/ovarian-cancer/basics/coping-support/con-20028096
About This Article
If you think you might have ovarian cancer, look for common symptoms like a distended abdomen and pelvic pain that won’t go away, loss of appetite, weight loss, and frequent urination. While these symptoms can point towards ovarian cancer, they aren’t very distinctive, so you shouldn’t count out other conditions like premenstrual syndrome or irritable bowel syndrome. Also, consider whether you may have a higher risk of developing ovarian cancer, since it is most likely to occur in people over the age of 50. You may also have a higher risk if you used estrogen hormone replacement therapy or fertility treatments. No matter what symptoms you notice, err on the side of caution and see a doctor to get a proper diagnosis. For more help from our Medical co-author, including how to better understand the different types of ovarian cancer, read on.












-Step-13.webp)


-Step-8-Version-3.webp)


















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...