This article was co-authored by Peter Gardner, MD. Peter W. Gardner, MD is a board certified physician who has practiced Gastroenterology and Hepatology for over 30 years. He specializes in diseases of the digestive system and liver. Dr. Gardner earned his Bachelor’s degree from the University of North Carolina and attended Georgetown Medical School. He completed his residency in Internal Medicine and then his fellowship in Gastroenterology at the University of Connecticut. He is a previous Chief of Gastroenterology at Stamford Hospital and remains on the staff. He is also on the staff of Greenwich Hospital and New York (Columbia) Presbyterian Hospital. Dr. Gardner is an Approved Consultant in Internal Medicine and Gastroenterology with the American Board of Internal Medicine.
There are 31 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 38,897 times.
Colitis is an inflammation of the large intestine that can result in abdominal pain and diarrhea.[1] It can also be associated with inflammation of the small intestine (enteritis).[2] Colitis can have a variety of causes, and treatment depends on cause and type. You can treat mild to moderate cases at home with over-the-counter medication, but severe cases call for professional medical attention.
Steps
Determining the Cause
-
1Learn what colitis is. This condition is an inflammation or swelling of the large intestine and colon.[3] It's often the result of other underlying conditions like infection or autoimmune disease. However, colitis is a serious condition in its own right, and you should always inform a healthcare professional if you develop symptoms.[4] Treatment of colitis depends on the cause, and can range from home care to prescription medications.
-
2Take note of general colitis symptoms. The different types of colitis have different causes, and therefore different symptoms and treatments.[5] However, there are some general signs for colitis that can let you know that you need to look more closely for the specific diagnosis. The general symptoms of colitis include:[6]
- Abdominal pain and bloating.
- Bloody stools. These could appear either dark, tar like or red.
- Fever and/or chills.
- Diarrhea and/or dehydration.
Advertisement -
3Seek medical attention immediately. Colitis is a serious, potentially fatal condition that requires expert evaluation as soon as possible. Provide the doctor with a detailed list of your symptoms, as well as how long you've observed them. Be able to list any other medical conditions you may have, as well as any medications you're taking. Depending on the cause your doctor suspects, he may run a number of different tests. For example:
- Bacterial infection: The lab will analyze stool samples to identify the bacteria causing the infection. They may also test for your white blood cell count, which is usually increased if you have inflammation or infection.[7]
- IBD: If your doctor suspects inflammatory bowel disease, the lab may do a blood test for anemia (low red blood cells) or signs of infection.[8]
- They may also analyze stool samples rule out other causes or check for the presence of white blood cells in your stool, which points to colitis.
- You may also need a colonoscopy, biopsy, or imaging scans to rule out other conditions or determine the extent of inflammation.[9]
-
4Get checked for an infection.[10] Infectious colitis results from any type of infection — bacterial, viral, or parasitic. Infection is the most common cause of colitis in children.[11] Common infectious causes include:
- Bacterial: food poisoning from Escherichia coli, Shigella, or Salmonella.
- Viral: cytomegalovirus (CMV) infection.
- Parasitic: Entamoeba histolytica.
-
5Consider pseudomembranous colitis if you've taken antibiotics recently because they may kill too much of your beneficial bacteria. Without enough good bacteria, then Clostridium difficile (C. diff) can take over. C. diff may develop after taking clindamycin, fluoroquinolone, penicillin, or cephalosporin. Antibiotics are often prescribed for a bacterial infection, but most antibiotics do not kill off C. diff because it has a spore form that is not effected by antibiotics. This bacterium can cause intense intestinal toxins and inflammation. Though treatable, pseudomembranous colitis is potentially fatal, so alert a doctor immediately if you develop symptoms:[12]
- Watery or bloody diarrhea
- Abdominal cramps and pain
- Fever
- Pus or mucus in your stool
- Nausea/loss of appetite
- Dehydration
-
6Think about whether you have inflammatory bowel disease (IBD). This is a general umbrella term that covers three more specific conditions that cause inflammation in the intestines. IBD might refer to ulcerative colitis, Crohn's disease, or indeterminate colitis.[13] Other symptoms of IBD include:[14]
- Cramping
- Irregular or bloody bowel movements
- Weight loss
- Fever or sweats
- Fatigue
-
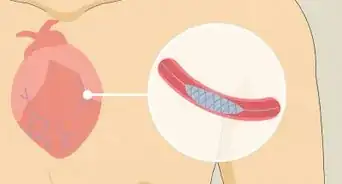
7Look for signs of ischemic colitis.[15] When local arteries get too narrow or are otherwise blocked, it reduces blood flow to the large intestine, causing ischemic colitis. Although you can feel pain anywhere in the colon, most patients feel it on the left side of the belly. Symptoms of ischemic colitis include:
- Abdominal pain, tenderness or cramping (sudden or gradual)
- Bright red or maroon-colored blood in your stool
- Rectal bleeding without stool
- Urgent bowel movements
- Diarrhea
-
8Suspect necrotizing enterocolitis (NEC) in newborns.[16] Babies who are born premature or who take formula instead of breast milk may suffer from NEC, usually within two to three weeks of birth. It occurs more rarely in full- and near-term babies, but symptoms can show up from one to three days after birth through the first month of life. NEC can be incredibly dangerous, with a mortality rate of 50% or more, so report symptoms immediately:
- Vomiting
- Diarrhea
- Delayed bowel movements
- Distended and/or tender stomach
- A decrease in bowel sounds
- Erythema (redness) of the stomach in advanced stages
- Bloody stool
- Sleep apnea (stopping breathing during sleep)
- Lethargy
- Trouble breathing
Getting Medical Treatment
-
1Consult your healthcare provider about medicinal treatments. There are several types of medications that are used to help control IBD.[17] [18]
- Aminosalicylates target colon inflammation, but are less effective at treating the small intestine. These drugs are usually used to treat mild to moderate colitis.
- Sulfasalazine is effective, but side effects include nausea, vomiting, diarrhea, heartburn, and headache.
- Corticosteroids fight inflammation, but suppress all immune response instead of focusing on the colon. These drugs (prednisone, methylprednisolone) are used for moderate to severe colitis. Side effects include weight gain, excessive facial hair growth, mood swings, high blood pressure, type 2 diabetes, osteoporosis, bone fractures, cataracts, glaucoma, and an increased risk of infection.
- Azathioprine and mercaptopurine act slowly, so they're usually prescribed alongside a corticosteroid.
- Immunomodulators, like corticosteroids, suppress immune response to calm inflammation. They're usually used only when aminosalicylates and corticosteroids have failed.
- Cyclosporine is a very strong medication that begins to work within one or two weeks. Since it is so strong and comes with a range of severe side effects, it is generally only prescribed until less toxic medications can take effect.
- Infliximab and adalimumab fight intestinal inflammation specifically. Infliximab can cause problems in people with cancer or a history of heart disease.
-
2Consider antibiotic use. Antibiotics don't treat the colitis itself. If intestinal ulcers cause infection though, antibiotics will prevent further complications.
- Antibiotics can treat abscesses of fistulas (abnormal connections between organs or vessels) seen in Crohn's Disease and usually occurring in the small intestine.[19]
- Tell your doctor if you develop a fever, which could indicate infection.
-
3Talk to your doctor about biologic therapies.[20] Though it may sound "natural" or "herbal," biologic therapies take their name from the fact that they're developed from biological material — usually protein. This treatment targets the chemicals responsible for inflammation. These fairly new medications are used for moderate to severe colitis if other treatments have failed.
- They're also known as anti-TNF agents. Tumor necrosis factor (TNF) is a naturally produced chemical responsible for inflammation.
- Biologic therapies produce antibodies that attach themselves to the TNF, so that it can be destroyed by the body.
- Your doctor must test you for tuberculosis before you can begin TNF.
-
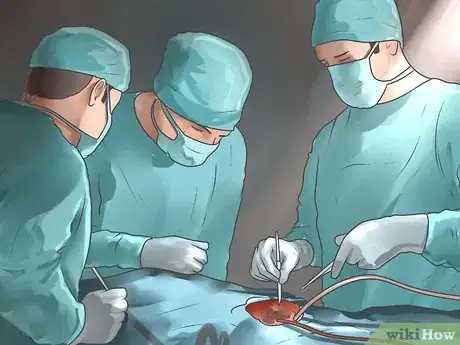
4Be prepared for surgery if necessary. If your colitis is so severe that no medication, home cure, or alternative treatment can keep it in check, you might need to have a colectomy. During this surgery, part or all of your colon will be removed. Removal of your colon will lead to lifestyle changes.[21] Although most people will be able to do most of the routine activities they did before, you have to live with a stoma (a hole in your abdomen from which waste is expelled).[22]
- The only way to cure colitis completely is to have a total colectomy performed. Since a total colectomy can come with adverse side effects (like small bowel obstruction), though, a partial colectomy is sometimes done instead.
- The surgeon may also opt to perform a procedure that links the small intestine to the anus, thereby producing more normal bowel function.
Caring for Colitis at Home
-
1Take antibiotics for colitis from bacterial infection.[23] Bacterial gastroenteritis or food poisoning can result from eating or drinking contaminated food or water. Usually, this type of colitis will go away on it’s own in two to three days. But if the infection is severe, your doctor may prescribe an antibiotic depending on the type of organism causing the infection. If an antibiotic is prescribed, it's important to complete the full course of antibiotics and not skip doses, even if symptoms go away.
-
2Manage any diarrhea.[24] The three major concerns with diarrhea are dehydration, nausea/vomiting, and fatigue. Get plenty of rest, and seek medical attention if any of these symptoms grows severe. You can also ask your doctor whether he recommends an over-the-counter anti-diarrheal like Imodium.[25]
- Caution: If you have a C. diff infection and use Imodium for more three days to try to stop diarrhea, you will be retaining dangerous toxins caused by C. diff which can seriously effect the kidneys, liver and intestines, etc.
-
3Avoid problem foods that might cause IBS flare-ups or worsen diarrhea. While diet is not the cause of colitis, certain foods can agitate your symptoms and make the condition worse. Foods that are rough on your stomach or intestines should be cut out of your diet as much as possible.[26] [27]
- Dairy can make symptoms dramatically worse, especially if you are lactose intolerant. When you do have dairy, take an enzyme product that can help break down the problematic lactose in dairy.
- Avoid high fiber foods (fruits and vegetables), or cook them to break down the fiber.
- Cut out gas-producing foods (carbonated drinks or caffeine), as well as fatty, greasy, or fried foods.
- Instead, eat digestible, bland foods like clear soup, crackers, toast, bananas, rice, and applesauce.[28] If you're actively vomiting, you should stick with clear liquids alone until you can hold them down.
-
4Eat small meals. Small meals are less likely to trigger your symptoms. Large meals, on the other hand, can overwhelm your digestive tract and cause a colitis flare-up. [29] [30] Switch from two or three large meals each day to five or six small ones. Give your digestive system a week or so to adjust, and continue on this schedule if it improves your symptoms. If not, you can probably switch back to your previous routine.
-
5Drink enough fluids. Hydration is important both for bacterial infection and IBD. The diarrhea from bacterial infection can dangerously dehydrate the body. If you have IBD, fluids ease the passage of waste through your intestines, causing less pain and fewer complications.[31] [32]
- Water is the best option. Try to drink six to eight 8-oz (250-ml) glasses of water daily to maximize your colon health.
- Avoid beverages that can dehydrate you, like those containing alcohol and caffeine. Caffeine also stimulates the intestines, often worsening symptoms in the process. Carbonated drinks can agitate symptoms by producing gas.
-
6Ask your doctor about multivitamin use. Colitis can make it difficult for your intestines to absorb enough nutrients, even if you eat a nutritious diet. A multivitamin might be able to supplement some of the vitamins and minerals your body's missing out on.[33] [34]
- While multivitamins might be able to help you supplement missing nutrients, do not rely on multivitamins instead of actual food and drink.
- Multivitamins do not provide your body with the protein and calories it needs to run.
-
7Reduce your stress. Stress can trigger colitis flare-ups, so you should take lengths to minimize it, though you can't cut it completely out of your life. Stress can make your stomach empty slowly and produce more acid than usual. It can also change the rate at which food passes through the intestines or affect intestinal tissue.[35]
- Mild to moderate exercise (jogging, cycling) can quickly and dramatically reduce your stress levels.
- You could also try yoga, meditation, or other exercises that ask you to focus on your breathing.
- If none of these options help or seem appealing, you could simply set aside a little time each day to do something you enjoy. That one simple action, in itself, can reduce your stress levels.
-
8Avoid medications that could cause flare-ups. Look at the side-effects for all your medications (including over-the-counter ones) to see whether they irritate the digestive tract or not. Avoid any over-the-counter medication that mentions stomach or intestinal irritation. Never stop taking a prescribed medication without first consulting your healthcare provider.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), in particular, have been known to cause flare-ups of colitis.[36]
-
9Try alternative treatments.[37] Probiotics are useful bacteria found naturally in the digestive tract. Getting more of them through yogurt or supplements can replace those lost through colitis, normalizing digestive health. The effectiveness of fish oil is debated — though a known anti-inflammatory, it's not been proven useful for intestinal inflammation. It could also loosen stools, and worsen colitis-induced diarrhea.
- Some evidence suggests that aloe vera might help as an anti-inflammatory, but the evidence is weak at best. Like fish oil, it's a known laxative.
- Acupuncture is used to treat a variety of conditions involving pain and inflammation. Always go to a licensed, rather than amateur, acupuncture specialist when trying this treatment.
- Turmeric has a compound called curcumin. When used in conjunction with other colitis therapies, some evidence suggests that this compound can improve symptoms.
Expert Q&A
-
QuestionIs colitis for life?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician Yes, you will be affected for life. You will have periods of waxing and waning symptoms over the course of your lifetime, though.
Yes, you will be affected for life. You will have periods of waxing and waning symptoms over the course of your lifetime, though.
Warnings
- It is always advisable to consult your doctor before beginning any treatment for colitis. A doctor can work with you to determine how severe your condition is, and together, the two of you can determine which treatment plan might be most beneficial for your specific set of circumstances.⧼thumbs_response⧽
References
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/001125.htm
- ↑ http://emedicine.medscape.com/article/927845-overview
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/001125.htm
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/001125.htm
- ↑ http://emedicine.medscape.com/article/927845-workup
- ↑ https://my.clevelandclinic.org/health/diseases/10351-ulcerative-colitis
- ↑ https://my.clevelandclinic.org/health/diseases/10351-ulcerative-colitis
- ↑ http://emedicine.medscape.com/article/927845-overview
- ↑ http://emedicine.medscape.com/article/927845-overview#a3
- ↑ https://medlineplus.gov/ency/article/000259.htm
- ↑ http://emedicine.medscape.com/article/927845-overview
- ↑ http://emedicine.medscape.com/article/179037-overview
- ↑ https://www.sparrow.org/departments-conditions/conditions/ischemic-colitis
- ↑ http://emedicine.medscape.com/article/977956-overview
- ↑ https://my.clevelandclinic.org/health/diseases/10351-ulcerative-colitis
- ↑ http://www.pharmacytimes.com/publications/issue/2011/july2011/irritated-about-your-irritable-bowels-confronting-ulcerative-colitis
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/002365.htm
- ↑ http://www.ccfa.org/what-are-crohns-and-colitis/what-is-ulcerative-colitis/colitis-medication.html
- ↑ https://www.uofmhealth.org/health-library/uf4785
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000250.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000254.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000121.htm
- ↑ http://reference.medscape.com/drug/imodium-k-pek-ii-loperamide-342041#91
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000249.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000250.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000122.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000249.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000250.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000249.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000250.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000249.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000250.htm
- ↑ https://my.clevelandclinic.org/health/diseases/10351-ulcerative-colitis
- ↑ http://www.medscape.com/viewarticle/752846
- ↑ https://ejmcm.com/article_5511_b847542af265a4f5cd57f0bf9964d751.pdf
About This Article
To cure colitis, first visit a doctor as soon as possible so they can run some tests and give you their recommendations for medicinal treatments. While waiting for medical attention, you can care for your colitis at home by drinking plenty of water to stay hydrated and help your colon health. You should also avoid foods that can make your symptoms worse, such as dairy, high fiber fruits and vegetables, carbonated drinks, and caffeine. For more help from our Medical co-author, including how to reduce your stress to minimize colitis flare-ups, read on!









































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...