This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
This article has been viewed 59,390 times.
If you’re experiencing moderate to severe pain—whether chronic or due to an injury or medical condition—you can ask your primary-care physician for a diagnosis and potentially, a pain medication. In some circumstances, doctors may be skeptical of your requests for pain meds if they think that you are abusing prescription medication or that you’re exaggerating the effects of your pain because many medications are highly addictive. To make a successful request, describe your pain on a 1–10 scale, be as specific as possible, and clarify if there are certain circumstances that cause the pain to increase or decrease.
Steps
Meeting with Your Doctor
-
1Schedule an appointment. If you are experiencing pain and cannot control it with over-the-counter medications, set up an appointment with your doctor at your earliest convenience. You’ll need to make the appointment by calling the doctor’s office main phone number and speaking with the receptionist.
- If you’re suffering from extreme or debilitating pain, or if your doctor’s office is not currently open, you may need to have a friend or family member take you to an emergency room or urgent care facility.
-
2Tell the doctor if you’re currently taking any over-the-counter or prescription pain meds. Your doctor will request this information if you ask for pain medication, even if you’re only requesting an extension of an existing prescription. Make sure you tell your doctor if you take any over-the-counter medication such as Tylenol or Ibuprofen, and whether or not these provide any relief. Mixing drugs can have harmful side effects, so it’s important to be thorough when relating which—if any—meds you currently take.[1]Advertisement
-
3Describe other activities done to relieve pain. When you’re asking your doctor for a pain medication, they may want to know if you have tried any non-medical means of alleviating pain, and if those methods have produced successful results.[2] If you’ve tried acupuncture, massages, yoga or Pilates, or any other non-medical pain-relief techniques, let your doctor know.
- Be aware that doctors will be less likely to prescribe a pain medication if the problem can be alleviated through other, non-medical means.
Describing the Pain
-
1Describe the location of the pain as specifically as possible. Your doctor will not be able to diagnose your pain, understand the root of the symptoms, or prescribe an effective pain medication if your descriptions are vague. Tell your doctor exactly where on your body you experience the pain, and if the pain travels or moves from one location to another, be precise about that as well.[3] For example:
- Rather than saying, “My back hurts,” say something like, “I feel pain between my shoulder blades, and sometimes a stabbing feeling shoots up my neck.”
- “My pain is all in my legs, but during the course of the day it moves from a sharp pain in my ankles to a more throbbing pain in my knees and hips.”
-
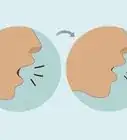
2Use precise language to convey how your pain feels. “Pain” itself is a fairly broad term; it can cover a tremendous variety of symptoms, from mild discomfort to tremendous suffering. To help your physician better understand your specific pain, use descriptive terminology. The better your doctor understands the experience of pain that you’re going through, the more accurately they’ll be able to prescribe a helpful pain medication. Your doctor will most likely only prescribe you pain medication if the source of your pain is consistent with an acute injury or a debilitating chronic medical condition that you suffer from, so make sure that you describe it clearly and accurately.[4] Use words like:
- “Dull” or “aching.”
- “Throbbing” or “pounding.”
- “Stabbing,” “sharp,” or “shooting.”
- “Burning” or “tingling.”
-
3Rate your pain on a 1–10 scale. Pain is an inherently subjective feeling, and it’s tough to communicate that to a doctor. To help your doctor understand the degree of the severity of your pain, describe pain using a 1–10 scale. 1 is a very mild pain (e.g. a slight sore throat) and 10 is a severe pain (e.g. the worse you’ve ever experienced.)[5] To communicate this to your doctor, say something like:
- When I first wake up, my neck pain is mild, maybe a 3. But by the time I’m going to bed it’s become much worse, maybe a 7 or 8.”
-
4Provide your doctor with your medical documents. Make sure to show your doctor any MRIs, X-rays, or other medical records that display important parts of your medical history. Especially if you’ve had a severe injury or condition, your doctor will be more inclined to prescribe pain medication. Whether you have a degenerative joint disease or an acute injury, your doctor will evaluate your potential need of pain medication and if so, what type on a case-by-case basis.
Conveying the Severity of Your Pain
-
1Explain the duration and frequency of your pain. This information will be helpful to your doctor as they try to diagnose the pain’s cause. Understanding the amount of time that your pain lasts for and how frequently it occurs will allow your doctor to prescribe the most effective pain medication. A brief, infrequent pain, likely has a different cause than a long-lasting, constant pain, even if both of the pains are similarly severe (e.g. both an 8).[6] Say something like:
- “The severe headaches never last for very long; maybe only about 15 or 20 minutes at a time. They happen three or four times per day, though.”
- “My pain in my hips is constant; I feel it throughout the day. There’s no point at which I’m not in serious pain.”
-
2State the psychological effect of your pain. It’s important for your physician to understand the ways in which your pain is hampering or worsening your daily life. This will increase a doctor’s likelihood of writing you an effective prescription for pain medication. If you find that your pain is interfering with your abilities to lead a normal life, or reduces your ability to perform daily functions, convey this to your physician.[7] Say something like:
- “The pain in my back has prevented me from being able to do some everyday activities that I never used to struggle with, like driving and working out.”
- “My pain is so intense that some days it’s not even worth getting out of bed.”
-
3Be careful not to develop a drug dependency. Part of the reason that doctors are often hesitant to prescribe pain medications is that the meds are potent and can be habit-forming. Users of opioid-based pain medications—such as hydrocodone (e.g. Vicodin) and oxycodone (e.g. OxyContin and Percocet)—are at an especially high risk for developing a dependency.[8]
- Even a prescription drug dependency can result in a potentially fatal overdose.
Warnings
- Narcotic analgesics are highly addicting, so first try to relieve your pain using other methods and/or types of medication.⧼thumbs_response⧽
References
- ↑ https://www.hss.edu/conditions_speaking-of-pain-how-to-help-your-doctor-help-you.asp
- ↑ http://www.caringinfo.org/i4a/pages/index.cfm?pageid=3509
- ↑ https://www.healthcentral.com/article/how-to-talk-to-your-doctor-about-your-pain
- ↑ http://www.cancer.net/blog/2014-10/talking-your-doctor-about-pain-management
- ↑ https://www.hss.edu/conditions_speaking-of-pain-how-to-help-your-doctor-help-you.asp
- ↑ https://www.hss.edu/conditions_speaking-of-pain-how-to-help-your-doctor-help-you.asp
- ↑ https://www.hss.edu/conditions_speaking-of-pain-how-to-help-your-doctor-help-you.asp
- ↑ http://www.philly.com/philly/blogs/health-cents/Talking-to-your-doctor-about-prescription-pain-medications.html











-Step-14-Version-2.webp)





















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...