This article was co-authored by Justin Barnes. Justin Barnes is a Senior Home Care Specialist and the Co-Owner of Presidio Home Care, a family-owned and operated Home Care Organization based in the Los Angeles, California metro area. Presidio Home Care, which provides non-medical supportive services, was the first agency in the state of California to become a licensed Home Care Organization. Justin has over 10 years of experience in the Home Care field. He has a BS in Technology and Operations Management from the California State Polytechnic University - Pomona.
There are 8 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 22,191 times.
Hospice focuses on patients with terminal illnesses living out their last days in comfort. Hospice care is recommended for patients who have received diagnoses of less than 6 months to live due to terminal illnesses, such as cancer or Alzheimer's.[1] Hospice is family-oriented, as the family stays involved in all aspects of decision-making and patient care, while a team of hospice caregivers attends to patient monitoring, medications, and therapy. If you or a loved one is facing a terminal illness, use these tips to learn how to arrange hospice care.
Steps
Determining Eligibility
-
1Watch for signs it may be time to move to hospice. A number of signs can point to the fact that it may be time for the patient to enter hospice care. For instance, the patient may stay in bed all the time, contract more infections, have more pain, and experience rapid weight loss. The patient may also be increasingly weaker, as well as needing to visit the hospital more often.[2] In addition, you may notice signs that your loved one is getting worse, despite still taking drugs to cure the disease.[3]
-
2Make sure the patient is ready for hospice care. Hospice is intended to make the patient's life more comfortable as they deal with a terminal illness. It's not intended to treat the disease the patient has, except for pain management. In other words, if the patient still wants to fight the disease through treatments like chemotherapy or a transplant, it's not time for hospice yet.[4]
- Keep in mind that hospice care doesn't provide interventions that prolong life, such as feeding tubes, unless the patient already has a feeding tube before entering hospice care.
- It can be difficult to have this conversation. You have to open it up with sensitivity and care. It can also be helpful for you to involve health care providers because they have lots of experience having this conversation. Plus, they know all about the benefits of hospice.
- If you choose to have the conversation alone, start by saying what kind of care hospice offers. You could say, "We may need to start thinking about hospice. Hospice covers pain management, medication coordination, and daily care. Just because you accept hospice doesn't mean you can't go back to treatment later.”
- You might also mention that Hospice workers are kind, caring, and experienced in all aspects
Advertisement -
3Have a doctor certify the patient for hospice care. To be in hospice care, particularly if the care needs to be covered by Medicare, the patient needs to be certified by a doctor. Generally, that means that the patient has a terminal illness and can't be reasonably expected to live more than 6 months.[5]
-
4Understand how payment works. You don't want to be worrying about money as someone's life draws to a close, but often, money can become an issue. Luckily, hospice is covered in full by Medicare, and it's also covered in part or in full by many major insurance companies.[6]
- However, if you aren't covered by Medicaid, Medicare, veteran's insurance like TRICARE, or private insurance usually cover hospice care. However, you may need to pay for hospice out of pocket if it is not covered. Many nonprofits will provide some relief for people who must pay out of pocket, such as paying on a sliding scale.[7]
- Though hospice is cheaper than hospital care, it can still be expensive, running as much as $600 or more per day, though it can be as little as $150 per day, depending on what services the patient is receiving. This amount is usually subsidized (partially covered) by your insurance company. However, you should still check with your provider to see what you might owe out-of-pocket.
Contacting a Hospice Center
-
1Contact a hospice center. If you're a family member, you can initiate contact with hospice. The patient or their doctor can also begin contact. With the initial contact, you will just be discussing what hospice entails. You're not committing to it yet.
- Usually, your doctor will recommend a hospice center. Generally, a nonprofit hospice is recommended. However, you can call any hospice center in your area that you feel is appropriate for you.
- You can also find local hospices through organizations like the American Cancer Society, United Way, or the Agency on Aging. These organizations often provide referrals to local hospices.
- Another way to pick a hospice is to ask friends and family for recommendations. Many people have been in the same place you have, and they can offer guidance about the agencies in town.
- Often, a hospice nurse will come to the hospital, house, or nursing home where the patient is staying at the time to discuss hospice care.
-
2Verify that your agency has the proper certifications. Your agency should be accredited through a national agency, such as the Joint Commission. In addition, it should be Medicare-approved, since that approval requires that the agency meet certain standards. Some states also require that the agency be licensed, which you can look up through your state.
- When meeting with the agency, you can ask about their accreditation, certification, and licensing, or you can look the information up online.
- Don't be afraid to go to another agency if you're not comfortable with what one is telling you. It is fine to shop around with other agencies to see what they offer, but keep in mind that all of the nurses will be through hospice.
- The Joint Commission is a national accrediting agency that provides accreditation for approximately 21,000 health organizations in the United States.[8]
-
3Ask questions. When you visit with the hospice worker, feel free to ask questions. That's why they are there. They want you and the patient to feel comfortable with the decision to go with hospice, so don't be afraid to put your fears out there. The hospice worker understands, and they are trained to be compassionate and caring.
- Ask about things like how soon care can be started (right away is best), what requirements the agency has for in-patient care, whether the patient can continue on certain treatments (such as dialysis), and exactly what kinds of care hospice provides for the patient.
- Also ask if the caregivers are on-call anytime (24 hours a day) and whether they personalize care plans for each patient. You can also ask about who will be providing care and what you'll be expected to do.
- If you don't get all your questions answered in the first meeting, you'll have a chance to talk again. Most hospice centers welcome calls, and many will send someone out to meet with you more than once.
-
4Learn what hospice covers. Hospice covers everything from care to equipment. They can provide nursing and doctor care. They can also provide equipment, such as hospital beds, wheelchairs, walkers, and bedside toilets, as well as supplies, such as catheters, bed pans, bed pads, and gloves. The patient will also be given medications appropriate for palliative care, such as pain medications, and will also be provided with nursing aid care, such as showering or bathing several times a week.[9]
- Other services may include diabetes counseling, physical therapy, spiritual guidance (from a chaplain), and nutritional advice.
- For the family, hospice can provide short-term and long-term respite care, meaning hospice can care for the patient 24-hours a day for a period (usually up to 5 days) if the primary caregiver needs a break.
- Keep in mind that hospice covers in home care and hospital care as needed. A hospice nurse will visit the patient at home, and the nurse may also recommend that the patience be admitted to the hospital.
- Hospice does not cover medications intended to cure the disease rather than manage pain.
-
5Don't be afraid to say "yes." Hospice sounds scary because it may seem like you're giving up on the person's care. However, if the person has a terminal illness, hospice can provide care to make the person more comfortable, meaning the end of the person's life will be better. Plus, hospice can provide a wide variety of care that helps relieve you and other people in charge of the person's care, so that you can focus on being with the person rather than caring for the person.
-
6Make the decision, if you need to do so. If you're the person's medical power of attorney, it may fall to you to make the decision for hospice. Often in the final days of an illness, the person becomes confused and unable to make informed decisions, which is why they named a person they trusted to make the decision for them (you, possibly). In that case, you may need to decide that the person needs to enter hospice care, and legally, you have the right to do so.
Opening the Door to Hospice Care
-
1Be ready for hospice to enter the home. Most hospice care is done in the patient's home or nursing home. Therefore, you need to be ready to have people in the patient's home at all hours of the day, though most care will be provided during the day.[10] While in some cases, the patient may be moved to an in-patient hospice center, one of the benefits of hospice care is it can be done in the comfort of the patient's own home.
- Basically, all you need to get ready is to make space available for what hospice will bring in, such as a hospital bed.
- The patient doesn't need to be home-bound to receive hospice care. In other words, the patient can still receive hospice care even if they are still able to get out and about.
-
2Continue seeing the patient's doctor. Most of the time, the doctor that is already caring for the patient becomes part of the hospice team. Therefore, you don't need to worry about switching to a new doctor at this difficult time. The patient will be able to have someone they know and trust on the team.
-
3Let hospice coordinate care. One of the benefits of having hospice care is that they will coordinate the patient's care. In other words, they will give information to the parties that need it, including the pharmacy and the patient's doctor, so you don't have to. You can focus on being with the person.
- The hospice team will be composed of many members, which can include a registered nurse, doctors, nursing aids, therapists, nutritionists, social workers, and trained volunteers, all ready to help provide care to your loved one.
- When the time does come, the team will also assist with connecting you to the funeral home of your choice, and they can do so at any time to help you make arrangements.
-
4Don't be afraid to call. Hospice is meant to be there for you when you need it, even in the middle of the night. If something is happening with the patient, call hospice for help. They can either reassure you or send someone out to check on the patient.[11]
-
5Prepare for the fact that the patient won't return to the hospital. While it is a benefit for the patient to be in their own homes, generally the patient will not return to hospital for any care. You will find hospice will make exceptions for injuries not related to the illness, such as the patient falling and cutting themselves, where stitches are required. However, the patient usually doesn't return to the hospital for care related to the terminal illness, though it does depend on the patient and the hospice program.
- When the patient needs to go to the hospital for something non-illness related, you usually need to inform hospice of what is happening.
-
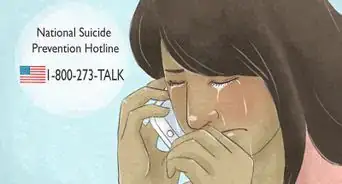
6Accept the help that hospice offers the family. Hospice care of course provides relief for friends and family member by assisting with care. However, hospice also provides other services for friends and family, such as having regular meetings to keep family updated, as well as bereavement care when the patient finally passes.
-
7End hospice care if you feel it's appropriate. Once you commit to hospice care, you and the patient are saying that you just want palliative care, not curative care, meaning you're not looking to cure the patient's disease. However, you can stop hospice care at any point if the patient or a family member decides that they want to pursue cures again. Therefore, you are able to change your mind if new information comes to light.
- However, the person cannot be pushed off hospice by the provider or by Medicare. Once the person is in hospice, they'll remain, even if they live beyond the "6 months" certified by the doctor.
References
- ↑ https://www.cancer.org/treatment/end-of-life-care/hospice-care/what-is-hospice-care.html
- ↑ Justin Barnes. Senior Home Care Specialist. Expert Interview. 6 March 2020.
- ↑ https://www.nia.nih.gov/health/what-are-palliative-care-and-hospice-care
- ↑ https://www.cancer.org/treatment/end-of-life-care/hospice-care/what-is-hospice-care.html
- ↑ https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/Hospice
- ↑ https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/Hospice
- ↑ https://www.mcleodhealth.org/services/care/hospice-overview/paying-for-hospice/
- ↑ https://www.jointcommission.org/about_us/about_the_joint_commission_main.aspx
- ↑ https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c09.pdf
- ↑ Justin Barnes. Senior Home Care Specialist. Expert Interview. 6 March 2020.
- ↑ https://hospicefoundation.org/hfa/media/Files/8-5x11_booklet_Hospice_Cagle_Sept1.pdf




































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...