This article was co-authored by Trudi Griffin, LPC, MS. Trudi Griffin is a Licensed Professional Counselor in Wisconsin specializing in Addictions and Mental Health. She provides therapy to people who struggle with addictions, mental health, and trauma in community health settings and private practice. She received her MS in Clinical Mental Health Counseling from Marquette University in 2011.
There are 7 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 36,399 times.
The Beck Depression Inventory (BDI) was published in 1996 and is a reliable self-report inventory used to evaluate the symptoms of depression.[1] It is a short inventory that can easily be administered in 10 to 15 minutes. The items are easy to understand and rate, and the scoring procedure is very simple. By taking and then periodically retaking the BDI, you can not only evaluate your depression but track its progress and the success of any treatment, including making note of particular areas (insomnia, etc.) that may not be responding to your current treatment.[2]
Steps
Setting Up the Test
-
1Familiarize yourself with the Beck Depression Inventory. There is a lot of information online about the administration and scoring of the Beck Depression Inventory. It's a good idea to do some online research before you begin. Here is some valuable information about the inventory:[3]
- It is a 21 item self-report inventory.
- It is used to evaluate depression in both clinical and non-clinical patients.
- It was developed to be administered on adolescents and adults, so it can be used by anyone 13 and above.
- It uses a rating tool where each item is rated on a four point scale from 0-3.
- 0 means you are experiencing no symptoms, while 3 means you are experiencing a severe form of the symptoms.
- The inventory has been translated into various languages.
-
2Read the test items carefully. In order to use this tool for self-administration or to administer it to someone else, you should first read all of the items carefully along with the instructions.
- For example, a question may ask you to respond by circling the response that most accurately describes you, such as
- 0: I do not feel sad
- 1: I feel sad some of the time
- 2: I am sad all the time
- 3: I am so sad or unhappy that I can’t stand.[4]
Advertisement - For example, a question may ask you to respond by circling the response that most accurately describes you, such as
-
3Get acquainted with the administration procedure. This is very important for administering the inventory.
- First of all, you have to rate the items based on your condition during the past two weeks as well as they day you administer the test.
- If you feel that multiple statements describe your condition equally, choose the response with the higher number on the 0-3 scale. For example if you think 2 and 3 are equally representative of your condition, choose statement 3.[5]
- Lastly, item 16 (changes in sleeping pattern) and item 18 (changes in appetite) are rated on a seven-point scale instead of the normal four-point scale. However, these items are not given any more weight than the others when calculating your results.[6]
-
4Try to administer the test in a distraction-free environment. When you take or administer the test, make sure to do it in a quiet room. You should give the test your undivided attention. Take care of any needs (bathroom, snack, etc.) before the test.
- Give yourself ample time to complete the test--don’t rush through it.
- Take it when you feel well enough to concentrate on your responses. Don’t take the test if you’re distracted by a headache or stomach ache, etc.
Administering and Scoring the Test
-
1Try to answer as accurately as you can. Carefully read each question and make sure you understand what’s being asked. Always try to give the answer that most closely matches your condition over the past two weeks.[7]
- Because you can only choose a single item out of four statements, try to judge your emotions, feelings, or behaviors as precisely as possible.
-
2Score the items. Simply add up all the ratings to get your score. For example, if you have circled 0 on the first item and 3 on second, you’ll add them to get a score of 3 for the first two items.
- Proceed in the same manner for the rest of items until you have added the results for all 21 items.
- Note down your total score. It will fall in between the range of 0 to 63.
-
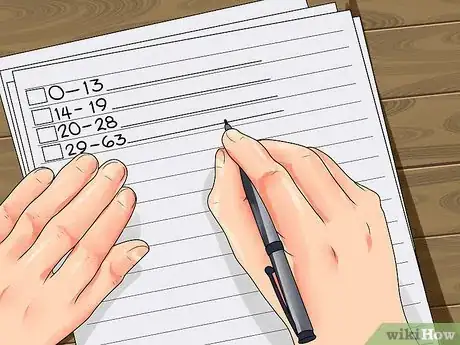
3Assess your score. There are no arbitrary cutoff points for diagnosing each category of depression. However, there are ranges of scores which indicate the particular category of depression a person is passing through. Once you have calculated your total score, simply compare your score with the following categories:[8]
- Score of 0 to 13: no depression
- Score of 14 to 19: mild depression
- Score of 20 to 28: moderate depression
- Score of 29 to 63: severe depression[9]
-
4Keep track of your depression. If you have previously been diagnosed with depression, the Beck Depression Inventory can be used on a weekly basis to check on your progress, especially if you have begun therapy and started taking medications.[10] This is very helpful for the following reasons:
- You can identify any changes in your emotional state.
- You can identify the areas where depression is still high, such as if you still have difficulty sleeping or have thoughts about suicide.
- Once you have identified the areas that are still causing a problem, you can start working to improve them with the help of your therapist.
- Regularly checking in with your progress helps to give you motivation for further change.
References
- ↑ http://www.minddisorders.com/A-Br/Beck-Depression-Inventory.html
- ↑ Beck Depression Inventory.(n.d).
- ↑ Beck Depression Inventory.(n.d).
- ↑ Osman,A., Downs,W.R., Barrios,F.X., Kopper,B.R.,Gutierrez, P.M.,& Chiros,C.E.(1997). Factor structure and psychometric characteristics of the beck depression inventory-II. Journal of Psychopathology and Behavioral Assessment, 19 (4), 359-376.
- ↑ Osman,A., Downs,W.R., Barrios,F.X., Kopper,B.R.,Gutierrez, P.M.,& Chiros,C.E.(1997). Factor structure and psychometric characteristics of the beck depression inventory-II. Journal of Psychopathology and Behavioral Assessment, 19 (4), 359-376.
- ↑ Osman,A., Downs,W.R., Barrios,F.X., Kopper,B.R.,Gutierrez, P.M.,& Chiros,C.E.(1997). Factor structure and psychometric characteristics of the beck depression inventory-II. Journal of Psychopathology and Behavioral Assessment, 19 (4), 359-376.
- ↑ Smarr ,K.L& Keefer,A.L.(2011). Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthritis Care & Research,63 (11), 454-456. doi: 10.1002/acr.20556.
- ↑ *http://www.nctsn.org/content/beck-depression-inventory-second-edition-bdi-ii
- ↑ Smarr ,K.L& Keefer,A.L.(2011). Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthritis Care & Research,63 (11), 454-456. doi: 10.1002/acr.20556.































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...