This article was medically reviewed by Mark Ziats, MD, PhD. Dr. Mark Ziats is an Internal Medicine Physician, Scientist, Entrepreneur, and the Medical Director of xBiotech. With over five years of experience, he specializes in biotechnology, genomics, and medical devices. He earned a Doctor of Medicine degree from Baylor College of Medicine, a Ph.D. in Genetics from the University of Cambridge, and a BS in Biochemistry and Chemistry from Clemson University. He also completed the INNoVATE Program in Biotechnology Entrepreneurship at The Johns Hopkins University - Carey Business School. Dr. Ziats is board certified by the American Board of Internal Medicine.
There are 33 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 72,743 times.
Dermatitis is a broad term used to describe skin conditions that cause inflammation and irritation. There are many different kinds of dermatitis, and they have a range of causes, from common allergic reactions to genetic disorders. Symptoms of dermatitis range from dryness and itching to severe, blistering rashes. The good news is that, in general, dermatitis can be treated and managed with over-the-counter medications and creams, good habits, and medications prescribed by your doctor.
Steps
Soothing Contact Dermatitis
-
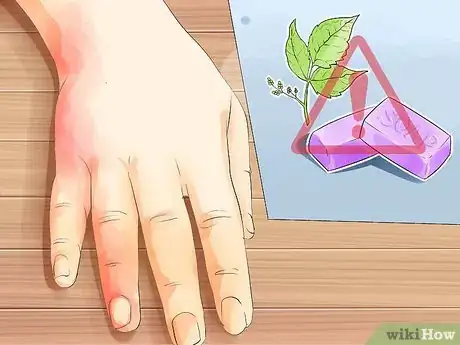
1Look for a localized, itchy and red rash to identify contact dermatitis. Contact dermatitis is one of the most common forms of dermatitis. This type of skin inflammation is caused by exposure to an allergen or irritant such as poison ivy or poison sumac. Signs of contact dermatitis include a localized rash, red patches and bumps, and localized itching. More severe symptoms include blisters and swelling. Usually, symptoms begin very soon after you’re exposed to the allergen or irritating substance.[1]
- Allergic contact dermatitis is a rash triggered even by brief contact with the allergen, and may take up to 2 weeks after exposure to develop. Examples include poison ivy and poison sumac, fragrances, plants, and materials that you may be allergic to.[2]
- Irritant contact dermatitis is dry, damaged skin caused by repeated rough exposure or exposure to harsh chemicals. It’s commonly caused by washing your hands too frequently, but harsh soaps, detergents, or industrial chemicals can also be at fault.
-
2Wash the affected area to remove any irritants. As soon as you notice a rash forming, rinse off your skin with lots of warm water to remove any irritants that may still be on the surface. Use a few drops of a gentle, unscented soap to avoid further irritation. Don’t scrub or rub too harshly or you could further aggravate your skin or potentially break the skin, which could lead to an infection.[3]Advertisement
-
3Avoid being exposed to the cause of your contact dermatitis. Identify the cause of your contact dermatitis so you can actively avoid being exposed to it. Cosmetics, perfumes, hair products, and metal jewelry are common causes of dermatitis, as are detergent, soap, or other household cleaning chemicals. Remove the cause of your exposure so you don’t have another outbreak.[4]
- If you don't know the exact cause of your dermatitis, avoid all harsh and scented products and metallic jewelry as much as possible or switch to gentler and fragrance-free alternatives.
Tip: If you are having trouble isolating the cause of your contact dermatitis, talk to your doctor about getting an allergy test, which will help you identify the exact cause so you can avoid it in the future.
-
4Use a barrier to protect yourself if you can’t avoid the irritants. If the cause of your dermatitis is a substance you work with or you can’t avoid being around it, a barrier can physically prevent the irritant from contacting your skin. Depending on the specific cause of your dermatitis, you can use different barriers such as:[5]
- Protective gloves or clothing
- Barrier creams
- Putting clear coats of nail polish on metal jewelry
-
5Take an oral antihistamine to reduce itching. If the itching is too severe for you to ignore, an over-the-counter antihistamine can help relieve it. Visit your local pharmacy and pick up a standard antihistamine that will reduce the itchiness and help prevent you from scratching at night.[6]
- Some antihistamines can make you drowsy.
-
6Apply moisturizer regularly to help your skin heal. Use fragrance-free, alcohol-free, and hypoallergenic moisturizer to keep your skin hydrated, which will help speed up the healing process. Apply the lotion by smoothing a large amount onto the skin in the direction your hair grows. Don’t rub the moisturizer in so it can moisturize the outer skin and create a protective layer to prevent dehydration.[7]
- Switch to a different moisturizer if you find it irritates your skin further. Be on the lookout for more symptoms, especially if you don’t know the cause of your contact dermatitis.
- Try using calamine lotion to help soothe your skin.[8]
-
7Take cool baths to soothe your skin. Painful, oozing lesions can be treated with lukewarm or cool baths. It won’t cure your dermatitis, but it can give you some temporary relief and soothe your skin so the symptoms are easier to deal with. Add 1/2 cup (90 g) of baking soda or colloidal oatmeal to the bath to make it extra soothing and calming on your skin.[9]
- If you don’t have time for a cool bath, apply a cool, wet compress to your skin for 15-30 minutes instead.
-
8Apply a topical corticosteroid cream for severe cases. If your condition does not improve with home remedies, apply a topical corticosteroid to the affected area to help reduce itchiness and inflammation. Visit your local pharmacy and pick up an over-the-counter hydrocortisone cream or contact your doctor and ask them to write a prescription for a stronger cream.[10]
- Apply the cream according the directions on the packaging.
- Don’t use a corticosteroid on an infant under 2 years of age. Pregnant women should apply with caution and use low-strength creams.
- Apply the ointment once a day, and do not continue for more than two weeks without doctor approval.
-
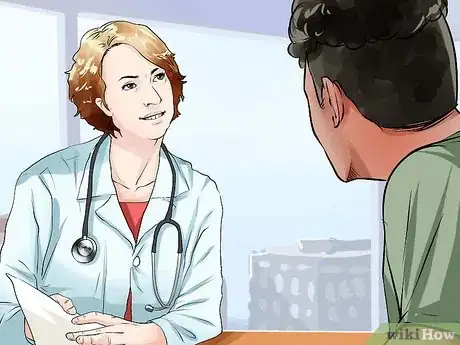
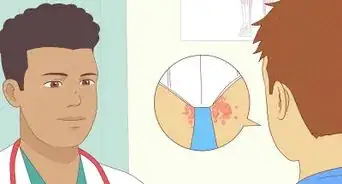
9See a dermatologist if symptoms persist for longer than 2 weeks. Contact dermatitis usually clears up within 1-2 weeks using home remedies, over-the-counter treatments, and avoiding the causes. However, if you still have a severe rash after 2 weeks, it could be a sign of a deeper issue. See a dermatologist so they can examine you and recommend strategies or prescribe medications that will treat your contact dermatitis.[11]
- A dermatologist can also prescribe stronger corticosteroids to calm inflammation or antibiotics to treat skin infections that may have developed.
- See your doctor if your dermatitis is affecting your sleeping, breathing, or work performance.
- If you experience a great deal of pain or you begin to develop infections or blisters on the affected area, contact your doctor.
Managing Eczema Symptoms
-
1Look for dry, scaly patches on your skin to identify eczema. Atopic dermatitis, or eczema, is a common skin condition that is caused by a combination of genetic and environmental factors. Symptoms of atopic dermatitis include intense itching, scaly patches on the elbows, knees, hands, and upper torso, small bumps that might ooze fluid, and swollen, sensitive skin. If you think you may have eczema, visit your doctor for an official diagnosis.[12]
- Many patients develop symptoms before age 5, and in many cases symptoms lessen or disappear in adulthood.
- If you or anyone in your genetic family has had similar rashes, asthma, or hay fever, then your chances of getting eczema are higher.
-
2Avoid allergens and irritants that trigger your symptoms. Atopic dermatitis can be aggravated by a number of things, so take note of allergens and irritants that trigger your symptoms or make them worse so you can actively avoid or minimize your contact with them. Your doctor can also conduct tests that will help you find the specific causes. A few common triggers of eczema include:[13]
- Perfumes, dyes, and cosmetics
- Dust, sand, and dust mites
- Chlorine, mineral oil, solvents, and other strong chemicals
- Animal fur or dander
- Cigarette smoke
- Pollen
- Food you or your doctor suspect you may be allergic to
- Excessive bathing without moisturizing
- Low humidity
- Emotional stress
- Your skin getting overheated[14]
-
3Wear cotton or other soft clothing. Wool and other rough material can exacerbate atopic dermatitis. Tight-fitting clothing or clothing that makes you sweat can also aggravate your eczema and make your symptoms worse. Choose loose-fitting clothing that also promotes air flow to your skin.[15]
Tip: Wash any fabrics that come into contact with the skin regularly using fragrance-free detergent. Dust mites can exacerbate eczema, so you want your clothing, towels, sheets, and pillows to be as clean and irritant-free as possible.
-
4Take a lukewarm bath or shower 2-3 times a week. Bathing, showering, or swimming more than 2–3 times a week can dry out your skin and trigger a rash. Avoid using hot water or any harsh or scented soaps and cleansers to keep your skin from drying out and your symptoms from getting worse.[16]
- Add soothing products to your bath such as uncooked oatmeal, colloidal oatmeal, or baking soda to help relieve your skin.
- Gently pat dry with a towel after bathing. Don't rub hard or vigorously or you’ll dry out your skin.
-
5Apply moisturizer to your skin daily to soothe your skin. Apply a moisturizing ointment or cream immediately after bathing, before bed, and throughout the day if necessary. Pay particular attention to your back, chest, and legs, as well as any other affected areas on your body. Choose an unscented moisturizer or ask your doctor for recommendations for soothing moisturizers that won’t aggravate your condition.[17]
- Use a low water content lotion, or a zero water content option such as petroleum jelly, which protect against water evaporation on your skin and have a lower chance of triggering a flare up.
-
6Use antihistamines or an anti-itch cream to help control scratching. Itching can be severe in atopic dermatitis cases, but scratching the affected patches of skin will make your condition worse and could lead to skin infections. An over-the-counter oral antihistamine can help reduce the itchiness. You could also apply a topical anti-itch cream or a hydrocortisone cream directly to your patches of atopic dermatitis to control the itchiness.[18]
- Cut your fingernails short to minimize damage from scratching.
- Wear gloves at night if you scratch yourself while sleeping.
-
7Keep yourself cool to prevent sweating. Sweating can irritate your skin and aggravate your atopic dermatitis. If your room gets too cold at night, set your thermostat to a comfortable temperature and use a humidifier to keep the dry air from drying out your skin.[19]
-
8Find ways to reduce your stress to prevent outbreaks. Stress and anxiety will make the symptoms of your atopic dermatitis more severe and can cause additional outbreaks or flare ups. Identify the stressors in your life so you can avoid them or find ways to manage them. If you’re struggling with stress and anxiety, visit a licensed therapist to help identify the underlying causes. They may also prescribe medication that can help you manage your stress.[20]
- Some ways you can help manage your stress include regular exercise, talk therapy, meditation, or deep breathing exercises.
-
9Talk to a dermatologist about prescription-strength treatments. Severe cases of eczema may require more serious medical intervention to relieve your symptoms. There are a variety of therapies and medications that can treat serious cases of eczema, and your doctor can help determine what the best course of treatment is for you. If you’re unable to treat or manage your symptoms on your own, make an appointment to see your doctor.[21]
- A prescription-strength orticosteroid cream can be used for severe cases to reduce inflammation and scaling.
- Oral antibiotics can help treat skin infections as well as reduce the skin bacteria that can worsen atopic dermatitis.
- UV Phototherapy can help treat atopic dermatitis.
- A combination of moisturizers and corticosteroids can be applied to the skin using wrapped bandages.
Relieving the Symptoms of Seborrheic Dermatitis
-
1Check for yellow or reddish scaling on the scalp, face, or genitals. Also called "cradle cap" in infants, seborrheic dermatitis causes greasy yellowish or reddish scaling, most commonly on the scalp, face, or genitals. On your face, it’s usually found around the eyebrows or the sides of your nose. The most common symptoms are flaking or dandruff on the scalp and eyebrows, scaly and red skin, itchiness, and crusty eyelids.[22]
-
2Use over-the-counter antidandruff shampoo to wash your scalp. Especially for mild cases, an over-the-counter anti-dandruff shampoo is often sufficient to relieve the symptoms of seborrheic dermatitis. Choose a dandruff shampoo with ingredients such as pyrithione zinc, tar, selenium, ketoconazole, or salicylic acid to help remove scaly patches and dandruff.[23]
- Depending on the type of shampoo you use, you can shampoo between 2-7 times per week.
- Leave the shampoo on your hair for the recommended amount of time on the bottle.
- Alternate shampoos to find the most effective one for you.
Tip: If you have a beard or other form a facial hair, and you have seborrheic dermatitis on the skin beneath it, use a dandruff shampoo to treat it. You don’t have to shave![24]
-
3Avoid skin products that contain alcohol. Skin cleansers, aftershaves, cosmetics, and fragrances that contain alcohol can aggravate your seborrheic dermatitis and make your symptoms worse. Look for hypoallergenic products that are unscented, alcohol-free, and suitable for sensitive skin.[25]
-
4Talk to your doctor if your symptoms don’t improve after 2 weeks. Most cases of seborrheic dermatitis can be treated with over-the-counter methods and will generally clear up after a week or so. However, more severe cases might require more serious medical intervention. Talk to your doctor about treatments or medications they can prescribe to help treat your symptoms. Some of these treatments might include:[26]
- Prescription-strength corticosteroids
- Antifungal shampoos, creams, and oral medications
- Antibacterial gels and creams
- Light therapy
- Immune system suppressants
Preventing Outbreaks of Nummular Dermatitis
-
1Look for coin-sized red spots to identify nummular dermatitis. Also known as discoid eczema, nummular dermatitis is characterized by circular, coin-sized red plaques. They’re often found on the legs, arms, hands, or torso. The red discs tend to be 1–4 inches (2.5–10.2 cm) in diameter, and they can sometimes lead to blistering or leaking sores.[27]
- Men between the ages of 55-65 and women between the ages of 15-25 are the most commonly affected groups.
-
2Avoid the triggers of nummular dermatitis. Nummular dermatitis is a stubborn condition that can be caused by a number of possible environmental factors. Identify the potential causes and triggers of your condition so you can avoid or minimize your exposure to them. Common causes of nummular dermatitis include:[28]
- A cold, dry climate
- Insect bites and abrasions
- Metals, such as nickel
- Prescription medications such as interferon and isotretinoin
- Chemicals such as formaldehyde or chlorine
- Bacterial infection
- Poor circulation, especially in the legs
-
3Protect your skin from scrapes and harsh chemicals. Avoid scratching and rubbing your skin and wear protection if you play contact sports that could cause an abrasion. Don’t expose your skin to strong cleansers or chemicals such as bleach so you don’t irritate it or cause a potential infection.[29]
Tip: If you have a scrape or patches of nummular dermatitis, avoid playing rough sports or strenous activity until your skin heals.
-
4Take a daily lukewarm bath or shower to soothe your skin. It’s important to keep your skin clean so your nummular dermatitis can clear up, but taking excessively long or hot baths or showers can irritate your skin. Bathing or showering for 20 minutes in lukewarm water will help your skin improve.[30]
- You can add 1/2 cup (40 g) of uncooked oatmeal or baking soda to the bath to help soothe your inflamed skin.
-
5Moisturize immediately after bathing to keep your skin hydrated. Apply a moisturizing cream, ointment, or lotion before drying off to hydrate the dry skin. Dry yourself with a clean towel by gentle patting, not rubbing. Add enough moisturizer so you skin is soft and well-hydrated.[31]
- A room humidifier can also help keep your skin moist.
-
6Ask a dermatologist about further treatment options. For extreme cases, a dermatologist can recommend prescription-strength treatment. Many of these treatments have side effects, so be sure that you consult a medical professional carefully about your options. These can include:[32]
- UV light therapy
- Topical and oral corticosteroids
- Wet dressings
Dealing with Stasis Dermatitis
-
1Check for skin changes on your legs to identify stasis dermatitis. Stasis dermatitis is caused by poor circulation in your lower legs and can cause swelling from the blood and fluid buildup. The swelling and fluid buildup causes pain and irritation in the skin on your legs. Common signs of stasis dermatitis include swollen ankles, feelings of heaviness or achiness in the leg, and skin changes such as hardening, bumpiness, thinness, itchiness, or darkening.[33]
- Stasis dermatitis is most commonly found in patients with congestive heart failure, varicose veins, or other circulation problems.
-
2Treat the underlying condition to get rid of stasis dermatitis. Because stasis dermatitis is caused by pooling blood and fluid in your legs, the only real way to treat and get rid of it is to address the underlying medical issue that is causing the fluid buildup. Talk to your doctor about procedures and medications that can help treat the causes of your poor blood circulation to improve the symptoms of your stasis dermatitis. Common strategies and treatments include:[34]
- Compression stockings
- Varicose vein surgery
- Avoiding long periods of standing or sitting
- Keeping your legs elevated while sleeping and every few hours while awake
-
3Talk to a dermatologist about safe skin medications you can use. You can use skin medications to help relieve your symptoms and improve the condition of your skin. But, some skin medications can negatively interact with other medications that you may be taking, so it’s important that you talk to your doctor before you try any new skin medications. They’ll be able to recommend the best options for you. Depending on your case, such treatments might include:[35]
Breaking the Itch-Scratch Cycle of Neurodermatitis
-
1Look for dry skin and a scratching compulsion to identify neurodermatitis. Neurodermatitis is a skin condition characterized by chronic itching and compulsive scratching and can be caused by stress or over-scratching an initial irritation, which now remains itchy due to the repeated scratching. The repeated scratching and picking at the same area can create thick, scaly skin that itches even more. Signs of neurodermatitis include patches of red, scaly, or leathery skin and the inability to prevent yourself from scratching the same spot on your body.[38]
-
2Take an oral antihistamine to help reduce itchiness. Reducing the amount that your skin itches can help you break the itch-scratch cycle that causes neurodermatitis. Pick up some over-the-counter antihistamines from your local pharmacy and take them as directed to get rid of the itch that compels you to scratch.[39]
- Topical hydrocortisone creams can provide a similar soothing effect.
-
3Wear soft cotton clothing to minimize irritation. Soft and comfortable clothes won’t make your skin itchy, which will help reduce your urge to scratch. Choose well-fitting cotton clothes that also allows your skin to breathe so you don’t sweat.[40]
-
4Protect your skin from overnight scratching. It can be hard to resist the urge to scratch the affected area when you’re asleep. Cut your fingernails short and wear gloves at night to prevent damage while sleeping. You can also bandage the area with a soft material to prevent you from scratching while you sleep.[41]
Tip: Getting restful sleep will also help your mental state, which can make it easier for you to control the urge to scratch. Make sure you get at least 7 hours of sleep every night.
-
5Keep the affected area well moisturized. Use moisturizing creams and lotions to keep your skin hydrated so it can heal and won’t be as painful or itchy. Add 1/2 cup (40 g) of uncooked oatmeal to your lukewarm baths to soothe and hydrate your skin. Moisturize your skin immediately after you bathe or shower.[42]
- Remember to pat yourself dry with a towel, don’t rub or abrade your skin further.
-
6Consult a physician about further treatment if your symptoms get worse. If you aren’t able to control your scratching and your skin is really inflamed or painful, talk to your doctor about other treatment options. They may be able to recommend strategies or medications you can use to relieve your symptoms and control your scratching. They can also refer you to a therapist who can help you manage your scratching. A few possible treatment options include:[43]
- Psychotherapy
- Stress-relief techniques or anti-anxiety treatments
- Corticosteroids
- Light therapy
- Botulinum (Botox) therapies
- Anti-inflammatories
Warnings
- If your skin shows signs of an infection, such as red streaks or pus oozing out of it, go to a doctor immediately.⧼thumbs_response⧽
- Follow all instructions for over-the-counter medications, shampoos, and treatments carefully. Don’t mix medications together without talking to a doctor first.⧼thumbs_response⧽
References
- ↑ https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-4362.1993.tb05022.x?sid=nlm%3Apubmed
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000869.htm
- ↑ https://pubmed.ncbi.nlm.nih.gov/27857991/
- ↑ https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1396-0296.2004.04031.x
- ↑ https://my.clevelandclinic.org/health/articles/4089-dermatitis
- ↑ https://my.clevelandclinic.org/health/articles/4089-dermatitis
- ↑ https://my.clevelandclinic.org/health/articles/4089-dermatitis
- ↑ https://www.drugs.com/mtm/calamine-topical.html
- ↑ https://my.clevelandclinic.org/health/articles/4089-dermatitis
- ↑ https://www.nhs.uk/conditions/contact-dermatitis/treatment/
- ↑ https://www.healthdirect.gov.au/contact-dermatitis
- ↑ https://pubmed.ncbi.nlm.nih.gov/24636644/
- ↑ https://pubmed.ncbi.nlm.nih.gov/28577805/
- ↑ https://www.ncbi.nlm.nih.gov/pubmed?term=16911274
- ↑ https://link.springer.com/article/10.1007/s11882-015-0518-0
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000853.htm
- ↑ https://pubmed.ncbi.nlm.nih.gov/29393034/
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000853.htm
- ↑ https://pubmed.ncbi.nlm.nih.gov/30082151/
- ↑ https://pubmed.ncbi.nlm.nih.gov/30665478/
- ↑ https://pubmed.ncbi.nlm.nih.gov/29121124/
- ↑ https://pubmed.ncbi.nlm.nih.gov/25822272/
- ↑ https://pubmed.ncbi.nlm.nih.gov/29410727/
- ↑ https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2133.1972.tb00312.x?sid=nlm%3Apubmed
- ↑ https://pubmed.ncbi.nlm.nih.gov/26051065/
- ↑ https://pubmed.ncbi.nlm.nih.gov/25822272/
- ↑ https://pubmed.ncbi.nlm.nih.gov/27399024/
- ↑ https://www.aad.org/public/diseases/eczema/types/nummular-dermatitis/causes
- ↑ link to correct page: https://www.aad.org/public/diseases/eczema/types/nummular-dermatitis/treatment
- ↑ https://www.aad.org/public/diseases/eczema/nummular-dermatitis
- ↑ https://pubmed.ncbi.nlm.nih.gov/29229630/
- ↑ link to correct page: https://www.aad.org/public/diseases/eczema/types/nummular-dermatitis/treatment
- ↑ https://pubmed.ncbi.nlm.nih.gov/28063094/
- ↑ https://pubmed.ncbi.nlm.nih.gov/28063094/
- ↑ https://pubmed.ncbi.nlm.nih.gov/28063094/?from_term=Stasis+Dermatitis+treatment&from_pos=1
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000834.htm
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000834.htm
- ↑ https://pubmed.ncbi.nlm.nih.gov/2928979/?from_term=neurodermatitis&from_page=3&from_pos=2
- ↑ https://pubmed.ncbi.nlm.nih.gov/1595516/
- ↑ https://pubmed.ncbi.nlm.nih.gov/28216719/
- ↑ https://pubmed.ncbi.nlm.nih.gov/28216719/
- ↑ https://pubmed.ncbi.nlm.nih.gov/28216719/
- ↑ https://pubmed.ncbi.nlm.nih.gov/2928979/
About This Article
To treat dermatitis, cover the affected area for 15 to 30 minutes with a cool, damp cloth to calm your irritated skin. You can also try taking an over-the-counter antihistamine, such as Benadryl, to help soothe the itching. For severe itching and inflammation, apply calamine lotion or a hydrocortisone cream to the affected area once a day. Additionally, use a fragrance free, hypoallergenic moisturizer after showering or bathing to protect your skin from further irritation. To learn more, like how to tell what type of dermatitis you have, scroll down!

























































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...