This article was co-authored by Rebecca Nguyen, MA. Rebecca Nguyen is a Certified Lactation Consultant and Childbirth Educator. She runs Family Picnic in Chicago, Illinois with her mother Sue Gottschall, where they teach new parents about childbirth, breastfeeding and child development and education. Rebecca taught preschool through 3rd grade for 10 years, and she received her Master’s Degree in Early Childhood Education from the University of Illinois in 2003.
This article has been viewed 43,647 times.
Relactation is the process of stimulating breastmilk production after you have stopped nursing for a period of time. There are many reasons for relactating, but regardless of your circumstances, understand that the process is not easy. Many mothers have success, but some do not.
Steps
Part One: Before You Begin
-
1Consider the time frame. Your odds of success mostly depend on how old your baby is and how long it's been since you initially stopped breastfeeding. Your genes will also determine how feasible relactating is.
- It is easiest to relactate if the process is started within three weeks after the birth of your baby. After that period, prolactin levels drop dramatically. You can still relactate after that window passes, but doing so can prove more difficult.
- Babies younger than three months are usually willing to resume breastfeeding, especially if they were breastfed previously. Between three and six months, individual temperament will determine how willing your baby will be. After six months, most babies will not be willing to return to breastfeeding.
-
2Contact a lactation consultant.[1] Contact the hospital you delivered through and ask to speak with a lactation consultant they have on staff there. If the hospital does not employ a lactation consultant, ask for a recommendation.
- You can also ask your midwife, your doctor, or your baby's doctor for a recommendation.
- Most of the tricks and techniques you can use to relactate are things you can try on your own, but a lactation consultant will usually be able to give you additional advice. This can be especially helpful if you are dealing with unusual circumstances.
Advertisement -
3Set aside at least two weeks. For two full weeks, your main concern should be breastfeeding and stimulating relactation. The entire process might take more time, but you need to keep it your primary focus for at least two weeks if you want to maximize your odds of success.
- Keep in mind that the amount of time it takes to relactate is usually equal to the amount of time that has passed since you stopped breastfeeding.
- Only 50 percent of mothers who successfully relactate establish a full supply within one month. The rest took longer, and some never produced a full supply.
-
4Build a base of support. You will need both emotional and professional help to make it through this difficult process.
- Turn to understanding family and friends for emotional support.
- If you know anyone who has successfully relactated, ask her for support and advice.
- Talk to your doctor, lactation consultant, and other related healthcare professionals for professional support.[2]
-
5Quit being so hard on yourself. Relactation is not easy and does not work for every woman who tries it. You can do everything right, and the process may still fail. Understand that it is not your fault and that failing to relactate does not, in any way, make you a bad mother.
Part Two: Stimulate Your Milk Supply
-
1Nurse your baby every two hours. The most important factor in relactation is physical stimulation. If your baby is willing to latch onto your breast and suck for at least two or three minutes, commit to nursing every two hours.[3] If possible, keep your baby at your breast for 20 to 30 minutes each time.
- Offer the breast as a pacifier before your milk comes in. The sucking motion can help stimulate your supply, so as long as your baby is willing, treating your breast as a pacifier can help speed the process along.
- Offer the breast before, after, and in between formula feedings, too. Do this regardless of how much formula your baby drinks.
- Switch sides. Offer your baby both breasts in equal intervals and for equal periods of time. Doing so stimulates equal milk production in both breasts and can prevent possible health problems.
-
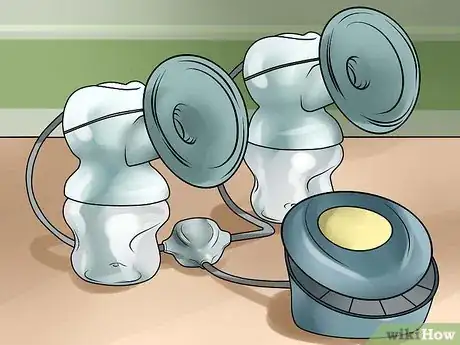
2Rent or buy an electric pump. You will probably need to stimulate milk production with a fully automatic electric pump kit, especially if your baby is initially unwilling to latch on.
- Double pumps are better than pumps that only work on one breast at a time.
- Since good electric pumps can be expensive, many mothers opt to rent them. Talk to a hospital, doctor, or lactation consultant about safe, trustworthy breast pump rental options available to you.
- Double pump eight times a day. Each session should last 10 to 15 minutes, no matter how much you are able to produce in that amount of time. Any stimulation is better than none.
-
3Take care of yourself. Drink plenty of water and get plenty of sleep throughout the entire process. Doing so will keep you healthy and will improve your chances of success.[4]
- You need to be fully hydrated if you want to produce sufficient breastmilk. Try to drink eight to ten 8-oz (250-ml) glasses of water daily.
- Sleep as much as possible and rest when sleep isn't possible. Your body will be less able to make the adjustments it needs to make if you are tired and running on empty.
-
4Use fenugreek.[5] Fenugreek belongs to a class of supplements known as galactagogues. Taking fenugreek on a regular basis is a safe, natural way to stimulate milk production. Among milk-stimulating supplements, it also has the highest rate of success.
- Fenugreek stimulates your sweat glands. The breast is actually a modified sweat gland, which is part of the reason why fenugreek is believed to be effective.
- Take two or three 500 mg fenugreek capsules up to three times daily. Most mothers see a notable increase in milk production within 24 to 72 hours of first use.
- Fenugreek tea is not as strong as pill supplements are and tends to be less effective.
-
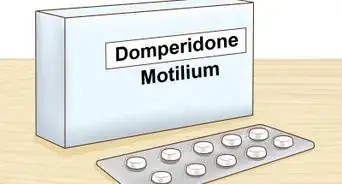
5Try galactagogue medication. If galactagogue supplements aren't strong enough, you can talk to your doctor about taking a prescription galactagogue medication like reglan or domperidone.[6]
- Domperidone has fewer side effects and is available in many countries, including Canada and Australia, but it is not available in the United States. If you are able to get a prescription for domperidone, you will need to take 10 mg three times a day. After taking it for a few weeks, this amount will be increased to 20 mg four times a day.
- Reglan should be taken three times a day in 10 mg doses. You'll need to decrease the dose gradually to avoid a dramatic drop in milk production. You should also note that taking it for four or more weeks can trigger or worse depression.
Part Three: Encourage Your Baby
-
1Choose the right time and place. Your baby may be more receptive to resuming breastfeeding if you set the right mood. As a general rule, the baby should feel comfortable and soothed.
- Do not wait until the baby is very hungry or very tired. Your baby should be relaxed, even to the point of falling asleep.
- Sit in a rocking chair placed in a dimly lit or dark room. Play soothing music. Keep the area free of distractions for both you and your baby.
-
2Stay calm and patient. Try not to stress out each time you sit with your baby to nurse. If your baby senses your stress, he or she will probably become stressed, too. A stressed baby will have very little interest in nursing.
- Keep the experience as pleasant as possible—for yourself and for your baby—so that your baby feels as though breastfeeding is a positive thing.
- Staying calm can also make the process easier for you to bear and may increase your odds of success.
-
3Increase touch. Some studies suggest that increasing the amount of physical contact between you and your baby can encourage your baby to accept breastfeeding while also stimulating your milk supply.
- Skin-to-skin contact is especially helpful.
- Spend more time cuddling and stroking your baby. Consider sleeping together or bathing together.
- Use a sling or a baby carrier to keep your baby close even when you aren't actively nursing.
-
4Apply milk to the nipple. If your baby still refuses to latch on, apply a little milk or formula to the nipple and areola. When your baby tastes it, he or she will identify the area as a source of food and may want to latch on.
- Before you produce any breastmilk, you can apply formula. After you've succeeded in stimulating some relactation, apply actual breastmilk to the area.
Part Four: Keep Your Baby Healthy
-
1Supplement with formula. While you work on building up your milk supply, you will need to continue feeding your baby formula. Do not cut back on the amount of formula you feed your baby until you begin relactating and your baby accepts it.
- Use bottles with slow flowing nipples. Liquid flows out of standard bottle nipples quickly, so your baby doesn't need to work very hard to eat. As a result, he or she can become more resistant to the idea of taking milk from the breast, which is more difficult to do.
-
2Consider using a supplemental nursing system. A supplemental system will deliver formula to your baby through a soft tube while your baby is nursing at the breast. As a result, your baby gets the food he or she needs while re-associating food with the breast instead of the bottle.
- Many babies are willing to work with these supplemental systems because each suck is rewarded with a steady flow of formula.
- You will need to wear a container of formula around your neck on a cord. Thin, soft tubes leading from this container will be inserted into your baby's mouth as he or she is at your breast. When your baby sucks, formula from these tubes will flow into his or her mouth.
- Note that you can use these systems with both formula and breastmilk.
- It is strongly recommended that you receive help from a lactation consultant before using this device since it can be difficult to maneuver at first. If used incorrectly, it can even hurt the baby's mouth.
-
3Gradually decrease the amount of formula. Once your baby begins to breastfeed well, you can start cutting back on the amount of formula he or she receives.
- Monitor your baby's weight during the entire process. If he or she is younger than four months, your baby must gain at least 1 oz (28 g) per day before you can safely cut back on formula supply.
- After your baby begins breastfeeding well, decrease the amount of formula by 1/2 fl oz (15 ml) in each bottle. Decrease by another 1/2 fl oz (15 ml) the following day. Repeat this pattern until you can eliminate or reduce supplemental formula feeding as much as possible without jeopardizing your baby's health.
Expert Q&A
-
QuestionWhat if my breast milk doesn't come back?
 Rebecca Nguyen, MARebecca Nguyen is a Certified Lactation Consultant and Childbirth Educator. She runs Family Picnic in Chicago, Illinois with her mother Sue Gottschall, where they teach new parents about childbirth, breastfeeding and child development and education. Rebecca taught preschool through 3rd grade for 10 years, and she received her Master’s Degree in Early Childhood Education from the University of Illinois in 2003.
Rebecca Nguyen, MARebecca Nguyen is a Certified Lactation Consultant and Childbirth Educator. She runs Family Picnic in Chicago, Illinois with her mother Sue Gottschall, where they teach new parents about childbirth, breastfeeding and child development and education. Rebecca taught preschool through 3rd grade for 10 years, and she received her Master’s Degree in Early Childhood Education from the University of Illinois in 2003.
International Board Certified Lactation Consultant Ultimately, you need to do what is best for your baby. If you cannot stimulate an ample enough supply of milk or if your baby remains unwilling, that's okay. The “right thing” is simply keeping your baby healthy and providing the nutrition he or she needs, regardless of whether that nutrition comes through breastmilk or formula.
Ultimately, you need to do what is best for your baby. If you cannot stimulate an ample enough supply of milk or if your baby remains unwilling, that's okay. The “right thing” is simply keeping your baby healthy and providing the nutrition he or she needs, regardless of whether that nutrition comes through breastmilk or formula.
References
- ↑ Rebecca Nguyen, MA. International Board Certified Lactation Consultant. Expert Interview. 10 June 2019.
- ↑ Rebecca Nguyen, MA. International Board Certified Lactation Consultant. Expert Interview. 10 June 2019.
- ↑ http://www.babycenter.com/404_how-do-i-breastfeed-once-my-milk-has-dried-up-relactation_8891.bc
- ↑ Rebecca Nguyen, MA. International Board Certified Lactation Consultant. Expert Interview. 10 June 2019.
- ↑ Rebecca Nguyen, MA. International Board Certified Lactation Consultant. Expert Interview. 10 June 2019.
- ↑ https://www.breastfeedingbasics.com/articles/relactation-and-adoptive-nursing