This article was co-authored by Mohammad Dar, MD. Dr. Mohammad Dar (MoDar) is a board certified Internist based in Boston, Massachusetts. With over seven years of experience in the medical field, he is skilled in epidemiology, healthcare, and health policy. Dr. Dar has had a myriad of experiences in healthcare, including working on the implementation of the Affordable Care Act at the White House Office of Health Reform, volunteering in rural Uganda with public health initiatives, and leading policy and on-the-ground COVID-19 operations during the pandemic. He has also worked on a number of innovative public health and insurance reform initiatives in Massachusetts. Dr. Dar received a BS in Cell and Molecular Biology and History from The University of Michigan and an MD from The University of Michigan Medical School. He completed his residency training at Harvard Medical School and Brigham and Women’s Hospital, from which he received the Golden Stethoscope Award.
There are 23 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 29,234 times.
Cortisol is often called the stress hormone, but it performs a range of vital functions. High levels of cortisol may contribute to Cushing syndrome, as well as other cortisol-related disorders like anxiety and depression. Very high levels of cortisol are most often caused by a tumor on your pituitary gland, long-term use of corticosteroid medications, or an adrenal gland disease. Your doctor will determine the cause of your high cortisol levels so they can prescribe an appropriate treatment to manage your condition.[1]
Steps
Taking Adrenal-Blocking Drugs
-
1Discuss treatment options for high cortisol with your doctor. High cortisol may result from pituitary or adrenal tumors or long-term use of corticosteroid medications, which can also worsen existing high cortisol levels. Surgery may be the recommended treatment for tumors, and it’s about 80 to 90% successful.[2] If surgery isn’t an option or effective, talk to your doctor about adrenal-blocking medications that stop your body from producing too much cortisol.[3]
- If you're having a tumor removed, you may also take adrenal-blocking drugs for a few weeks before surgery. For those with serious symptoms, such as severe high blood pressure or a weakened immune system, taking medication before surgery can lower the risk for complications.
- If you have a tumor that's in a hard to reach location or the risks of surgery outweigh the benefits, your doctor may not recommend surgery for you. If they decide surgery isn't an option, they'll usually recommend a long-term medication regimen to help manage your cortisol levels.
Cushing syndrome vs. Cushing disease: Cushing syndrome, or hypercortisolism, is the medical term for a collection of disorders related to high cortisol levels. Cushing disease is more specific and occurs when the pituitary gland tells the adrenal glands to make too much cortisol.[4]
-
2Talk to your doctor about metyrapone to treat acute, serious symptoms of high cortisol. The advantage of metyrapone is that it starts lowering cortisol levels within 2 hours. This makes it a good option for managing severe symptoms in the short-term. A typical starting dose is 250 mg 3 times per day, but doses of up to 8,000 mg per day are sometimes required.[5]
- Since it can cause cortisol levels to become too low, you’ll need to see your doctor for tests frequently while taking metyrapone.
- Side effects may include stomach pain, weight loss, and nausea. Tell your doctor if you experience side effects, as they may be a sign that your dose is too high.
- Metyrapone usually isn't prescribed for long-term management of high cortisol levels. Long-term use of this medication can lead to acne, potassium deficiency, high blood pressure, and unusual hair growth in women.[6]
Advertisement -
3Ask your doctor about ketoconazole for long-term management. Of the medications used to manage high cortisol levels due to Cushing syndrome, ketoconazole is the best-tolerated and most commonly prescribed. A typical regimen involves taking 400 to 1200 mg in 2 to 4 divided doses at around the same times each day.
-
4Consult your doctor about pasireotide for inoperable Cushing disease. Pasireotide makes the pituitary gland produce less of the hormone that tells the adrenal glands to make cortisol. Treatment involves either going to your doctor’s office for weekly injections or injecting yourself twice a day at home.[9]
- If you take injections at home, your doctor will show you exactly how to use your medication. Inject the pre-measured dose into your thigh, upper arm, stomach, or buttock. Choose a different injection site each time you use your medication to help prevent irritation.
- Side effects may include diarrhea, high blood sugar, abdominal pain, and fatigue; long-term use may lead to diabetes.
- Your doctor may also prescribe metyrapone or ketoconazole in combination with pasireotide.[10]
Managing High Cortisol Due to Corticosteroids
-
1Ask your doctor about non-steroid treatments for your condition. Corticosteroids are used to treat conditions such as asthma, arthritis, skin disorders, and lupus. If you take a corticosteroid and it’s raised your cortisol to unhealthy levels, consult your doctor about managing your condition with a non-steroid medication.[11]
- If a non-steroid alternative isn’t available, ask your doctor about delayed-release corticosteroids, which may lower the risk for harmful side effects. For instance, a delayed-release form of prednisone is now available for the management of rheumatoid arthritis.
- Even if you're able to switch medications, your doctor will need to gradually decrease your dosage amount to wean you off of the corticosteroid. Stopping a corticosteroid abruptly is not recommended.
-
2Take a lower dose of your corticosteroid, if possible. If you can’t switch medications, work with your doctor to determine the smallest dose you can take. Ask your doctor if lowering the dose is an option or if you can take your medication on alternating days.[12]
Safety Precaution: Don’t lower your dose or stop taking a corticosteroid or any other prescription medication without consulting your doctor. Stopping a corticosteroid suddenly can lead to symptoms of withdrawal and other harmful side effects.[13]
-
3Monitor your blood pressure, blood sugar, and bone density. If you can’t stop taking a corticosteroid, you’ll need to see your doctor for regular check-ups. They’ll need to check for potential health risks, such as high blood pressure, high cholesterol, and bone thinning.
Trying Natural Remedies
-
1Practice deep breathing techniques. Do breathing exercises regularly to keep your stress and cortisol levels in check. Close your eyes and inhale deeply as you count to 4, and fill your belly with air instead of raising your chest and shoulders. Hold your breath for a 7 count, then exhale slowly as you count to 8.[15]
- As you breathe slowly and deeply, imagine calming scenery. Picture yourself on a beach, in a tranquil field, or in a comfortable place from your childhood.
- Continue to control your breathing for 2 to 3 minutes, or until you start to feel more relaxed.
-
2Listen to relaxing music to reduce stress. Play soothing music with a slow beat, such as classical or ambient music. You can listen to music when you feel stressed, or make it a part of your daily routine.[16]
- You don’t have to be stressed out when you listen to music for it to have beneficial effects. Music can help keep cortisol levels from spiking in stressful situations hours after you’ve stopped listening.
-
3Try progressive muscle relaxation. To perform progressive muscle relaxation, contract the muscles in your toes, then release them. Exhale as you release, and imaging tension leaving your body.[17]
- After tensing and releasing your toes, contract and relax the muscles in your feet, calves, and thighs. Tense and relax one muscle group at a time, and work your way up until you’ve reached your head and neck.
- Do progressive muscle relaxation whenever you’re feeling stressed. It can also help you fall asleep, so try it when you hit the hay, too.
-
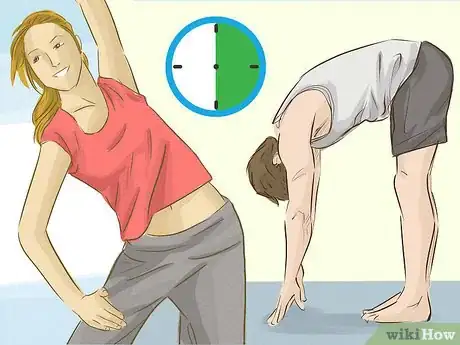
4Exercise for at least 30 minutes a day. In addition to being important for your overall health, regular exercise reduces cortisol and stress levels.[18] Try to walk, jog, or ride your bike for 30 minutes a day, 5 days a week. On the other 2 days, include strength training, such push-ups, crunches, pull-ups, and lifting free weights.[19]
Safety Precaution: Check with your doctor before starting a new exercise routine, especially if you’re not already physically active. Ask them for advice about safely becoming more active.
-
5Get at least 7 to 9 hours of sleep each night.[20] Lack of sleep can raise cortisol levels and increase stress. To develop healthy sleeping habits, try to go to bed and wake up at the same time every day. Set aside 1 to 2 hours before bed to relax, and keep your bedroom cool, dark, and comfortable.[21]
- Avoid looking at electronic screens before bed, since they produce blue light and trick your brain into thinking it’s daytime. If you need to use your phone, tablet, or computer, download a filter app that blocks out blue light.
- Avoid drinking caffeine later than 2 p.m., and try not to have a heavy meal within 3 to 4 hours of going to bed.
-
6Maintain a healthy, balanced diet.[22] Fill half of your plate with fruits and veggies, go for whole grains, and choose lean proteins, such as seafood and white meat poultry. Include foods in your diet that can lower cortisol levels, such as avocados, blueberries, salmon, and unsalted nuts.[23]
- Limit your intake of salt, added sugars, and trans fats, which can each increase cortisol. Items to limit or avoid include processed meats (such as bacon and deli meats), soft drinks and other sweetened beverages, fatty cuts of red meat, and fried foods.
- Avoid skipping meals and low-calorie diets, which can raise cortisol levels. Make sure you’re consuming enough calories per day to meet your daily needs. Learn more about your specific nutritional requirements at https://www.choosemyplate.gov.
-
7Set limits and learn how to say no. If you're starting to get overwhelmed, do your best to stop taking on new responsibilities. Ask for help when possible to avoid getting stressed. If you’re anxious about saying no to someone, remind yourself that watching out for your well-being is your top priority.[24]
- Set limits whenever possible by saying, “I’d love to volunteer, but this month is crazy for me,” “Thanks for the invitation! I’d love to go, but my schedule is packed,” or “The ABC account is taking up all of my time. Unless you want me to reprioritize, I can’t take on a new project this week.”
- Whether you have kids or are busy at work, you can’t take care of others or do your best work if you’re burned out.
-
8Talk to your doctor about taking an herbal supplement for stress. Consult your doctor before taking an herb or supplement. Tell them about any medications you take, and ask them to recommend a dosage regimen. There’s evidence some herbal supplements may safely lower cortisol and reduce stress, but most medical professionals recommend against long-term use.[25]
- Valerian and chamomile may lower cortisol, reduce stress, and make it easier to fall asleep. There are no expert-approved dosage amounts, but a typical daily dose is 400 mg to 1,400 mg. When in doubt, start at a low dose to see how a supplement affects you.
- Taking a 300 mg capsule of Ashwagandha root 1 to 2 times per day may also lower stress and anxiety.[26]
- Green, black, and oolong teas contain a compound called L-theanine, which may lower cortisol levels. Additionally, relaxing with a hot cup of caffeine-free tea at night may help you de-stress after a long day.[27]
Expert Q&A
-
QuestionWhat lowers cortisol overnight?
 Mohammad Dar, MDDr. Mohammad Dar (MoDar) is a board certified Internist based in Boston, Massachusetts. With over seven years of experience in the medical field, he is skilled in epidemiology, healthcare, and health policy. Dr. Dar has had a myriad of experiences in healthcare, including working on the implementation of the Affordable Care Act at the White House Office of Health Reform, volunteering in rural Uganda with public health initiatives, and leading policy and on-the-ground COVID-19 operations during the pandemic. He has also worked on a number of innovative public health and insurance reform initiatives in Massachusetts. Dr. Dar received a BS in Cell and Molecular Biology and History from The University of Michigan and an MD from The University of Michigan Medical School. He completed his residency training at Harvard Medical School and Brigham and Women’s Hospital, from which he received the Golden Stethoscope Award.
Mohammad Dar, MDDr. Mohammad Dar (MoDar) is a board certified Internist based in Boston, Massachusetts. With over seven years of experience in the medical field, he is skilled in epidemiology, healthcare, and health policy. Dr. Dar has had a myriad of experiences in healthcare, including working on the implementation of the Affordable Care Act at the White House Office of Health Reform, volunteering in rural Uganda with public health initiatives, and leading policy and on-the-ground COVID-19 operations during the pandemic. He has also worked on a number of innovative public health and insurance reform initiatives in Massachusetts. Dr. Dar received a BS in Cell and Molecular Biology and History from The University of Michigan and an MD from The University of Michigan Medical School. He completed his residency training at Harvard Medical School and Brigham and Women’s Hospital, from which he received the Golden Stethoscope Award.
Board Certified Internist & Health Policy Director Try your best to lower cortisol through consistent healthy living. It's not medically safe to deploy cortisol-controlling medications for people without true issues in how their adrenal production works. Make changes in your lifestyle and talk to your primary care doctor about your symptoms. The professional then can decide if testing by a specialist is merited to look for an issue.
Try your best to lower cortisol through consistent healthy living. It's not medically safe to deploy cortisol-controlling medications for people without true issues in how their adrenal production works. Make changes in your lifestyle and talk to your primary care doctor about your symptoms. The professional then can decide if testing by a specialist is merited to look for an issue. -
QuestionHow do you know if your cortisol levels are high?
 Mohammad Dar, MDDr. Mohammad Dar (MoDar) is a board certified Internist based in Boston, Massachusetts. With over seven years of experience in the medical field, he is skilled in epidemiology, healthcare, and health policy. Dr. Dar has had a myriad of experiences in healthcare, including working on the implementation of the Affordable Care Act at the White House Office of Health Reform, volunteering in rural Uganda with public health initiatives, and leading policy and on-the-ground COVID-19 operations during the pandemic. He has also worked on a number of innovative public health and insurance reform initiatives in Massachusetts. Dr. Dar received a BS in Cell and Molecular Biology and History from The University of Michigan and an MD from The University of Michigan Medical School. He completed his residency training at Harvard Medical School and Brigham and Women’s Hospital, from which he received the Golden Stethoscope Award.
Mohammad Dar, MDDr. Mohammad Dar (MoDar) is a board certified Internist based in Boston, Massachusetts. With over seven years of experience in the medical field, he is skilled in epidemiology, healthcare, and health policy. Dr. Dar has had a myriad of experiences in healthcare, including working on the implementation of the Affordable Care Act at the White House Office of Health Reform, volunteering in rural Uganda with public health initiatives, and leading policy and on-the-ground COVID-19 operations during the pandemic. He has also worked on a number of innovative public health and insurance reform initiatives in Massachusetts. Dr. Dar received a BS in Cell and Molecular Biology and History from The University of Michigan and an MD from The University of Michigan Medical School. He completed his residency training at Harvard Medical School and Brigham and Women’s Hospital, from which he received the Golden Stethoscope Award.
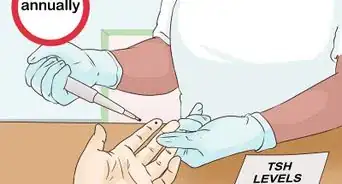
Board Certified Internist & Health Policy Director Cortisol tests are usually done by a specialist like an Endocrinologist, rather than by a primary care doctor. This is because the tests might need to be done at different times of day, might require sampling over 24 hours, etc. to gather the data needed to determine if you have a true medical issue where your body is making too much or too little cortisol and which would require medications.
Cortisol tests are usually done by a specialist like an Endocrinologist, rather than by a primary care doctor. This is because the tests might need to be done at different times of day, might require sampling over 24 hours, etc. to gather the data needed to determine if you have a true medical issue where your body is making too much or too little cortisol and which would require medications.
Warnings
- Take any medication according to your prescriber’s instructions. Don’t stop taking a medication without consulting your healthcare provider.[31]⧼thumbs_response⧽
- Consult your doctor before trying a supplement, especially if you take blood thinners or other prescription medications. Supplements may change how medications work or lead to unwanted side effects.[32]⧼thumbs_response⧽
- Steer clear of over-the-counter cortisol blockers that promise to reduce stress or promote weight loss. There’s insufficient research to back their claims or verify their safety.[33]⧼thumbs_response⧽
- For most people, controlling cortisol levels is less about finding a medication to regulate it and more about taking care of your body through habits of healthy living.[34]⧼thumbs_response⧽
References
- ↑ https://www.mayoclinic.org/diseases-conditions/cushing-syndrome/symptoms-causes/syc-20351310
- ↑ https://www.mayoclinic.org/diseases-conditions/cushing-syndrome/diagnosis-treatment/drc-20351314
- ↑ Mohammad Dar, MD. Board Certified Internist & Health Policy Director. Expert Interview. Friday, September 3, 2021.
- ↑ https://medlineplus.gov/ency/article/000410.htm
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3683198/
- ↑ https://www.karger.com/Article/FullText/314292
- ↑ https://medlineplus.gov/druginfo/meds/a682816.html
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3683198/
- ↑ https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/200677lbl.pdf
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3683198/
- ↑ Mohammad Dar, MD. Board Certified Internist & Health Policy Director. Expert Interview. Friday, September 3, 2021.
- ↑ https://www.hormone.org/diseases-and-conditions/adrenal/cushing-syndrome
- ↑ https://www.mayoclinic.org/diseases-conditions/cushing-syndrome/diagnosis-treatment/drc-20351314
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2872100/
- ↑ https://medlineplus.gov/ency/patientinstructions/000874.htm
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3734071/
- ↑ https://medlineplus.gov/ency/patientinstructions/000874.htm
- ↑ Mohammad Dar, MD. Board Certified Internist & Health Policy Director. Expert Interview. 3 September 2021.
- ↑ https://www.health.harvard.edu/staying-healthy/exercising-to-relax
- ↑ Mohammad Dar, MD. Board Certified Internist & Health Policy Director. Expert Interview. 3 September 2021.
- ↑ https://medlineplus.gov/ency/article/001942.htm
- ↑ Mohammad Dar, MD. Board Certified Internist & Health Policy Director. Expert Interview. 3 September 2021.
- ↑ https://my.clevelandclinic.org/health/transcripts/1458_stress-busting-foods
- ↑ https://medlineplus.gov/ency/article/001942.htm
- ↑ https://www.mayoclinic.org/diseases-conditions/generalized-anxiety-disorder/expert-answers/herbal-treatment-for-anxiety/faq-20057945
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3573577/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4728665/
- ↑ https://medlineplus.gov/ency/article/000348.htm
- ↑ https://medlineplus.gov/ency/article/001942.htm
- ↑ https://www.nimh.nih.gov/health/publications/stress/index.shtml
- ↑ https://www.nimh.nih.gov/health/topics/mental-health-medications/index.shtml
- ↑ https://www.mayoclinic.org/diseases-conditions/generalized-anxiety-disorder/expert-answers/herbal-treatment-for-anxiety/faq-20057945
- ↑ https://www.mayoclinic.org/healthy-lifestyle/weight-loss/expert-answers/cortisol-blockers/faq-20058132
- ↑ Mohammad Dar, MD. Board Certified Internist & Health Policy Director. Expert Interview. 3 September 2021.
























-Step-12-Version-2.webp)














































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...