This article was co-authored by Chris M. Matsko, MD. Dr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
There are 19 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 52,888 times.
Leptospirosis is an infection caused by bacterial spirochetes that affects humans and animals.[1] While for many people and animals the infection will be mild and have no real impact on long term health, for others the infection can become severe and life-threatening. Symptoms can look like symptoms of several other illnesses, such as the flu. When assessing symptoms that may be signs of infection, you need to take into consideration your recent activities and the possible risk of exposure.[2]
Steps
Watching for Symptoms of Exposure
-
1Don’t mistake symptoms for flu. Symptoms of leptospirosis can vary and can look like symptoms associated with other infections or illnesses. If you develop flu-like symptoms suddenly, don’t assume it is flu if there is the possibility of exposure.[3]
- Leptospirosis generally presents with flu-like symptoms including fever, myalgia, rigor, and headache.[4]
-
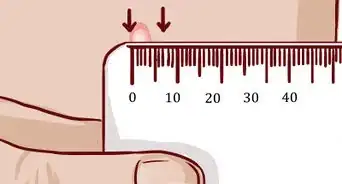
2Take your temperature. A high fever and chills can indicate infection because your body is trying to fight off the infection. If you feel excessively warm suddenly, or have chills, take your temperature and call your doctor.[5]Advertisement
-
3Be alert to eye pain or headache. Some people experience symptoms of light sensitivity and headache with this kind of infection. If you develop a painful reaction to light or intense headaches along with other symptoms, get medical attention.[6]
-
4Take note of any achiness. Muscle aches are a common symptom of infection too. Because muscle aches are symptoms of fever or flu as well as leptospirosis, review your recent activities before deciding these are merely flu symptoms.[7]
-
5Take seriously any feelings of queasiness. You may feel nausea with or without vomiting or diarrhea. Let your doctor know about any sudden stomach problems.[8]
-
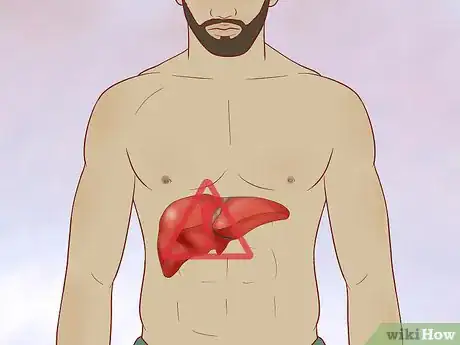
6Pay attention to changes in your coloring. Jaundice may appear later as the infection progresses, and can indicate serious liver problems. Jaundice will typically appear 4-5 days after exposure, so review activities during that time period to assess exposure risks.[9]
-
7Watch for abdominal pain. Pain in the right upper abdominal area is a symptom of second phase infection. Often leptospirosis can develop into chronic renal disease. If you develop pain in this area, see a doctor right away.[10]
-
8Beware of any signs of rash. Sudden rash that is dark red to purple in color is symptomatic of infection. A rash that is concentrated on the lower body or palette of the mouth is specifically associated with this kind of infection.[11]
Knowing When You Should Seek Treatment
-
1Determine your risk of exposure. There are certain environments that increase your chance of exposure to leptospirosis. Factors like climate and land use can make conditions more favorable to the bacteria that cause this infection, so knowing where and when to be alert to those conditions can reduce your chance of infection.[12]
- The bacteria that cause leptospirosis are found in temperate or tropical zones.
- Water is one of the most common places of contamination and infection.
- Urine from infected animals is also a common source. Both domestic and wild animals can be infected. These include, but are not limited to, cattle, pigs, horses, dogs and rats.
-
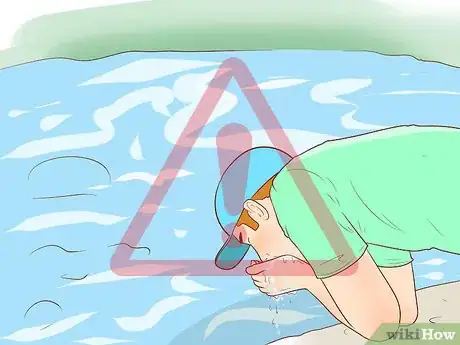
2Be aware of activities that put you at risk. Certain hobbies and professions carry a higher risk of exposure to infection. Know which environments can lead to exposure.[13]
- Athletes who participate in outdoor sports like kayaking and rafting have an increased risk of exposure.[14]
- Campers who swim or wade in contaminated water can be infected.
- Drinking water from contaminated streams or rivers while hiking or camping can be a source of infection.
- People who work in professions or industries involving animals have higher risks for infection. Veterinarians, dairy farmers, as well as workers in the fishing industry and slaughterhouse facilities all face the possibility of infection.
- There has also been an increase in infection rates among urban children in recent years.
-
3Don’t rely on symptoms alone. If you have been exposed, you may or may not exhibit symptoms of infection, so talk to your doctor about activities that may have put you at risk for infection. Depending on your history and what symptoms you do have, your doctor will decide which tests to do and if treatment should be started.[15]
- Symptoms are typically nonspecific so tests are needed to confirm infection.
- Signs of infection are similar to symptoms of other illnesses. If there’s reason to suspect you have been exposed and you develop flu-like symptoms, see your doctor.
- Some people are asymptomatic and may not be affected by the infection. You should see your doctor regardless of how you are feeling if you think you have been exposed.
-
4Contact your doctor if you relapse. For many people, one treatment will be enough to cure them of the infection. Some people may seem to get better without having sought treatment at all initially. However, the leptospirosis infection may not actually have been cured.
- A more serious form of infection may occur after a seeming recovery, usually about a week after the first range of symptoms have cleared up.
- For people with a more severe form of infection, symptoms occur in 2 stages.
- The first stage of the initial illness will be the milder form, with flu-like symptoms.
- The second stage will typically be more severe and last longer than the first stage.
-
5Be alert to signs of second stage infection. The second stage of leptospirosis infection, called Weil’s disease, is much more severe and can have long term health impacts, or even lead to death.[16]
- This second stage can develop after the infection seems to be gone.
- The second stage can also overlap with the first stage of infection.
- At this stage, bacterial infection can cause serious damage to the kidneys or liver, even leading to chronic kidney disease or liver failure with jaundice.
- The bacteria can invade the lungs, posing a serious threat to respiratory health. Severe pulmonary disease, characterized as pulmonary hemorrhage, is a serious complication of leptospirosis. ARDS or acute respiratory distress syndrome is also a complication of leptospirosis.
- Signs of lung infection are having a persistent cough, shortness of breath, and coughing up blood due to bleeding in the lungs.
- Infection can also spread to the heart, causing an enlarged heart, myocarditis, or cardiac arrhythmia.
- Other complications may include rhabdomyolysis and uveitis.
Treating Leptospirosis
-
1Take your overall health into consideration. Many people can recover spontaneously, although it usually will take longer to recover without treatment. You should take into consideration any pre-existing conditions that can increase possible damage to your long term health.[17]
- Pregnant women with leptospirosis infection have a higher infant mortality rate.
- Unborn babies can become infected in utero.
- Heart conditions, respiratory problems, or liver or kidney damage may be worsened if the infection develops into the second stage.
-
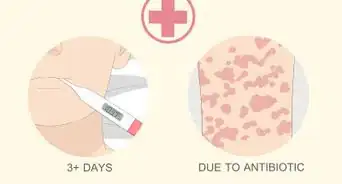
2Start treatment quickly. For most people, the symptoms of leptospirosis will be mild, and the recovery period fairly short. However, should your infection develop into the second stage, symptoms could have major health impacts or even be life-threatening. Treatment can protect you from the more severe stage of infection.[18]
- With treatment, infection and symptoms may last for a few days or for 3 weeks or longer.
- Without treatment recovery may take several months.
- Some people may be completely recovered after the initial infection, but some may not. Your doctor should monitor you during recovery, and for any return of infection symptoms.
-
3Contact your doctor if symptoms return. You may need to extend or change your course of antibiotic treatment if the infection is not responding to the medication.
-
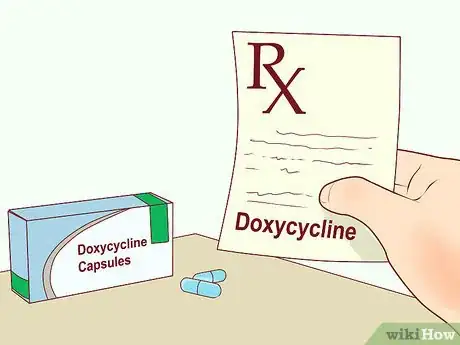
4Take prescribed antibiotics as directed. Antibiotics like doxycycline or azithromycin may be prescribed for milder, first phase infections.[19] Doxycycline should not be used in the pregnant patient, this can cause liver problems and affect the development of the teeth in the unborn infant.
-
5Discuss possible hospital care with your doctor. For severe cases of infection and second phase infection, treatment may include hospital care for intravenous antibiotics (penicillin, doxycycline, ceftriaxone, and cefotaxime) and rehydration treatments as well as antibiotics in pill or liquid forms.[20]
Identifying Infection in Pets
-
1Be alert to possible infection. Symptoms in pets can be nonspecific and vary greatly, and some pets won’t exhibit symptoms at all. If your pet has been exposed to contaminated areas or other animals infected with leptospirosis, consider having it checked even if there are no symptoms.[21]
-
2Be aware of your pet’s level of risk. Younger animals are more vulnerable to serious long term damage to organs or even death. Dogs seem to be more susceptible to becoming infected than other household pets.[22]
-
3Talk to a veterinarian. If you suspect your pet may have been exposed and you see any of the following symptoms, you should contact a veterinarian immediately.[23]
- Fever.
- Vomiting.
- Abdominal pain.
- Diarrhea.
- Refusal to eat.
- Severe weakness and depression.
- Stiffness.
- Severe muscle weakness.
-
4Seek treatment if your pet is infected. Getting your pet on antibiotics in the early stages of the infection is very important. Antibiotics will help your pet recover more quickly, lessen any damage to internal organs, and shorten the length of time during which you are at risk for infection.[24]
-
5Know what to expect. Because of the possibility of permanent damage to your pet’s health, as well as your risk of becoming infected through contact with your pet, ask your veterinarian for advice and information about what to do while the infection persists.[25]
- Typically, the infection will be active for between 5 to 14 days. For some animals however, the infection can last for just a few days or for as long as several months.
- While your pet is infected, there is a risk of the infection spreading to you and anyone else caring for the pet.
- With normal daily activities like grooming, petting, walking and playing the risk for transmission is typically low.
- There is a risk for becoming infected through direct or indirect contact with urine, blood, or tissues.
-
6Contact a veterinarian if your pet is not making progress. Also contact the veterinarian if your pet is experiencing problems due to symptoms from infection. Your pet may need dialysis and hydration therapy to recover.
References
- ↑ https://emedicine.medscape.com/article/220563-overview
- ↑ https://www.cdc.gov/leptospirosis/exposure/index.html
- ↑ https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/leptospirosis
- ↑ https://www.medscape.com/answers/220563-82077/what-are-the-signs-and-symptoms-of-leptospirosis
- ↑ https://www.cdc.gov/leptospirosis/symptoms/index.html
- ↑ http://emedicine.medscape.com/article/220563-overview
- ↑ https://www.nhs.uk/conditions/leptospirosis/
- ↑ http://emedicine.medscape.com/article/220563-overview
- ↑ http://patient.info/doctor/leptospirosis-weils-disease
- ↑ https://www.cdc.gov/leptospirosis/symptoms/index.html
- ↑ https://www.nhs.uk/conditions/leptospirosis/
- ↑ https://www.cdc.gov/leptospirosis/infection/index.html
- ↑ https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/leptospirosis
- ↑ http://www.cdc.gov/features/leptospirosis/
- ↑ http://emedicine.medscape.com/article/220563-overview
- ↑ https://patient.info/doctor/leptospirosis-weils-disease
- ↑ https://www.msdmanuals.com/home/infections/bacterial-infections-spirochetes/leptospirosis
- ↑ https://www.msdmanuals.com/home/infections/bacterial-infections-spirochetes/leptospirosis
- ↑ https://emedicine.medscape.com/article/220563-treatment
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4111189/
- ↑ https://www.cdc.gov/leptospirosis/pets/index.html
- ↑ https://www.avma.org/public/PetCare/Pages/Leptospirosis.aspx
- ↑ http://www.petmd.com/dog/conditions/infectious-parasitic/c_multi_leptospirosis
- ↑ https://www.cdc.gov/leptospirosis/pets/treatment/index.html
- ↑ http://www.petmd.com/dog/conditions/infectious-parasitic/c_multi_leptospirosis#
About This Article
To recognize leptospirosis symptoms, look for high fever, chills, achiness, nausea, light sensitivity, and intense headaches. Since the infection can lead to jaundice, keep an eye out for any changes in the color of your skin. You should also watch out for pain in your right upper abdominal area or a dark red to purple rash on your lower body or around your mouth. If you notice any of these signs, go to a doctor so they can start treatment, such as antibiotics, as soon as possible before the infection develops into something more serious. For more information from our Medical co-author, including how to figure out your risk of exposure to leptospirosis, read on!




























-Step-11.webp)
















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...