This article was medically reviewed by Jonas DeMuro, MD and by wikiHow staff writer, Glenn Carreau. Dr. DeMuro is a board certified Pediatric Critical Care Surgeon in New York. He received his MD from Stony Brook University School of Medicine in 1996. He completed his fellowship in Surgical Critical Care at North Shore-Long Island Jewish Health System and was a previous American College of Surgeons (ACS) Fellow.
There are 17 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 92,942 times.
Toxic Shock Syndrome (TSS) is a rare but serious condition caused by staph or strep bacterial infections. It's often associated with using extra-absorbent tampons, but regardless of gender and age, anyone can come down with this condition. TSS can be hard to recognize because its symptoms mimic other illnesses like the flu, but a quick diagnosis and treatment can help you recover fully. Read on for a full explanation of TSS symptoms, risk factors, causes, and prevention tips.
Steps
Symptoms of Toxic Shock Syndrome
-
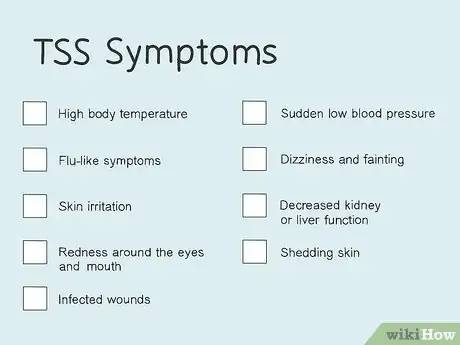
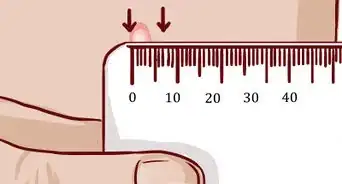
1High body temperature. TSS causes a high fever (usually above 102 °F (39 °C)) around the time that symptoms begin. Your normal body temperature can range between 97 °F (36 °C) and 99 °F (37 °C), with the average being 98.6 °F (37.0 °C). If you feel hot, take your temperature and determine whether you have a fever.[1]
- While a fever alone does not guarantee TSS, the circumstances of that fever can help you figure out when TSS is a possibility.
- If you suddenly get a fever while menstruating and using a tampon or while you have an oozing surgical wound, it's a telltale sign of TSS.
-
2Flu-like symptoms. A fever caused by TSS is typically accompanied by severe muscle aches, fatigue, chills, sore throat, cough, and headaches. It can be tough to differentiate TSS from an ordinary illness, but both the factors surrounding the sudden sickness and other TSS symptoms can help you tell them apart.[2]
- Another common flu-like symptom of TSS is nausea, accompanied by severe vomiting or watery diarrhea.
- Just like a fever, the flu doesn't mean you have TSS—but experiencing flu-like symptoms while menstruating or when you have a surgical wound is a significant indicator.
- If it is reasonably plausible that you may have TSS, keep a close eye out for other symptoms. Listen closely to your body to ensure you don't miss any vital signs!
-
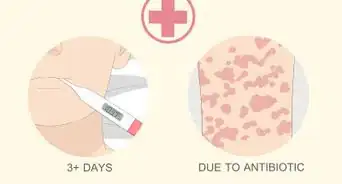
3Skin irritation. One telltale sign of TSS is red rashes that look like sunburn, particularly on the palms of your hands and the soles of your feet. However, it's important to note that TSS rashes can occur anywhere on your body. If you develop other symptoms, check your body for signs of a rash, as this can help diagnose the condition.[3]
- Like a sunburn, the rash won't be raised or bumpy on your skin. It'll be flat and red, covering areas of your body in large splotches.
-
4Redness around the eyes and mouth. You may notice bloodshot eyes and an unusual redness under your eyelids if you have TSS. The inside of your mouth can also become bright red, as can your vagina if you have one. Check each area for signs of redness if you suspect you have TSS.[4]
- The redness results from increased blood flow to the mouth, eyes, and vagina in people with TSS.
-
5Infected wounds. TSS can develop as a result of bacteria entering an open wound. If you have an injury on your body, particularly as the result of surgery or a viral infection that caused open sores, the risk for contracting TSS increases.[5] Check your wound if you have one: it will show signs of infection if TSS sets in, becoming red, swollen, and extremely painful.
- An infected wound may also produce foul-smelling discharge—typically white, though it can vary in color. If you see this, your injury needs immediate medical attention.
-
6Sudden low blood pressure. Low blood pressure (hypotension) develops as TSS sets in, meaning less blood is pumped throughout your body and up to your brain. Symptoms of hypotension include lightheadedness, confusion, nausea, fatigue, and blurred vision. It usually takes hypotension roughly 24 to 48 hours to set in after the first symptoms of TSS (fever and flu) set in.[6]
- If someone else is with you (or you're with someone who may have TSS), it's also possible to note agitation or unusual changes in behavior when a person has hypotension.
-
7Dizziness and fainting. Sudden low blood pressure also typically leads to extreme disorientation and loss of consciousness. Passing out (especially while experiencing other symptoms of hypotension or fever and flu-like symptoms) is a strong indicator that you're dealing with toxic shock syndrome.[7]
-
8Decreased kidney or liver function. If you have to pee a lot less than usual and you have fatigue, loss of appetite, nausea, and a decrease in your mental sharpness, it may mean that your kidneys are having trouble due to TSS. Liver failure can be detected through swelling in the legs, ankles, and abdomen, a dark urine color, and yellowish skin (also called jaundice). TSS can ultimately cause kidney and liver failure.[8]
-
9Shedding skin. Not long after rashes develop, the skin may start peeling. This is typically seen 1 to 2 weeks after your symptoms begin. Like sunburns, the skin around the rash areas will peel off, though it will do so in large sheets, particularly around the palms and soles of the feet. If you develop a rash that then sheds despite no extended exposure to sunlight that could cause a burn, TSS could be the source.[9]
Causes of Toxic Shock Syndrome
-
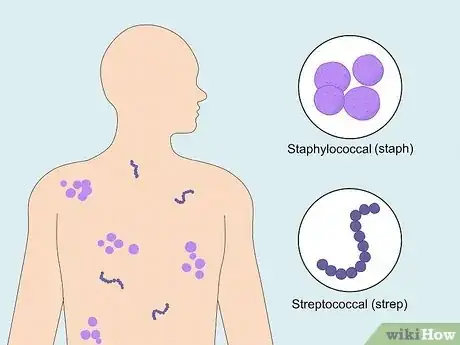
1A bacterial infection can increase the risk of getting TSS. The condition is usually caused by two types of bacteria: staphylococcal (staph) and streptococcal (strep). Strep bacteria cause infections like bacterial cellulitis and chickenpox, which is why people who have them can, in rare cases, develop TSS as a secondary infection.[10]
- Staph bacteria usually live on your skin harmlessly, but it can cause an infection when it gets into your body.
-
2Tampons and menstrual cups can increase the risk of TSS. Toxic shock syndrome is the result of harmful bacteria entering your body. When left in the vagina for too long, super-absorbent tampons (or menstrual cups) can encourage bacteria to grow and enter your bloodstream. Alternatively, tampons can stick to vaginal walls and cause tiny scrapes when removed, allowing bacteria to get into your body.[11]
- Inserted contraceptives like diaphragms and sponges left in your body for too long can also increase your risk for TSS.
- Occasionally, childbirth can also lead to TSS. The third type of bacteria that causes TSS is called Clostridium sordellii, which usually lives harmlessly in the vagina but can get into the uterus during childbirth.
-
3Surgical wounds or injuries on your skin can lead to TSS. Beyond surgery wounds, possible injuries that can get infected and cause you to develop TSS include cuts, burns, boils, nosebleeds, and insect bites. Strep or staph bacteria that get into your skin through open wounds release toxins that cause toxic shock syndrome and damage vital organs in your body.[12]
Getting Medical Attention
-
1Weigh your risk of having TSS. Symptoms of TSS can come from multiple causes, so narrowing down why you feel the way you do is essential. Since the causes of TSS are also pretty specific, you can use them to differentiate it from the flu and other common illnesses. If any causes of TSS apply to you and you notice the telltale symptoms above, you might have toxic shock syndrome.[13]
- TSS cannot be spread from person to person. The bacteria that causes TSS can be spread through direct contact (although even coming into contact with the bacteria does not guarantee TSS).
-
2Seek medical attention immediately if you identify symptoms of TSS. When caught early, Toxic Shock Syndrome is usually highly treatable. However, undetected TSS can progress rapidly, resulting in lengthy hospital stays, and (in rare cases) can be fatal. So, don't panic if you suspect TSS, but play it safe. If you have symptoms or risk factors of TSS, get medical assistance right away.[14]
- Symptoms can set in as early as 12 hours after getting TSS.
- Unless otherwise instructed while contacting medical assistance, immediately remove the tampon you are using (if relevant in your situation).
How is toxic shock syndrome treated?
-
1Patients with TSS need to stay in the hospital for several days. While TSS is treatable, care in the hospital's ICU (intensive care unit) is required to stop the infection. Doctors will give standard shock and organ failure treatments, including IV fluids, oxygen, and medicine. If you have them, doctors will also clean your wounds and drain infected abscesses.[15]
- Depending on your case and the severity of the TSS, other symptom-based treatments will also be given.
-
2Antibiotics are used to treat the infection. If you get TSS, doctors will always administer antibiotics to stop the disease and manage sepsis—a chemical response triggered by your body to fight infection, which damages organs in the process. Penicillin and clindamycin are commonly used together to treat patients with TSS, though antibiotic therapy can be tailored to your needs.[16]
-
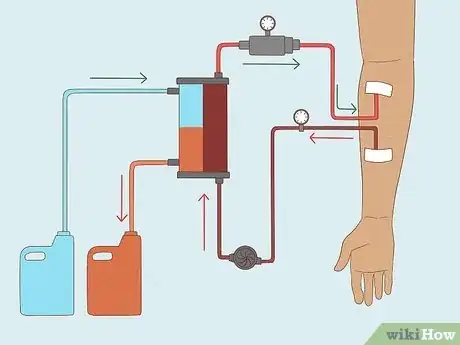
3Dialysis may be needed in case of kidney failure. If you are diagnosed with TSS after your kidneys show signs of decreased function, damage from the infection will be treated with dialysis. When your kidneys are damaged, they don't filter blood properly, so dialysis does the work for them and filters out waste. This gives your kidneys time to heal and start working again![17]
-
4Dead tissue will be surgically removed in extreme cases of TSS. Even when caught late after the infection worsens, TSS is still treatable. However, when the damage progresses so far that it kills tissue in the body, surgery—and sometimes even amputation—is needed to get rid of the infected issue and let the body heal.[18]
- When organs fail, gangrene can set in, which is what causes tissue to die and limbs (like fingers, toes, hands, and feet) to be surgically removed.
Preventing Toxic Shock Syndrome
-
1Treat wounds quickly. TSS is a rare condition! You can prevent it by taking care of your physical health when you get hurt. Clean and bandage any wound immediately, or get medical attention if necessary. This stops bacteria that cause TSS from entering the wound and infecting it.[19]
- Care for minor wounds easily at home by removing any small foreign objects, rinsing the wound with water, and applying antibiotic ointment before bandaging it.
-
2Practice good hygiene when using tampons. Wash your hands before and after inserting tampons to ensure there are no harmful bacteria on your hands that could cause TSS. Follow all instructions on the box when using tampons and change them out regularly (usually between 4 and 8 hours, depending on the type). Avoid using extra-absorbent tampons at the end of your period.[20]
- Always insert a fresh tampon before going to bed, rather than leaving a used tampon inside you overnight—and remove it when you wake up.
- Use tampons with the lowest absorbency possible. It's okay if you have a heavy flow and need extra-absorbent tampons, but don't use them if you have a light flow.
- In addition, keep a sponge or diaphragm contraceptive inserted for only as long as necessary, and never for more than twenty-four hours.
-
3Know the risk factors of TSS. Unfortunately, once you have had TSS, you're approximately 30% more likely to get it again. Use only pads (rather than tampons) and an alternative method of contraception to sponges or diaphragms. It's also important to note that adults over 65 are more likely to get TSS, as are people with a chronic illnesses such as diabetes or alcohol use disorder.[21]
References
- ↑ https://www.cdc.gov/groupastrep/diseases-public/streptococcal-toxic-shock-syndrome.html
- ↑ https://www.cedars-sinai.org/health-library/diseases-and-conditions/t/toxic-shock-syndrome-tss.html
- ↑ https://www.cedars-sinai.org/health-library/diseases-and-conditions/t/toxic-shock-syndrome-tss.html
- ↑ https://kidshealth.org/en/teens/tss.html
- ↑ https://www.cdc.gov/groupastrep/diseases-public/streptococcal-toxic-shock-syndrome.html
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/toxic-shock-syndrome-tss
- ↑ https://www.nhs.uk/conditions/toxic-shock-syndrome/
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/toxic-shock-syndrome-tss
- ↑ https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=EN&Expert=99919
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK459345/
- ↑ https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/toxic-shock-syndrome-tss
- ↑ https://myhealth.alberta.ca/Health/Pages/conditions.aspx?hwid=hw140188
- ↑ https://www.vdh.virginia.gov/epidemiology/epidemiology-fact-sheets/toxic-shock-syndrome/?pdf=1093
- ↑ https://www.dignityhealth.org/conditions-and-treatments/womens-services/perimenopause/toxic-shock-syndrome/diagnosis-and-treatment
- ↑ https://www.nhs.uk/conditions/toxic-shock-syndrome/
- ↑ https://www.msdmanuals.com/professional/infectious-diseases/gram-positive-cocci/toxic-shock-syndrome-tss
- ↑ https://www.healthychildren.org/English/health-issues/conditions/infections/Pages/Toxic-Shock-Syndrome.aspx
- ↑ https://my.clevelandclinic.org/health/diseases/15437-toxic-shock-syndrome
- ↑ https://www.nidirect.gov.uk/conditions/toxic-shock-syndrome
- ↑ https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/toxic-shock-syndrome-tss
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK459345/
About This Article
Toxic shock syndrome is a rare bacterial infection which often comes with flu-like symptoms. In most cases, toxic shock syndrome is associated with tampon use, but men and children can also get it. If you have flu-like symptoms that don't go away, such as intense aches, vomiting, and diarrhea, you may have toxic shock syndrome. Other common symptoms include sunburn-like rashes on your hands and feet, dizziness, disorientation, and in severe cases, seizures. If you think you might have toxic shock syndrome, seek medical help immediately. Fortunately, it’s easily treated with antibiotics when caught early on, but if left untreated, it can be severe. For more tips from our Medical co-author, including how to prevent reinfection of toxic shock syndrome, read on.
























-Step-11.webp)

















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...