This article was medically reviewed by Sarah Gehrke, RN, MS. Sarah Gehrke is a Registered Nurse and Licensed Massage Therapist in Texas. Sarah has over 10 years of experience teaching and practicing phlebotomy and intravenous (IV) therapy using physical, psychological, and emotional support. She received her Massage Therapist License from the Amarillo Massage Therapy Institute in 2008 and a M.S. in Nursing from the University of Phoenix in 2013.
There are 10 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 89% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 388,656 times.
Your doctor may run a blood gas analysis or arterial blood gas (ABG) test if you are showing the signs of an oxygen, carbon dioxide, or pH imbalance such as confusion or difficulty breathing. This test measures the partial levels of these substances using a small blood sample. From these numbers, your doctor can figure out how well your lungs move oxygen into your blood and remove carbon dioxide from your body. It can also indicate certain medical conditions such as kidney or heart failure, drug overdose, or uncontrolled diabetes. Your doctor is the best person to interpret the test results, but you can also get an idea about them yourself. You can interpret your test results by reviewing them closely and considering other data.
Steps
Reviewing Your Test Results Closely
-
1Evaluate the results with your doctor. The best way to interpret your blood results is by talking to your doctor. They understand the information and results better than anyone. Making an assessment on your own can lead to misdiagnosis or complications from self-treatment. Ask your doctor any questions you may have about individual or total levels and what they may indicate.
- Have your doctor go through each series of numbers individually, explaining what they test for and what your specific results may mean.
- Ask your doctor to compare previous results with the new ones to better judge where you are physically.
-
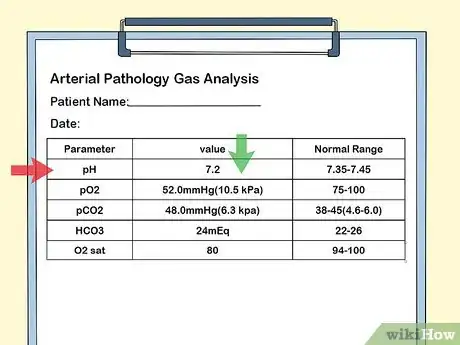
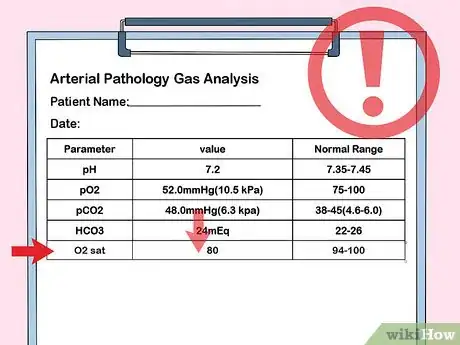
2Look at the pH number. This measures the number of hydrogen ions in your blood, which may indicate conditions such as COPD, asthma, pregnancy, diabetic ketoacidosis (DKA), lung disease, liver disease, or drug use.[1] The normal range for pH values are between 7.35 to 7.45.[2]
- If the pH level is below 7.38, then you may have more acidic blood from conditions such as airway obstruction, COPD, asthma, sleep disordered breathing, or neuromuscular impairment.[3]
- If the pH level is above 7.45, you may have a alkalosis, which could indicate stimulation of the central nervous system, lung disease, severe anemia, drug use, or pregnancy.
Advertisement -
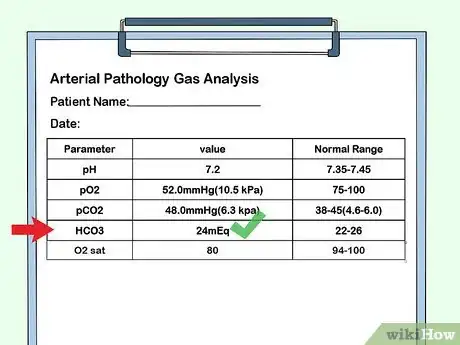
3Check bicarbonate, or HCO3, numbers. Your kidneys produce bicarbonate and help maintain a normal pH. The normal level for bicarbonate is between 22 to 26 milliEquivalents Per Liter (mEq/L). A disruption of your bicarbonate levels may indicate conditions such as respiratory failure, anorexia, and liver failure.[4]
- An HCO3 level is below 24 mEq/L indicates metabolic acidosis. It may be the result of conditions including diarrhea, liver failure and kidney disease.
- An HCO3 level above 26 mEq/L indicates metabolic alkalosis. This may be the result of dehydration, vomiting, and anorexia.
-
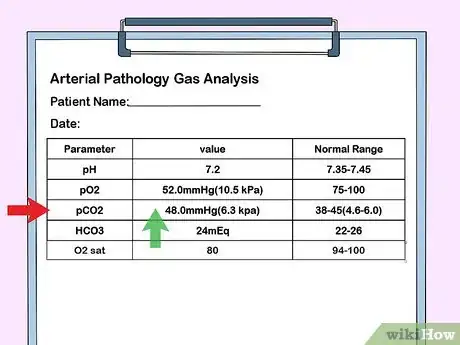
4Examine the PaCO2 number. Partial pressure of carbon dioxide, or PaCO2, measures the carbon dioxide in your blood. The normal level for PaCO2 is between 38 and 45 mmHg. Disrupted levels may indicate shock, kidney failure, or chronic vomiting.
- Respiratory alkalosis is present if the PaCO2 number is below 35 mmHg. This means there is too little carbon dioxide in the blood. It can signal kidney failure, shock, diabetic ketoacidosis, hyperventilation, pain, or anxiety.[5]
- Respiratory acidosis is present if the PaCO2 number is above 45 mmHg. This means that there is too much carbon dioxide in the blood. This can be a sign of chronic vomiting, low blood potassium, COPD, or pneumonia.
-
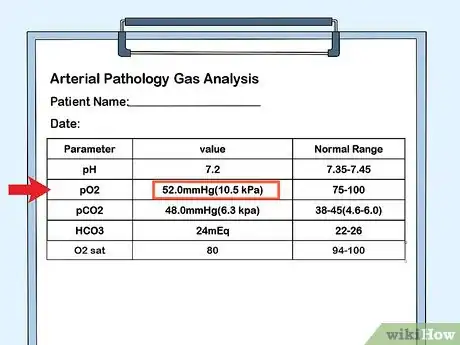
5Inspect the PaO2 number. Partial pressure of oxygen, or PaO2, measures how well oxygen can flow from your lungs into your blood. The normal level is between 75 to 100 mmHg. Higher or lower levels may indicate conditions such as anemia, carbon monoxide poisoning, or sickle cell disease.[6]
-
6Notice oxygen saturation. How well your hemoglobin carries oxygen to your red blood cells is called oxygen saturation. The normal levels are between 94 and 100%. Lower saturation rates may indicate the following:[7]
- Anemia
- Asthma
- Congenital heart defects
- COPD or emphysema
- Strained abdominal muscles
- Collapsed lung
- Pulmonary edema or embolism
- Sleep apnea
Considering Other Data
-
1Figure in medications or drugs. Certain factors such as your health, medication you take, and where you live can affect the results of your blood gas test. If you are taking any of the following medications or drugs, recognize that they may disrupt your blood gas results:
- Blood thinners, including aspirin
- Illicit drugs
- Tobacco or secondhand smoke
- Tetracycline (antibiotics)[8]
- Steroids
- Diuretics
-
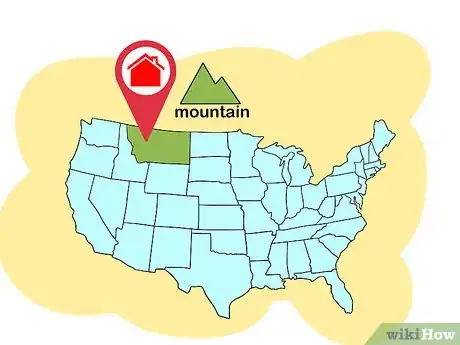
2Recognize your location. The amount of oxygen in the air decreases with elevation, which can also affect your blood gas results. If you live at altitudes of 3,000 feet (900 meters) or higher, factor this in your test.[9] Ask your doctor to correlate your partial pressure of oxygen with your location or factor that a healthy level of saturation is 80-90% between 10,000 – 15,000 feet.
- Respiratory alkalosis is commonly associated with people going to mountainous areas. Hyperventilation is especially likely when ascent is too rapid and there hasn’t been enough time to acclimate.[10]
-
3Acknowledge current medical conditions. Medical conditions ranging from liver failure to a simple fever can affect your blood gas results. Consider these as you review your test or discuss it with your doctor. The following conditions may disrupt normal blood gas levels:[11]
- Fever
- Hyperventilation
- Prior drug overdose
- Head or neck injury
- Respiratory disorders such as asthma and COPD
- Congestive heart failure
- Kidney failure
- Diabetes
- Blood disorders such as hemophilia
-
4Compare earlier tests. If you’ve had previous blood gas tests, review the results from them. This can give you an idea of any discrepancies that may indicate a new condition or improvement of another. Remember to discuss these results with your doctor, too.
Warnings
- Discuss test results with your doctor to ensure proper interpretation of the results.⧼thumbs_response⧽
References
- ↑ http://www.thoracic.org/professionals/clinical-resources/critical-care/clinical-education/abgs.php
- ↑ https://www.pharmaceutical-journal.com/news-and-analysis/opinion/correspondence/how-to-interpret-arterial-blood-gas-results/11069997.article?firstPass=false
- ↑ http://www.thoracic.org/professionals/clinical-resources/critical-care/clinical-education/abgs.php
- ↑ https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=167&contentid=bicarbonate
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4515441/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4666443/
- ↑ http://www.mayoclinic.org/symptoms/hypoxemia/basics/causes/sym-20050930
- ↑ https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=167&contentid=bicarbonate
- ↑ https://medlineplus.gov/ency/article/003855.htm







-Step-14-Version-2.webp)
























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...