This article was medically reviewed by Tu Anh Vu, DMD. Dr. Tu Anh Vu is a board certified dentist who runs her private practice, Tu's Dental, in Brooklyn, New York. Dr. Vu helps adults and kids of all ages get over their anxiety with dental phobia. Dr. Vu has conducted research related to finding the cure for Kaposi Sarcoma cancer and has presented her research at the Hinman Meeting in Memphis. She received her undergraduate degree from Bryn Mawr College and a DMD from the University of Pennsylvania School of Dental Medicine.
There are 9 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 61,141 times.
Experts agree that getting a tooth pulled (called a tooth extraction) is a common experience and nothing to worry too much about. You may need to get your tooth pulled if you have untreated tooth decay, damage to your tooth, or crowded teeth.[1] Research shows that wisdom teeth are the most commonly extracted teeth, and they may need to be pulled if you don't get them removed when they start to grow in.[2] While it's normal to be scared before you go to the dentist, you likely won't feel any pain while your tooth is being pulled, as your dentist will probably give you something to numb the area.
Steps
Finding Out if You Need Your Tooth Pulled
-
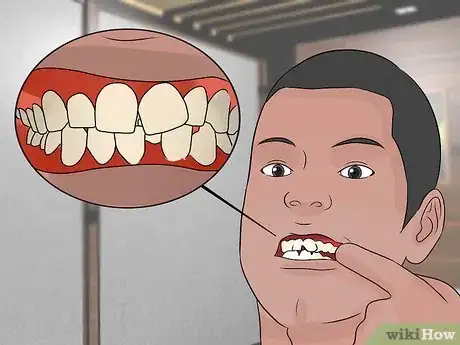
1Check for tooth decay. Tooth decay refers to any deterioration in the physical tooth surfaces — including cavities — often caused by plaque (bacteria feeding on substances leftover from eating, especially sugary or processed foods) eroding the enamel. This eventually causes inflammation of the inner pulp of the tooth. Decay, if left unchecked, can put deep holes in the tooth and cause infection, leading to extraction.[3]
- You can see signs of decay or damage by looking carefully in a mirror under good lighting.
- Check for discoloration on the tooth surface.
- Look for missing pieces or unusual marks on the tooth.
- See if the gums around the tooth are red, swollen, tender, painful, and/or bleeding.
- You may also notice a filling surrounded by black, which may be a secondary decay located at the margins of your filling.
-
2Examine the tooth for damage. If a permanent tooth is loose, this may indicate some damage or trauma was suffered in the immediate area. If the tooth falls out on its own, save it in a clean container and bring it to your dentist.Advertisement
-
3Look for signs of gum disease. If your gums around particular teeth are red, painful, swollen, and/or bleed frequently then you may have gum disease and/or an infection that will lead to an extraction.[4]
- Look for gums that have pulled away from the tooth.
- Persistent bad breath can be a sign of gum disease.
- Pay attention to any changes in the way your teeth fit when you bite.
- Notice you feel any type of mobility of your teeth when you bite. In some cases you may feel an opposing force from a tooth when you bite, similar to a spring that has a force on it. This may be due to an infection at the end of the root
- If you wear dentures, be aware of any changes in their fit.
- This can become a more advanced form of gum disease called periodontitis as further bone and tissue loss leads to looser teeth.
-
4Consult with your dentist if "crowding" is occurring. A common reason for tooth extraction is when a tooth is trying to break through the gum. One of the most common occurrences of this is when "wisdom" teeth are coming in.[5]
- If you have a fever and notice swelling, pus, and/or feel pain around the area where the tooth should be emerging, it could be a sign of an abscess and require attention as soon as possible.
- Swollen tonsils and swallowing difficulties will appear when lower wisdom teeth are involved.
- Ask your dentist about the risks of keeping the wisdom teeth in or removing them.
-
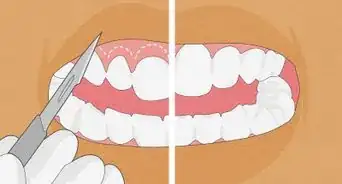
5Check for misaligned teeth. Another reason for tooth extraction occurs when the process of orthodontics (to properly align one's teeth) needs to move forward, but is hindered by the amount of room in the patient's mouth.[6]
- Braces work by placing a small brackets (metal, ceramic, or plastic) on each tooth and holding them together with wires. Sometimes additional fixtures like oral bands are used on the teeth that serve as an anchor for the wires and exterior head gear are used for more severe bite corrections. Spacers are used between the teeth that need to make room for the bands.[7]
- Ask your orthodontist about newer and more cosmetic varieties of braces that are just as effective, but less intrusive on the patient's daily life.
- Braces are usually worn by a patient for a duration of one to three years.
- Talk with an orthodontist about braces and any steps that will need to be taken once the braces are removed. She will make a determination if an extraction is necessary to make room in the patient's mouth during the procedure.
Going to the Dentist
-
1Schedule a dental appointment as soon as possible. If one or more teeth show signs of decay and/or damage, your gums are showing signs of infection, or these areas are giving you pain, then a dentist needs to determine the cause.[8] If your condition is extreme and no dentist is available in a timely fashion, you can consider going to your local emergency room.
- Before going to an emergency room or to your dentist, make sure they have x-ray equipment. If not, search for a dental x-ray center in order to save valuable time. Every tooth which is not extremely loose requires x-ray before extraction.
- If you suffered any injury to cause the possible need for extraction, let your dentist know.
- If your tooth has already fallen out or lost any portions that you managed to save, bring them along. This will help give your dentist an idea of what is left to be extracted.
-
2Bring necessary paperwork to your dental visits. Copies of any insurance, discount cards, medical records (or contact information to get them) and identification should all be brought to dental visits.
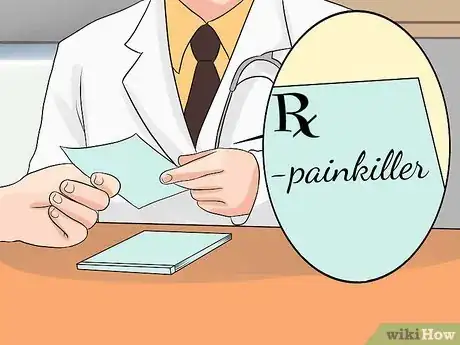
- Make sure you inform your dental provider with up to date information regarding medication you are on. He will need to know in case an extraction is the chosen course of action and uses anesthetic and/or painkillers later.
-
3Get a dental exam. The dentist will diagnose any oral condition you may be suffering as a result of problems with your teeth and/or gums. You will need to consult with her to make the final determination if extraction is necessary, or if another course of action can be taken.[9]
- Report to the dentist any incident(s) that may have caused the tooth's decay or damage.
- Provide the dentist any tooth or parts of tooth you may have saved.
- Submit to an oral x-ray of your mouth if recommended.
-
4Review the extraction procedures with your dentist. Know what to expect if extraction is indeed the recommended course of action.
- Either version of the extraction procedure will first involve injecting local anesthetic near the extraction area to numb it. Review any medical problems, such as allergies or adverse reactions you may have with anesthesia, if necessary.
- The most common type of tooth pulling procedure is a "simple extraction" in which the tooth is easily visible in the mouth. The dentist loosens the tooth with what is called an "elevator." Then the dentist uses another tool — forceps —to remove the tooth.
- Surgical extractions are used for broken or hidden teeth — and are usually performed by oral surgeons, though some regular dentists will perform the procedure. The dentist/surgeon must cut into the gum and sometimes cut away some of the bone around the tooth and cut the tooth itself in order to remove it.
-
5Gather information from your dentist on the risks of the extraction. These risks include problems with the physical procedure and aftermath risk with infection.
- A problem called a dry socket occurs in a small percentage of patients. This happens when the bone under the removed tooth is exposed to contamination if a blood clot doesn't remain in place after extraction. This can also occur after a very difficult extraction that caused the bone and blood vessels to expand.
- The dentist can accidentally damage neighboring teeth or jaw.
- The sinuses in the nearby area can be damaged. They will usually heal themselves, but more extreme cases would require additional surgery.
- Soreness in the extraction area or jaw.
- Numbness in the extraction area or jaw. This can be long-lasting or permanent if there is nerve damage.
- In some cases of anesthesia required for the extraction of upper front teeth up to premolars you may experience double vision or eyesight disorder for about an hour
Recovering After the Extraction
-
1Determine your needs after an extraction. This will take a combination of caring for the area the tooth was extracted and pain management. Consult closely with your dentist on keeping up dental hygiene, and spotting warning signs if the affected area is not healing correctly.[10]
- After the extraction your dentist will have placed gauze in the area to let a blood clot form. Change this pad early to avoid it becoming soaked with blood, but then leave it two to three hours to allow the blood clot to remain and stabilize in the socket.
- Take your dentist's prescribed painkillers as instructed.
- Keep ice bags around to apply to your face and reduce swelling. You may try applying the ice for 10-minute intervals.
- Avoid excessive physical activity, harsh mouthwashes, spitting, drinking from straws, smoking, eating hard foods, and lying too flat when resting for the day or two after the extraction. In addition, avoid heat in the area and do not sleep on that side, especially not propped up on your hands. Try to sleep faced up on a higher position by placing two pillows underneath your head.
-
2Report to your dentist immediately if you experience more severe difficulties. Problems are most likely to start at the extraction location, though some symptoms can be more general.[11]
- Your dentist may place sutures in order to help and fasten the healing but also to protect the blood clot. They should be removed after seven days.
- Let your dentist know if you have signs of infection such as fever, chills, and/or redness at the extraction location.
- If you feel nausea and/or experience vomiting soon after the procedure, also let your dentist know.
- If you feel short of breath, have bouts of coughing, and/or start suffering chest pains within a short time of the procedure, then let the dentist know immediately.
-
3Start a better oral hygiene regimen. If you were not already regularly brushing your teeth, flossing, and rinsing with mouthwash in order to prevent tooth decay and gum disease, then it is at least as important to do so after an extraction. The same techniques generally will work apart from some extra care in the week or two immediately after the extraction procedure.[12]
- Ask your dentist if she recommends any particular variety of toothpaste and toothbrush for your condition — especially after an extraction.
- Brush twice a day, including once before you go to bed.
- When brushing and flossing, don't neglect your back teeth.
- You should keep mouthwash or a dental rinse as part of the hygiene regimen. Some will instruct you to rinse before the brushing phase, some are to be used after the brushing phase.
-
4Change your eating habits. Eating balanced meals and reduced snacking can cut down on the sugars and other stain-leaving foods and drinks that frequently damage teeth.
- You don't have to eliminate things like coffee, teas, sodas, sugary snacks from your diet — but consume them in moderation.
- Ask your dentist about varieties of toothpaste or cleaning procedures that might help stave off decay in addition to regular efforts.
-
5See your dentist more regularly. Having check-ups and cleaning by your dentist and dental hygienist on a schedule can maintain the health of your teeth and gums.
- These check-ups, often called prophylaxis, can also spot potential problems early and allow your dentist and you to come up with a plan to deal with them before they become more severe.
- If you have dental insurance or a discount plan, consult with them on how often they will cover these visits.
Expert Q&A
-
QuestionDoes an infected tooth need to be pulled?
 Tu Anh Vu, DMDDr. Tu Anh Vu is a board certified dentist who runs her private practice, Tu's Dental, in Brooklyn, New York. Dr. Vu helps adults and kids of all ages get over their anxiety with dental phobia. Dr. Vu has conducted research related to finding the cure for Kaposi Sarcoma cancer and has presented her research at the Hinman Meeting in Memphis. She received her undergraduate degree from Bryn Mawr College and a DMD from the University of Pennsylvania School of Dental Medicine.
Tu Anh Vu, DMDDr. Tu Anh Vu is a board certified dentist who runs her private practice, Tu's Dental, in Brooklyn, New York. Dr. Vu helps adults and kids of all ages get over their anxiety with dental phobia. Dr. Vu has conducted research related to finding the cure for Kaposi Sarcoma cancer and has presented her research at the Hinman Meeting in Memphis. She received her undergraduate degree from Bryn Mawr College and a DMD from the University of Pennsylvania School of Dental Medicine.
Board Certified Dentist It really depends on the situation in your mouth. The only way to know if you need to get a tooth pulled is if you go to see a dentist and have your teeth examined by a professional. Keep in mind, tooth extractions are extremely common so you don't need to worry a whole lot, but not doing anything about it is a bad idea since the underlying problem may get worse.
It really depends on the situation in your mouth. The only way to know if you need to get a tooth pulled is if you go to see a dentist and have your teeth examined by a professional. Keep in mind, tooth extractions are extremely common so you don't need to worry a whole lot, but not doing anything about it is a bad idea since the underlying problem may get worse.
Warnings
- Do not pull out damaged permanent teeth carelessly on your own. This can lead to infection and damage to the surrounding area.⧼thumbs_response⧽
- There are high risks with not making room for teeth that are coming in including cysts, pain, infection, tumors, decay, and damage to neighboring teeth. This is why is an OPG (full mouth x-ray ) is required from time to time, especially after the age of 20, in order to keep track of any modifications that may appear.⧼thumbs_response⧽
- Not correcting misaligned teeth can lead to eating disorders, head pain, migraines, and also jaw disorders that can block the inferior jaw, which will leave the person unable to close his jaw.⧼thumbs_response⧽
References
- ↑ https://www.gosh.nhs.uk/teenagers/your-condition/tests-and-treatments/tooth-extraction
- ↑ https://www.yourdentistryguide.com/tooth-extraction/
- ↑ https://www.nhs.uk/conditions/tooth-decay/
- ↑ Tu Anh Vu, DMD. Board Certified Dentist. Expert Interview. 10 April 2020.
- ↑ http://www.mouthhealthy.org/en/az-topics/w/wisdom-teeth
- ↑ http://www.mouthhealthy.org/en/az-topics/b/braces
- ↑ https://www.nhs.uk/conditions/braces-and-orthodontics/
- ↑ Tu Anh Vu, DMD. Board Certified Dentist. Expert Interview. 10 April 2020.
- ↑ Tu Anh Vu, DMD. Board Certified Dentist. Expert Interview. 10 April 2020.
About This Article
To find out if your tooth needs to be pulled, look for signs of decay, such as discoloration of the tooth, missing pieces of enamel, or swelling and bleeding of the gums. Additionally, check to see if any of your teeth are loose, and save any teeth that fall out so your dentist can examine them. You may also need an extraction if you’re suffering from gum disease, so look out for symptoms such as persistently bad breath and receding gums. Finally, check for problems such as misalignment or overcrowding of your teeth. Keep reading for more advice from our Dental Health co-author, including how to find out from your dentist if you need an extraction!





































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...