This article was medically reviewed by Mark Ziats, MD, PhD. Dr. Mark Ziats is an Internal Medicine Physician, Scientist, Entrepreneur, and the Medical Director of xBiotech. With over five years of experience, he specializes in biotechnology, genomics, and medical devices. He earned a Doctor of Medicine degree from Baylor College of Medicine, a Ph.D. in Genetics from the University of Cambridge, and a BS in Biochemistry and Chemistry from Clemson University. He also completed the INNoVATE Program in Biotechnology Entrepreneurship at The Johns Hopkins University - Carey Business School. Dr. Ziats is board certified by the American Board of Internal Medicine.
There are 9 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 14,735 times.
Genetic counselors help patients navigate the medical, psychological, and hereditary aspects of their genetic backgrounds. Most people who seek their guidance do so because they are planning to have children and want to understand the likelihood of having a baby with a genetic disorder or birth defect. If you are thinking of starting a family (or if you or your partner are already pregnant), and if you have concerns about the risk of genetic disorders, you may wonder if genetic counseling is right for you.
Steps
Understanding Genetic Counseling
-
1Decide to see a Clinical Geneticist or a Genetic Counselor. Clinical Geneticists are MD physicians who are trained in diagnosing and educating families in genetic conditions. They have spent 4 years in college, 4 years in medical school, at least 1 year doing a general residency in a field like Internal Medicine or Pediatrics, and another 2 years doing a fellowship in Medical Genetics.. Genetic Counselors are trained individuals who help families cope with genetic disorders. They have completed 4 years of college and at least 2 years of masters degree in genetic counseling.
-
2Research the role of the genetic counselor. Genetic counselors are not medical doctors; rather, they hold Master of Science degrees in genetic counseling.[1] Their services are meant to supplement – not take the place of – the advice of your obstetrician or primary care physician. They offer information and support, not direct medical care.
- If you do see a genetic counselor and he or she identifies specific potential problems, you will likely be referred to a medical geneticist, a medical doctor with advanced training in genetics.[2] This person will be qualified to offer medical care.
-
3Know what kinds of services to expect. In general, genetic counselors will help you assess your risk of genetic disorders, weigh the pros and cons of genetic testing, and understand the results of those tests, if you take them. They will also help gather information about your family history of disease. Using whatever information they can gather, they will explain and help you evaluate all of your reproductive options. They will also offer support as you navigate these options.[3]
- Genetic counselors will frequently be unable to tell you for certain whether your child will have a genetic disorder or birth defect. They are often able only to give you a better sense of the probability.
- Genetic counselors will not tell you which reproductive options you should choose. They will not say, for example, that you should not start a family (or that you should), and they will not tell you to have an abortion (or advise against one). They will simply make sure you have as much information as possible so that you can make those decisions yourself.
Making the Decision to Seek Genetic Counseling
-
1Evaluate your emotions honestly. Even if you have one or more of the risk factors for genetic disorders, or if your doctor recommends genetic counseling, you may still feel apprehensive about taking that step. That's perfectly normal, and it's worth stopping to examine your feelings. Will more information make you feel more confident or more anxious? Will having more information help you feel more prepared for the most likely outcomes of your pregnancy?
- Some pregnant women and their partners are opposed to abortion in all circumstances.[4] They know they would continue with a pregnancy no matter what information they might get from a genetic counselor, so they worry that any “bad news” they do receive would only add unnecessary anxiety. If this is your position, that's absolutely valid, but understand that genetic counselors will never pressure you to terminate your pregnancy. Further, the information they give you might help you prepare more effectively for the possibility of having a baby with a genetic disorder or birth defect.
-
2Talk openly with your doctor. Your doctor should be able to offer you some basic advice about the pros and cons of genetic counseling for someone in your particular situation. Raise any concerns you have with your doctor first, and see what he or she recommends.
-
3Discuss genetic counseling with your partner.[5] If you have a spouse or partner, take the time to have a serious conversation about the possibility of genetic counseling. Good communication will help you make a decision together; it will also set the right tone for handling any issues that do come up.
Considering Your Medical Risks
-
1Look into your family history. Most people do not need to seek genetic counseling, but if you have a family history of genetic disorders or birth defects (or your partner does), you should consider it. Some genetic disorders are hereditary, and a genetic counselor can help you understand the likelihood of passing these disorders on to any children you might have.
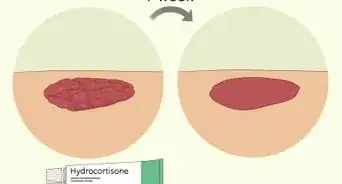
- Some of the more common hereditary genetic disorders include cystic fibrosis, and sickle cell anemia. If any of these disorders appear in your family history (or your partner's), you are an excellent candidate for genetic counseling.
-
2Consider your reproductive history. If you or your partner have a history of multiple miscarriages, a child who died in early infancy, or an existing child with a genetic disorder or birth defect, you might consider seeing a genetic counselor before trying to have another baby.[6]
-
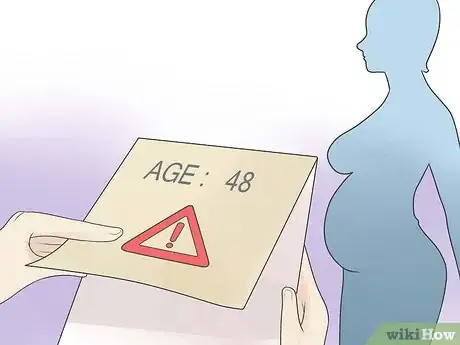
3Factor in maternal age. If you are pregnant (or want to become pregnant) after your mid-thirties, you might be a good candidate for genetic counseling. After age 35, the risk of having a baby with a birth defect increases significantly: at age 35, the overall chance is 1 in 178, while by age 48, the chance is 1 in 8.[7]
-
4Think about risks related to your ethnicity. Some genetic disorders are more common among particular ethnic groups. For example, sickle cell anemia is more common among people of African descent, thalassemia is more common among people of eastern European and Middle-Eastern descent, and Tay-Sachs disease is more common among Ashkenazi Jews.[8]
-
5Consider any exposure to potentially harmful substances. If you've had chemotherapy or been exposed to radiation or toxic chemicals, your risk increases. You should discuss the potential consequences with your doctor and consider pursuing genetic counseling.
-
6Note the results of any prenatal tests. If you or your partner are already pregnant, you will probably have a number of routine prenatal tests: every pregnant woman will have blood work, urinalysis, and ultrasounds performed, and some will have additional tests recommended by their doctors.[9] If your doctor thinks the results of any of these tests indicate a higher than normal possibility of genetic disease, he or she may suggest you consider genetic counseling.
References
- ↑ http://www.geneticdiseasefoundation.org/genetic-diseases/
- ↑ http://www.nlm.nih.gov/medlineplus/geneticcounseling.html
- ↑ https://www.mayoclinic.org/tests-procedures/genetic-testing/about/pac-20384827
- ↑ http://kidshealth.org/parent/system/medical/genetic_counseling.html
- ↑ http://www.genome.gov/19016905
- ↑ http://www.medicinenet.com/genetic_disease/index.htm
- ↑ https://www.stanfordchildrens.org/en/topic/default?id=when-to-seek-genetic-counseling-90-P02118
- ↑ https://medlineplus.gov/genetics/understanding/inheritance/ethnicgroup/
- ↑ http://www.healthline.com/health/pregnancy/risk-factors